Nebula Genomics DNA Report for Hernias
Are hernias genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
What is a hernia?
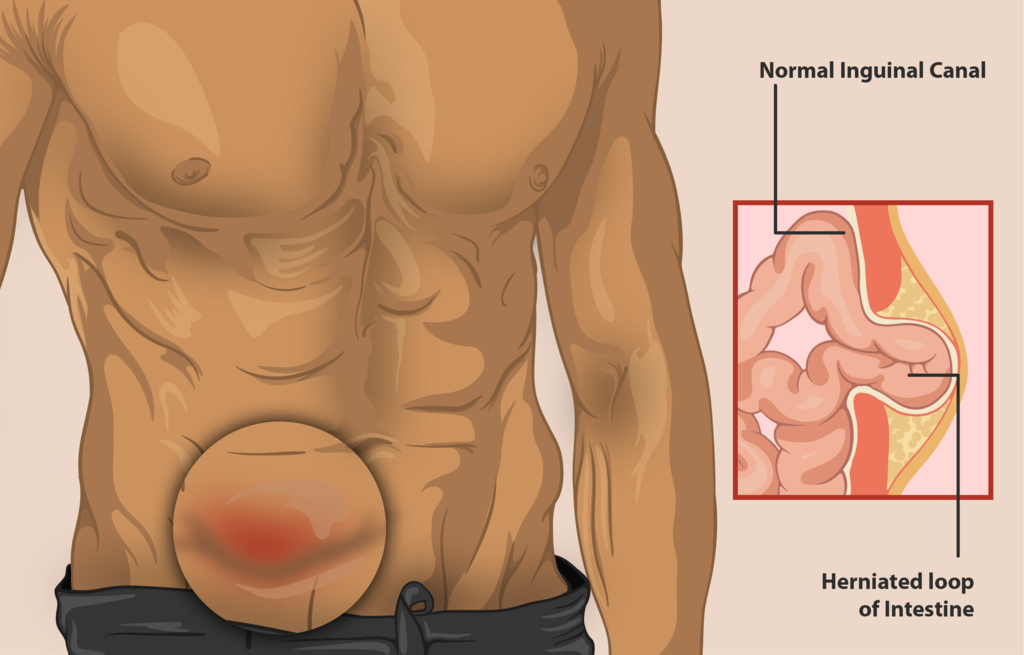
A hernia is a condition that occurs when an internal organ or tissue protrudes through a weakened area or opening in the body. They commonly occur in the abdominal area, also known as ventral hernias, but can also develop in the groin, upper thigh, or belly button.
Hernias are a common medical condition that can affect anyone, regardless of age or gender. They can cause discomfort, pain, and even life-threatening complications if left untreated.
Things like heavy lifting or straining may bring on the condition, especially if someone has weak abdominal muscles.
Types
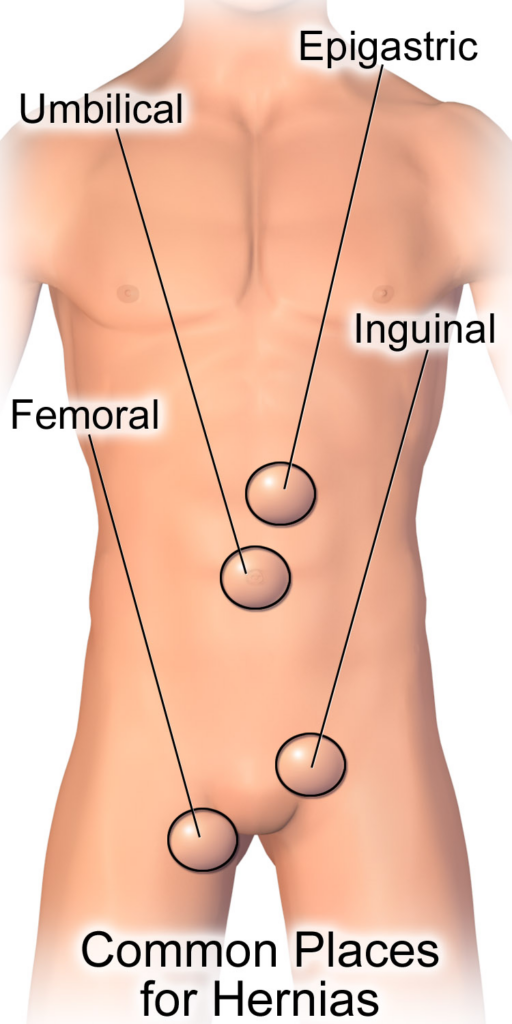
There are several types of hernias based on where the condition occurs:
- Inguinal: Occur when a part of the intestine protrudes through the groin area in the inguinal canal. This is the most common type.
- Femoral: Occur in the femoral canal in the upper thigh
- Umbilical: Occur in the abdominal wall near the belly button
- Incisional: Occur when a part of the intestine protrudes through a weakened area of the abdominal wall at the site of a previous surgery
- Hiatal: Occur in the diaphragm into the chest cavity
- Epigastric: Occur when tissue pokes through a gap in the abdominal wall between the breastbone and the belly button
Are Hernias Genetic?
The condition can develop for various reasons, including injury and lifestyle choices. Therefore, the role of genetic factors related to hernias remains an important area of research. Experts agree that the condition is not hereditary. That is, it cannot be passed from parent to child.
However, some studies suggest that genetic variants may predispose an individual and you may be at higher risk if you have a family history of inguinal hernias.
Experts have implicated several genes in development, including those responsible for collagen production, an essential protein for maintaining abdominal wall strength.
COL1A1 and COL1A2: These genes encode the type I collagen protein, a major component of connective tissue.
MMP2 and MMP9: These genes encode enzymes that are involved in the breakdown of collagen.
TGF-β1: This gene encodes a growth factor involved in tissue repair and regeneration.
FBN1: This gene encodes a protein called fibrillin-1, which is involved in forming connective tissue. This variant is associated with congenital diaphragmatic hernia (CDH), a life threatening birth defect in which the muscle that separates the chest from abdomen fails to close during fetal development. A study titled “Molecular genetics of congenital diaphragmatic defects” describes genes potentially involved in congenital diaphragmatic hernia (CDH), a severe birth defect accompanied by defects in several organs.
Hernia Research
Mutations in these genes can lead to weakened connective tissue, which may increase the risk of development. One study published in the Journal of Surgical Research found that there may be a genetic component to developing inguinal hernias. The study analyzed data from over 6,000 pairs of male twins and found heritability estimated at around 38%. However, the study also found that environmental factors played a significant role, suggesting that genetics alone cannot explain the condition.
Another study published in the Journal of Pediatric Surgery found that there may be a genetic component to the development of umbilical hernias in children. The study analyzed data from over 500 children with the condition and found a significant familial clustering. However, the study also noted that other factors, such as obesity and birth weight, may also play a role.
Epidemiology
Hernias are a common medical condition, with an estimated 20 million hernia repairs performed yearly worldwide, 700,000 in the United States. While anyone can develop the condition, it is more common in certain populations, including older adults and men.
Inguinal hernias are the most common type, accounting for up to 75%. They are also more common in men than women, with men being eight times more likely to develop them than women. The incidence increases after age 40.
Femoral hernias are more common in women than men, with women being four times more likely to develop them than men. They are also more common in people over the age 50.
Umbilical hernias occur more often in women than men and are often seen in newborns and infants. While most will resolve independently, some may require surgical repair if they do not improve by age four.
Incisional hernias occur due to previous abdominal surgery and can occur in up to 30% of patients who have had abdominal surgery. The risk increases with each subsequent abdominal surgery.
Symptoms
Hernia symptoms vary depending on the type and severity of the condition. Common symptoms of hernias include:
- A bulge or swelling in the affected area
- Pain or discomfort, especially when lifting, coughing, or straining
- Burning or aching in the affected area
- A feeling of heaviness or pressure in the affected area
- Weakness or pressure in the affected area
- Nausea or vomiting (in the case of a hiatal hernia)
Sometimes they may not cause symptoms, especially in the condition’s early stages. Patients are recommended to seek medical attention if a hernia bulge turns red, purple or dark (indications of a strangulated hernia that cuts off blood flow) or if it becomes painful or noticeable.
Causes
Hernias can develop as a result of a variety of risk factors, including:
Weakness in the abdominal wall: A weakness in the abdominal wall can allow organs or tissue to protrude through. This weakness can be congenital (present at birth) or acquired through injury or previous surgery. Overall, this feature increases the risk of developing hernias from the following:
Straining: Activities that involve lifting heavy objects, coughing, or straining during bowel movements that can increase the pressure inside the abdomen.
Obesity: Excess weight that increases pressure on the abdominal wall.
Chronic constipation: Straining during bowel movements can increase pressure on the abdominal wall.
Aging: As people age, abdominal muscles may weaken or deteriorate.
Pregnancy: The increased pressure on the abdominal wall during pregnancy can increase the risk of hernia development.
Diagnosis
Diagnosis typically involves a physical exam and medical history. The affected area is examined for signs of swelling or bulging. Doctors may also ask the patient to cough or strain to make the condition more visible.

Doctors may order imaging tests to confirm the diagnosis or determine the hernia’s size and location. Imaging tests include ultrasounds, CT scans, and MRIs.
Treatment
Doctors may recommend watchful waiting in some cases, especially for small, asymptomatic cases. If the condition is enlarged or painful, treatment typically involves surgical repair.
Hernia surgery involves inguinal hernia repair and reinforcing the area with a mesh patch. The two surgical options are either open or laparoscopic repair.
Open surgery involves making an incision near the groin and manually pushing the tissue back into the abdomen. The surgeon will close the incision site and reinforce the area.
Laparoscopic repair involves making several small incisions in the abdomen and using a tiny camera with specialized laparoscopic instruments to repair the condition.
In general, laparoscopic surgery is associated with shorter recovery times and less pain than open repair. However, not all hernias are suitable for laparoscopic repair. The optimal surgical approach will depend on various factors, including the size and location of the protruding tissue and the patient’s overall health. Common questions to discuss with a doctor before surgery include non-surgical option, risks, and treatment options.
Long-term benefits for both surgeries appear to be the same.
In addition to surgical repair, several lifestyle changes can help to reduce the risk of development or recurrence. These include:
- Maintaining a healthy weight
- Avoiding activities that involve heavy lifting or straining
- Treating chronic constipation
- Wearing supportive garments, such as a hernia belt, if recommended by a healthcare provider
If you liked this article, you should check out our other posts in the Nebula Research Library!
August 9, 2023
