Table of contents
Nebula Genomics DNA Report for GERD
Is GERD genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Introduction
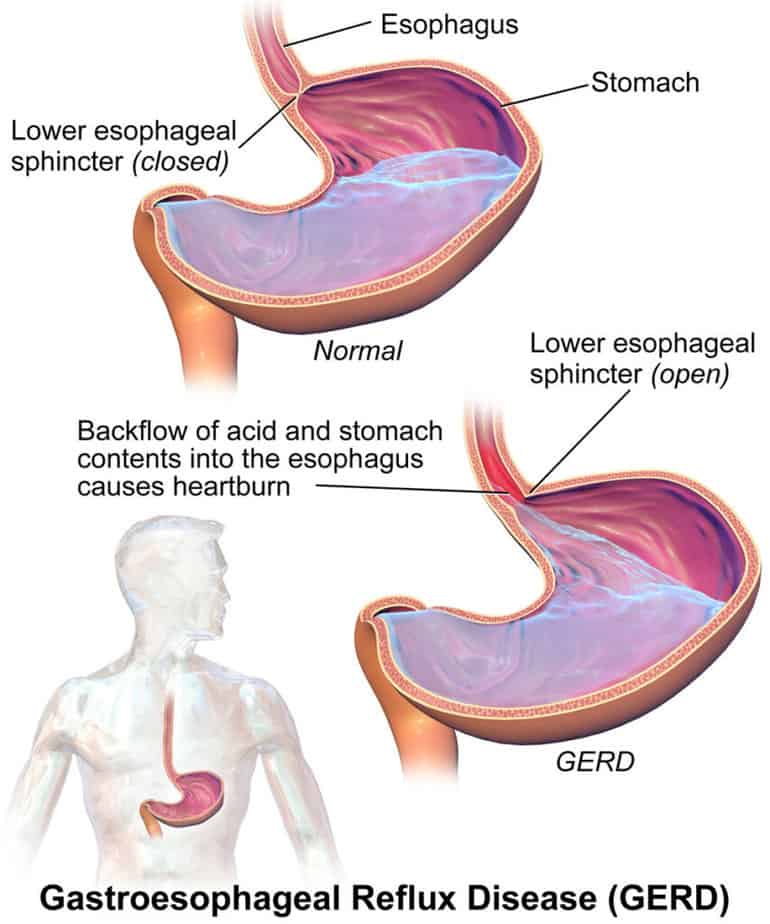
Gastroesophageal reflux disease (GERD) is a chronic condition in which stomach contents come back into the mouth and esophagus, resulting in uncomfortable symptoms such as he taste of acid in the back of the mouth, heartburn, bad breath, chest pain, regurgitation, breathing problems, and wearing away of the teeth.
Everyone will usually experience some heartburn or acid reflux (GER) in their lifetime and doctors consider perfectly normal. They diagnose the condition as GERD when occasional acid reflux occurs more than twice a week over a period of several weeks, doesn’t respond to heartburn medications, and interferes with daily life.
Risk factors for developing the condition include obesity, pregnancy, smoking, hiatal hernia, and taking certain medicines. The reflux occurs when the opening between the stomach and the esophagus does not close properly and acid backwash returns after eating. Usually, a doctor can diagnose and treat the condition.
The two most common GERD treatment options are lifestyle changes and medications. In some severe cases, doctors may recommend surgery. If left untreated, it can lead to more serious conditions.
Is GERD Genetic?
When people think about heartburn and GERD, they usually associate it with lifestyle factors, especially diet. It is true that these factors can contribute to instances of heartburn and development of the disease.
However, studies have shown that GERD and GER also have a strong genetic component. A 2018 article published in the World Journal of Clinical Cases suggested that identical and fraternal twin studies demonstrated a 31% heritability of the disease.
An earlier study published in Gut noted that among over 2,000 sets of identical twins, one twin was 1.5 times more likely to develop GERD if the other twin also had the condition.
Experts believe GERD to be a complex disease, with multiple genetic factors contributing to the disease occurrence and development. Some specific genes such as FOXF1, MHC, CCND1, anti-inflammatory cytokine and DNA repair genes are most likely involved.
Epidemiology
GERD is a very common condition in the general population. In 2014, a review study published the prevalence of GERD in the global population. The authors reported 18-28% of people in North America, 9-26% in Europe, 3-8% in East Asia, 9-33% in the Middle East, 12% in Australia, and 23% in South Africa suffer from GERD.
It can be difficult to get an exact estimate of the number of people with the disease since not everyone who has the symptoms has them to an extent of diagnosis. Many people will self-treat occasional symptoms with over-the-counter medications. Typically, the threshold for disease classification is damage to the tissues where the acid has moved from the stomach back to the esophagus.
Symptoms
The symptoms can vary greatly from person to person. Some of the most common signs, as noted by Cleveland Clinic, include:
- Heartburn (a painful, burning feeling rising from the lower tip of your breastbone toward your throat)
- Regurgitation (food comes back into your mouth from the esophagus)
Depending on the amount of acid regurgitated, other common symptoms may include:
- The feeling of food caught in your throat
- Coughing
- Chest pain
- Trouble swallowing
- Vomiting
- Sore throat and hoarseness

You may also experience symptoms that are signs of complications from a chronic disease:
- chest pain
- loss of appetite
- persistent vomiting
- problems swallowing or pain while swallowing
- signs of bleeding in the digestive tract, such as
- vomit that contains blood or looks like coffee grounds
- stool that contains blood or looks black and tarry
- unexplained weight loss
Children and infants display unique symptoms:
- Frequent small vomiting episodes
- Excessive crying, not wanting to eat (in babies and infants)
- Other respiratory (breathing) difficulties
- Frequent sour taste of acid, especially when lying down
- Hoarse throat
- Feeling of choking that may wake the child up
- Bad breath
- Difficulty sleeping after eating, especially in infants
Overall, patients with GERD are more likely to develop other serious health problems such as esophageal cancer or an esophageal stricture (narrowing of the esophagus).
Causes
The lower esophageal sphincter (LES) usually prevents stomach contents from coming back into the mouth by closing after food reaches the stomach. GER and GERD occurs when this sphincter becomes weak or relaxes when it shouldn’t. Temporary occurrences of GER occur to most people at some point in their life. In particular, environmental factors such as stressful situations and certain types of food such as those made with dairy, spice, or fried foods tend to cause GER.
Patients are at higher risk of developing the disease if they are obese, smoke, or are pregnant.
Some medications can also cause GERD including:
- Benzodiazepines (sedatives to induce sleep)
- Calcium channel blockers (used to treat high blood pressure)
- Certain asthma medicines
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Certain antidepressants
A hiatal hernia can also play a role in increasing the chance of getting GERD or make GERD symptoms worse. This condition occurs when the upper part of the diaphragm bulges into the stomach, altering normal food uptake.
Diagnosis
In most cases, your doctor can diagnose GERD by a physical examination and the description of your symptoms. They can often recommend medication and lifestyle changes without additional tests. You should always consult your doctor for medical advice, diagnosis, or treatment.
Sometimes a doctor will want to confirm your diagnosis if you appear to have a complication of GERD, if the symptoms appear to be similar to another health condition, or if symptoms don’t improve after medication and lifestyle changes. A gastroenterologist is a specialist that will often diagnose and treat the condition.
Upper Gastrointestinal (GI) endoscopy: During this procedure, the doctor will place an endoscope (a thin, flexible tube with a light and camera on the end) through the throat and into the upper GI tract. It can check for signs of the disease such as inflammation and can collect a sample of tissue as a biopsy for more serious conditions like Barrett’s esophagus and esophageal cancer.

Esophageal acid (pH) probe test: An esophageal pH test is the most accurate procedure to detect stomach acid in the esophagus. A monitor is placed in the esophagus that can tell how much and for how long stomach acid is regurgitated. The doctor can attach the monitor through a tube that enters through the nose (catheter monitoring) or it can be a small capsule that they insert in the esophagus during an endoscopy (capsule monitoring). A common example is the 48 Hour Bravo Esophageal pH Test.
Esophageal manometry: This is a test that measures how well your esophageal muscles contract when you swallow.
X-ray: This is an imaging technique that takes a picture of your esophagus, stomach and upper intestine.
Treatment
As noted by the National Institute of Diabetes and Digestive and Kidney Diseases, the most common way to treat GERD is through lifestyle changes and over-the-counter medications. Additional information can be found on their website. You should also talk to your doctor before making changes.
Lifestyle changes
- Losing weight
- Quitting smoking
- Changing eating habits and diet
Over-the-counter medications
Antacids: These medications, designed to neutralize stomach acid, provide nearly immediate relief of the symptoms. However, they do not heal damage, such as inflammation in the esophagus, caused by the disease. Overuse of these medications can cause diarrhea and some kidney problems. Examples include Mylanta, Rolaids and Tums.
H2 blockers: These will reduce acid production. They don’t work as quickly as antacids but they tend to reduce symptoms of GERD for longer. Examples include Tagamet HB, Pepcid AC, and Axid AR. Stronger versions can be obtained through a prescription.
Proton pump inhibitors (PPIs): These are stronger acid blockers than H2 blockers and reduce symptoms long enough for the esophagus tissue to heal. Examples include Prilosec OTC and Zegerid OTC. Stronger versions can be obtained through a prescription. Side effects are uncommon and may include headache, diarrhea, and upset stomach.
Surgery
Surgery is not generally recommended to treat GERD unless it does not respond to medications.
Fundoplication: This is the most common surgical option to treat the condition and often leads to long term improvement. It is a minimally invasive procedure that wraps the top of your stomach around the lower esophageal sphincter. This adds pressure to the muscle and prevents reflux.
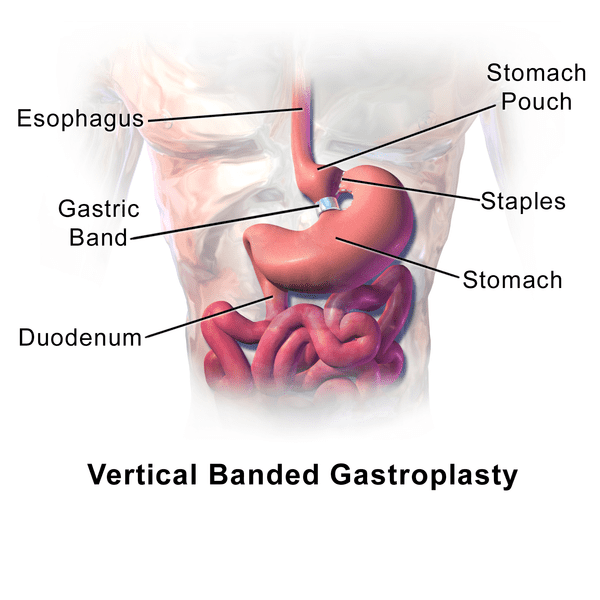
Bariatric surgery: If you are obese with GERD your doctor may recommend this type of surgy, often gastric bypass surgery. It helps both relieve symptoms and reduce weight.
LINX device: This is a ring of tiny magnetic beads that is wrapped around the connection between the stomach and the esophagus. The beads expand to let food through but are strong enough to keep the opening closed to prevent reflux. The device is placed using minimally invasive surgery.
Transoral incisionless fundoplication (TIF): This procedure creates a partial wrap around the lower sphincter using polypropylene fasteners. It is performed through the mouth and does not require surgery.
If you liked this article, you should check out our other posts in the Nebula Research Library!
May 23, 2023
