Nebula Genomics DNA Report for Testicular Cancer
Is testicular cancer genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
What is Testicular Cancer?
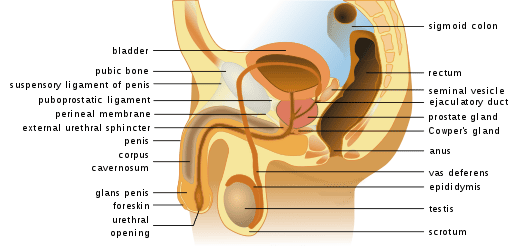
Testicular cancer occurs in the testicles, which are part of the male reproductive system located in the scrotum. They produce sperm and the hormone testosterone.
The condition usually starts as a painless lump or swelling in one or both testicles. Often, the testicular germ cell tumor will spread to other parts of the body.
Other symptoms may include a dull ache or pain in the testicles or scrotum, a feeling of heaviness in the scrotum, or a change in the size or shape of the testicles. Testicular cancer is a rare cancer type and it is highly treatable, especially if caught early. Treatment options may include surgery, radiation therapy, chemotherapy, or a combination.
It is the most common cancer in the United States and Europe in males between the ages of 15 and 45. However, it is also highly treatable, with a nearly 98% cure rate.
Is Testicular Cancer Genetic?
In most cases, experts do not consider the condition genetic or inherited. However, some studies have suggested that certain genetic factors may increase a person’s risk of developing testicular cancer.
For example, men with a family history of testicular cancer may have a higher risk of developing the disease. Additionally, experts have linked genetic disorders such as Klinefelter syndrome, which affects the sex chromosomes, to an increased risk of testicular cancer. However, most testicular cancers occur sporadically and are not associated with genetic or inherited factors. Other risk factors include age, race, and personal history of testicular cancer.
Research suggests that specific genetic alterations can increase testicular cancer risk. Patients can inherit or acquire these genetic changes during a lifetime. Here are some genes associated with developing cancer:
KIT: This gene produces a protein that helps regulate cell growth and division. It is critical in normal germ cell development.
KRAS: This oncogene helps cell signaling pathways that regulate cell proliferation, apoptosis, migration, and differentiation.
TP53: This tumor suppressor gene helps prevent cells from growing and dividing too quickly or in an uncontrolled way.
CDKN2A: This gene produces proteins that regulate cell growth and division.
PTEN: This tumor suppressor gene helps regulate cell growth and division.
It’s important to note that these genetic factors are associated with only a small percentage of testicular cancer cancers. Most occur sporadically and are unrelated to genetic or inherited factors.
Epidemiology
Testicular cancer is a relatively rare form, accounting for only about 1% of all cancers in males. However, it is the most common type of cancer in young men between 15 and 35. Testicular yolk sac tumor is the most common childhood testicular tumor.
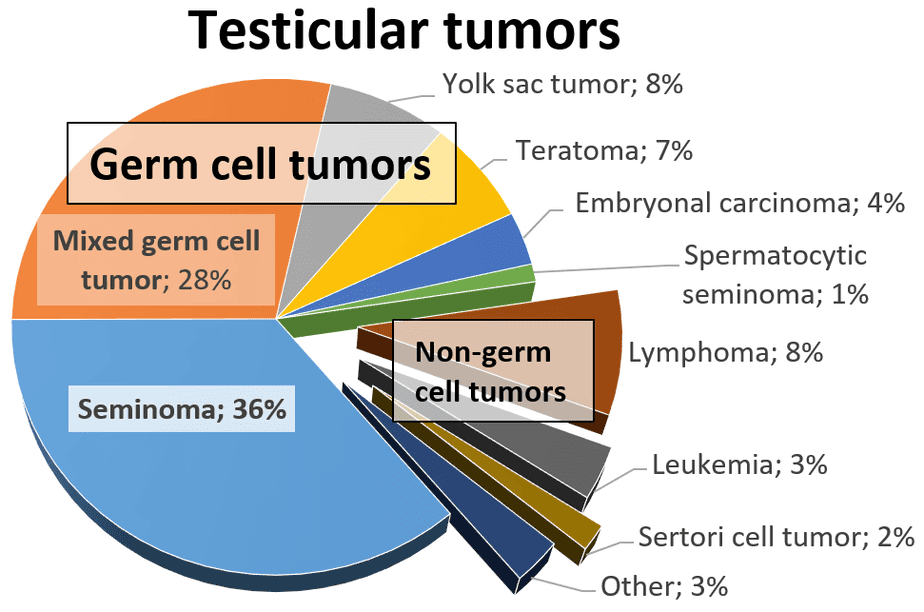
According to the American Cancer Society, doctors will diagnose approximately 9,190 new cases of testicular cancer and report 470 deaths in the United States in 2023. The incidence rate has been rising for several decades in the U.S. and other nations, particularly in seminomas, cancer that originates in male germ cells, without any known cause. Nonetheless, the rate of increase has recently slowed.
Fortunately, testicular cancer has a high cure rate, resulting in a low lifetime mortality risk, with only about one in 5,000 dying from this disease and a 5-year relative survival rate of around 95%.
Testicular cancer rates vary widely worldwide, with the highest incidence in Northern and Western Europe, Australia, New Zealand, and North America. In contrast, the lowest incidence rates are found in Asia and Africa. The reasons for these geographic differences are unclear, but they may be related to differences in lifestyle, environmental, or genetic factors.
Several risk factors have been associated with an increased risk of testicular cancer, such as age, race/ethnicity, family history of the disease, cryptorchidism, HIV infection, and body size.
Symptoms
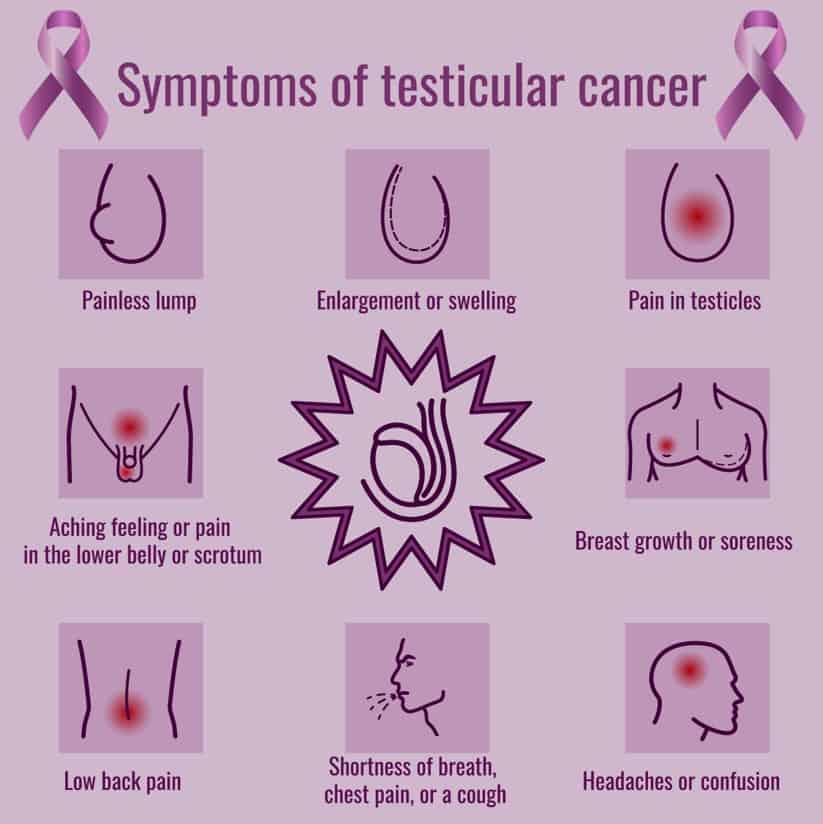
Testicular cancer may not always cause noticeable symptoms, especially in its early stages. However, some patients may experience one or more of the following symptoms of testicular cancer:
- A lump or swelling in either testicle, which may or may not be painful
- A feeling of heaviness or discomfort in the scrotum
- A dull ache or pain in the lower abdomen or groin
- A sudden buildup of fluid in the scrotum (hydrocele)
- Enlargement or tenderness of the breasts (gynecomastia)
- Back pain
It’s important to note that other conditions may cause these symptoms. For example, a lump or swelling in the testicle could indicate an infection or a benign (non-cancerous) cyst. However, a healthcare professional should evaluate any unusual symptoms in the testicles to determine the cause and whether the patients needs further tests.
Causes
Experts do not know the exact cause of testicular cancer. Like any cancer, it results when cells undergo DNA changes that prevent cell death and disrupt the natural process of controlling cell division. This causes a buildup of cells that eventually form a tumor. Nearly all testicular cancers start in the germ cells.
Therea are several risk factors for testicular cancer that can increase the chance of developing the disease. These include:
Age and sex: Testicular cancer is most common in young and middle-aged males between 15 and 44.
Cryptorchidism: Testicles typically move down into the scrotum within at birth or during the first year of life. Males born with undescended testicles (cryptorchidism) have an increased risk of testicular cancer.
Family history: Patients with a family history of testicular cancer may be at increased risk.
Race/ethnicity: White males have a higher risk of testicular cancer than those of other races or ethnicities. Studies have shown that Asian Americans have lower incidence of the disease but typically a higher stage at diagnosis.
Klinefelter syndrome: Patients with Klinefelter syndrome, a genetic condition resulting in an extra X chromosome, have an increased risk.
Personal history: People with testicular cancer in one testicle have an increased risk of developing the disease in the other one.
HIV infection: Those with HIV/AIDS have an increased risk.
Environmental factors: Exposure to certain chemicals, such as pesticides, have been linked to an increased risk of testicular cancer.
It’s important to note that having one or more of these risk factors does not necessarily mean that a person will develop testicular cancer, and many people with the disease have no known risk factors. More research is needed to understand the causes of testicular cancer fully.
Diagnosis
A patient may discover swelling or a lump during a self-exam or a standard testicular cancer screening. If you do notice something, it’s important to consult a professional. A doctor will take several steps to diagnose testicular cancer, including a physical exam. If they suspect the condition, they will examine the testicles and scrotum for lumps, swelling, or other abnormalities.
If a doctor finds something during the exam, they will most likely order an ultrasound to take pictures of the of the scrotum and testicles. These images will give the doctor a better idea of whether the lump is cancerous or not by where it is and what it looks like.
Additionally, blood tests can measure levels of proteins produced by testicular cancer cells. High levels of these proteins may indicate the presence of testicular cancer.
If the doctor thinks a lump may be cancerous, a biopsy may be necessary to confirm the diagnosis of testicular cancer. During a biopsy, a doctor removes a small tissue sample from the testicle and examines it under a microscope. They may also perform surgery to remove the testicle.
Once an expert diagnoses testicular cancer, they may perform additional tests to determine the cancer type and stage (whether it has spread to other body parts).
The two most common types of testicular cancer are seminoma and nonseminoma. The former tends to appear at older age and spread slowly while the latter more often occurs at a younger age and spreads more quickly.
Stages
Doctors usually describe testicular cancer stages as 0 to 3. In most cases stages 0 and 1 (the early stages, also called germ cell neoplasia in situ) indicate that the cancer is restricted to the testicle and surrounding areas. On the other hand, stage 2 means it has spread to the lymph nodes and stage 3 suggests it has spread to other parts of the body.
Additional tests may include CT, MRI, and PET scans. The stage of cancer helps determine the best course of treatment.
Treatment
Treatments depend on several factors, including the type and stage of cancer, the patient’s age, overall health, and whether the cancer has spread to other body parts. The main treatments for testicular cancer include;
The primary treatment for testicular cancer is removing the affected testicle (radical inguinal orchiectomy). The surgeon makes an incision in the groin and removes the entire testicle. If the cancer hasn’t spread, this may be the only treatment needed.
In some cases, patients may need additional surgery (retroperitoneal lymph node dissection) to remove lymph nodes in the abdomen. This occurs more often in the nonseminoma type.
Radiation therapy uses high-energy radiation to kill cancer cells. It is sometimes used after surgery to kill any remaining cancer cells or as the primary treatment for certain types of testicular cancer, usually the seminoma type.
Chemotherapy uses drugs to kill cancer cells. It is often used with surgery and radiation therapy or as the primary treatment for advanced or aggressive testicular cancers.
For certain types, management (close monitoring without immediate treatment) may be an option. This may involve regular exams, blood tests, and imaging studies to monitor cancer and detect any changes.
In rare cases, a stem cell transplant may be recommended for advanced testicular cancer that has not responded to other treatments. The overall prognosis for testicular cancer is very good, with a treatment success rate of more than 95%. If treated early, the cure rate increases to 98%.
If you liked this article, you should check out our other posts in the Nebula Research Library!
June 2, 2023
