Nebula Genomics DNA Report for Gallstones
Are gallstones genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
What are Gallstones?
Gallstones typically form when there is an imbalance in the substances that make up bile, such as cholesterol, bile salts, and bilirubin. They are hardened deposits of digestive fluid formed in the gallbladder, a small organ beneath the liver that stores bile.
When these substances are not properly balanced, they can crystallize and form gallstones. According to the Mayo Clinic, the composition of gallstones can vary, with the two main types being cholesterol and pigment stones.

Cholesterol stones are the most common type and are typically yellow-green. They form when there is an excess of cholesterol in the bile, which does not contain enough bile salts to dissolve the cholesterol effectively.
Pigment stones, on the other hand, are composed of bilirubin, a pigment that the body produces when it breaks down red blood cells. These stones are usually smaller and darker, ranging from brown to black. Pigment stones can form when there is an excessive amount of bilirubin in the bile, such as in cases of liver disease or certain blood disorders.
Gallstones can be as small as a grain of sand or as large as golf balls. Most cases of the conditions do not cause symptoms or require treatment. However, sometimes gallstones travel from their place of origin and cause problems that require intervention.
Are Gallstones Genetic?
Genetic factors play a role in gallstone development. From a heredity viewpoint, Native Americans have the highest rates of gallstones in the United States as they have genes that raise the cholesterol amounts in their bile. Mexican Americans are also at a higher risk.
Some studies suggest that genetic factors are responsible for at least 30% of symptomatic gallstone disease.
Experts have identified several genes involved in cholesterol metabolism and bile transport as associated with a genetic predisposition towards gallstone formation.
When considering cholesterol gallstones, scientists have linked variations in ABCG5/8 and Lith genes to differences in cholesterol metabolism that appear to play a role in gallstone formation. On the other hand, variations in the UGT1A1 gene are associated with an increased risk of pigment stone formation due to impaired bilirubin metabolism.
Research continues to be performed in this field. A paper published in 2021 identified 46 new genes that appear to increase gallstone risk.
It’s important to note that these genetic variations contribute to an increased susceptibility to gallstones, but they do not guarantee their development. Other factors such as diet, obesity, and medical conditions interact with genetics to influence gallstone formation. Rapid weight loss can trigger gallstones for the same reason as obesity in that it alters the balance of things like bile acids that affect gallbladder function.
Epidemiology
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), gallstones affect approximately 10-15% of adults in the United States. Women are at a higher risk, having a prevalence twice as high as men. Producing additional estrogen, such as during pregnancy or while taking birth control pills, may make the condition more likely.
The risk of developing gallstones increases with age and family history. Additionally, and the condition is more common among individuals who are overweight or obese.
Symptoms
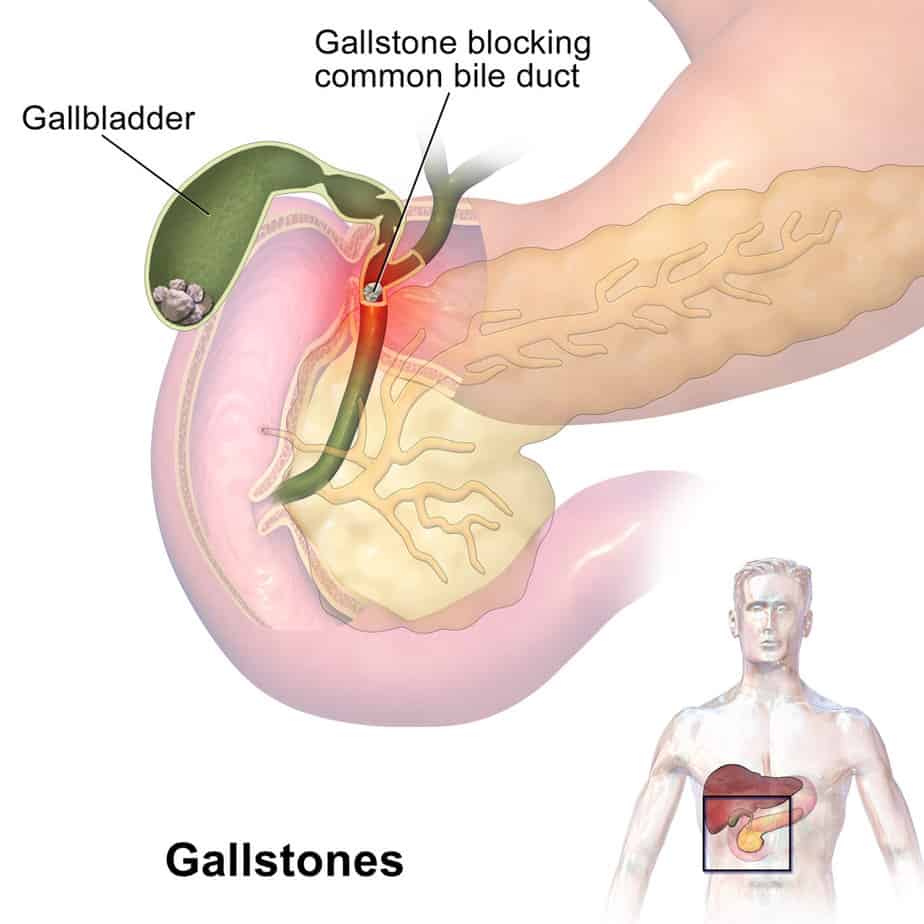
According to Mayo Clinic, gallstones are usually asymptomatic, but may cause problems if one lodges in the common bile duct and block the gallbladder, liver, or pancreas.
Symptoms of gallstones often include pain with nausea and vomiting. Patients typically feel the pain, caused by a gallbladder attack or biliary colic, in the upper right or center abdomen and may radiate to the back or there may be pain in the right shoulder blade. People with gallstones may have pain ranging from mild to severe and may be intermittent or persistent up to a few hours. Those who have experienced one gallbladder attack most often have more.
Patients may feel more pain after eating a fatty meal because these foods stimulate the gallbladder to release bile, which aggravates the condition.
Other signs include jaundice, dark urine, clay-colored stools, and fever and chills. Patients should see a doctor shortly after experiencing a suspected gallbladder attack as these symptoms may indicate a serious infection or inflammation of the gallbladder, liver, or pancreas.
Alternatively, they could be caused by appendicitis, ulcers, pancreatitis, or gastroesophageal reflux disease, which should also be checked by a healthcare professional.
Although symptoms will usually dissipate once the gallstone dislodges from the bile duct, a stuck gallstone can be fatal if left untreated.
Causes
The causes of gallstones vary. There are two primary types: those made of cholesterol (cholesterol stones) and those made of bilirubin (pigment stones).
Cholesterol stones: Bile salts help break down cholesterol. When the liver excretes higher cholesterol levels than the bile can dissolve, gallstones form from the excess cholesterol.
Pigment stones: The body makes bilirubin when it breaks down red blood cells. Liver cirrhosis or certain blood disorders such as anemia can disrupt normal bilirubin metabolism, leading to an excess that forms stones. Other genetic conditions, such as hereditary spherocytosis, or infections in the bile ducts, can predispose individuals to form pigment stones by affecting the breakdown of red blood cells and bilirubin metabolism.
Additionally, if the gallbladder does not empty bile efficiently or often enough, bile can become concentrated, contributing to formation.
Obesity and certain kinds of diet (e.g., high-fat, low-fiber, and high-cholesterol) are also risk factors. People with diabetes tend to have high levels of fatty acids, which can increase their risk for gallstones.
Diagnosis
A doctor will usually perform a physical exam and ask about a patient’s family history with gallstones. They will also examine the patient for abdominal pain. Healthcare professionals use various methods, usually imaging tests, to definitively diagnose gallstones and their related complications.
The most common test is an abdominal ultrasound. This imaging uses sound waves to visualize the gallbladder and check for the presence of gallstones. Doctors usually perform an ultrasound non-invasively on the top of the abdomen.
Alternatively, they can use an endoscopic ultrasound (EUS) to identify stones too small to pick up with a traditional ultrasound. This procedure involves passing a thin tube with an ultrasound device on its end through the mouth and digestive tract.

A doctor may use a cholescintigraphy (HIDA scan) to diagnose abnormal gallbladder contractions or bild duct blockages. It involves the injection of a radioactive tracer, which is taken up by the liver and excreted into the bile. The doctor tracks the tracer’s movement through the liver, bile ducts, and gallbladder to assess the functioning of the gallbladder and detect the blockages to the flow of bile.
Other imaging tests, such as CT scans and MRI may also be used.
Finally, a more invasive imaging test is endoscopic retrograde cholangiopancreatography (ERCP). This procedure combines endoscopy and X-rays to evaluate the bile ducts. It can help identify and then remove gallstones lodged in the bile ducts.
Doctors may also recommend blood tests that can help identify signs of infection, inflammation, or blockage in the bile ducts. Elevated levels of liver enzymes or bilirubin may indicate gallstone-related complications.
Treatment
The treatment of gallstones depends on several factors, including symptoms, the size and number of gallstones, and the risk of complications.
Asymptomatic gallstones that do not cause discomfort or complications usually do not require treatment. Doctors may recommend that the patient be alert for new or worsening symptoms, such as intesifying abdominal pain. If the issues persist, treatment may be necessary.
Surgery
Surgical removal of the gallbladder (cholecystectomy) is the most common and effective treatment. The procedure involves removing the gallbladder. Patients do not need this organ to live and those who undergo this surgery typically lead normal lives. There may be some diarrhea which is usually temporary.
Laparoscopic cholecystectomy is a minimally invasive procedure that involves making several small incisions in the abdomen and inserting a thin, flexible tube equipped with a camera and surgical instruments. The surgeon uses these instruments to visualize the gallbladder and surrounding structures on a monitor and safely remove the gallbladder. Laparoscopic cholecystectomy generally results in less pain, faster recovery, and fewer complications than open surgery.
On the other hand, open cholecystectomy involves making a larger incision in the abdomen to access and remove the gallbladder directly. Open surgery is typically reserved for complex cases, such as severe inflammation, scarring, or complications.
Both laparoscopic and open cholecystectomy procedures are generally safe and have high success rates. After the gallbladder removal, bile flows directly from the liver to the small intestine, allowing digestion to continue normally.
Medications
Medications may be prescribed to dissolve small cholesterol gallstones, particularly those not causing symptoms. These medications, known as oral bile acid pills, gradually dissolve the gallstones over months or years. However, this treatment approach is less common than surgical interventions and is generally less effective.
If you liked this article, you should check out our other posts in the Nebula Research Library!
July 7, 2023
