Table of contents
Nebula Genomics DNA Report for Anemia
Is anemia genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Anemia?
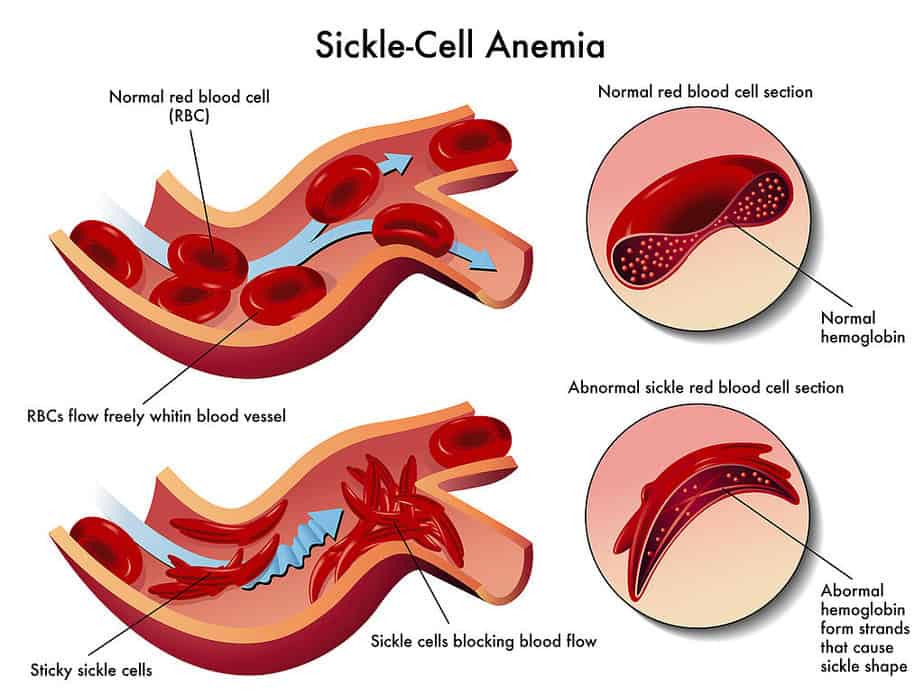
Anemia is a reduction of the number of red blood cells below the age- and sex-specific norm. Iron deficiency is the leading cause of the condition. Another common type of anemia is sickle cell anemia, a specific form of a larger category of sickle cell disease. Different types of anemia can occur based on why the red blood cell count is low:
- Not enough hemoglobin (low hemoglobin)
- Hemoglobin doesn’t work correctly
- Not enough red blood cells
- Break down of red blood cells occurs too quickly
Hemoglobin is a protein that carries oxygen from the lungs to other organs in the body. It is found in the blood, predominantly in the red blood cells (erythrocytes) along with iron. When a patient has this condition, it reduces the oxygen-carrying capacity of the blood, and organs may not receive enough oxygen to function properly.
To further ensure oxygen supply to the organs, the organism typically reacts by increasing the heart rate to pump blood faster through the circulation. However, this makes it easier for the body to reach its stress limits. Typical symptoms of anemia include easy fatigue, shortness of breath, especially during physical exertion, and frequent headaches.
Anemia is either acquired or congenital. Causes of acquired anemia can be blood loss, increased blood breakdown, diseases of the hematopoietic system, deficiency diseases, kidney diseases, hormonal disorders, pregnancy, or “consumptive diseases” such as tumor diseases or chronic inflammatory diseases. A common example of congenital anemias is genetic disorders of hemoglobin formation (sickle cell).
Is Anemia Genetic?
In addition to physical causes, like blood loss, some inherited conditions and specific genetic mutations lead to various forms of anemia.
Experts have associated mutations in the TMPRSS6 gene with a type of the condition called refractory iron deficiency anemia (IRIDA). This gene encodes a protein that helps regulate iron levels in the body. Gene mutations cause this protein to malfunction and thus cause a shortage of iron in the bloodstream.
Hereditary forms
There are specific forms of the condition that are hereditary, or passed from parent to child. Family history and genetic testing can help assess you or your child’s risk of developing one of these conditions. Congenital pernicious anemia is a rare form of genetic anemia in which the body is unable to make intrinsic factor, a protein needed for vitamin B12 production. Fanconi anemia occurs when the bone marrow does not produce enough new blood cells. Bone marrow is the soft, spongy tissue found in most bones. Patients with this condition are also at higher risks of infections and certain types of leukemia.
Experts characterize hereditary spherocytosis as red blood cells that are sphere-shaped and unusually fragile. Because they cannot travel to other parts of the body easily, they are usually destroyed in the spleen without delivering oxygen to other organs. Finally, thrombotic thrombocytopenic purpura occurs when a faulty blood-clotting enzyme prevents a normal amount of platelets from circulating. Poor blood clotting can result in excessive bleeding, which ultimately leads to anemia. Patients can acquire this condition later in life.
Other common genetic mutations associated with anemia include:
HBB: People with a genetic mutation in this gene have sickle cell anemia. The mutation causes hemoglobin to form incorrectly, which leads to red blood cells that form in a crescent shape. The symptoms can be severe and even lead to heart attack and stroke.
The α- and β-globin gene clusters on chromosome 16 and chromosome 11: People with these genetic mutations will often have a condition called thalassemia. With this disease, genetic mutations prevent the body from producing enough hemoglobin.
Current Research on Anemia
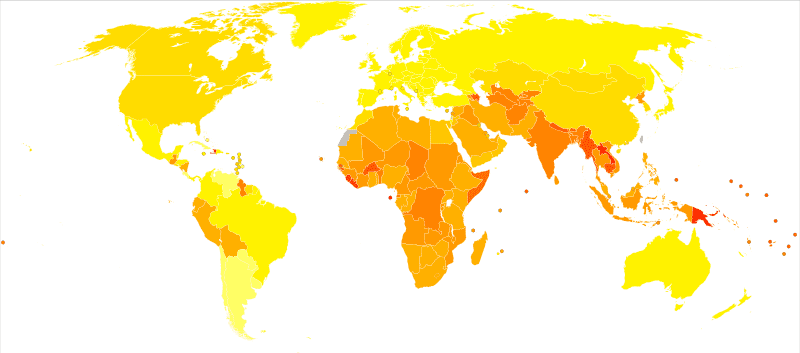
Sickle cell disease is not limited to geography and is evenly spread among the different races. It is common among people with African origins and Mediterranean countries such as Turkey, Greece, and Italy. Other countries that seem to have hereditary traits of the disease include the Arabian Peninsula, India, Spain, and other parts of the Caribbean. In the United States, Sickle Cell Disease is one of the common inherited blood disorders, and it affects about 100,000 Americans.
According to the US Department of Health and Human Services and Genetics Home Reference, patients inherit sickle cell anemia in an autosomal recessive pattern. That is, both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition both have a copy of the mutated gene, but they typically do not show signs and symptoms of the disease.
Regarding sickle cell anemia, a person who carries one copy of the mutated gene is a carrier for the condition or sickle cell trait. With two people who are carriers of an autosomal recessive disorder, there is a 25% chance the offspring will have the condition, a 50% chance of being a carrier, and a 25% chance of not having the condition of being a carrier.
The studies
An early research study termed “Iron refractory iron deficiency anemia” states that, for people with sickle cell disease, hemoglobin S replaces at least one of the beta-globin subunits in hemoglobin. In sickle cell anemia, also called homozygous sickle cell disease, the most common form of sickle cell disease, hemoglobin S replaces both beta-globin subunits in hemoglobin. In other types of sickle cell disease, hemoglobin S replaces just one beta-globin subunit in hemoglobin.
Abnormal versions of beta-globin can distort red blood cells into a sickle shape. The sickle-shaped red blood cells die prematurely, which can lead to anemia. Sometimes the inflexible, sickle-shaped cells get stuck in small blood vessels and can cause serious medical complications.
Researchers are continuing to look for new and better treatments. In 2019, researchers discovered a therapeutic compound that can block a chemical pathway in the body and the result is an increase in the production of red blood cells. The FDA has already approved drugs that block this pathway for certain neurological disorders. Experts hope they can repurpose them for people suffering from severe anemia.
The Mayo Clinic is just one of many organizations currently conducting clinical trials on anemia treatments. Many of these trials are for patients undergoing specific complex surgeries or specific conditions, such as autoimmune disease.
Epidemiology
According to the World Health Organization (WHO), anaemia is a serious global public health problem that particularly affects young children and pregnant women. The organization estimates that 42% of children under five years of age and 40% of pregnant women worldwide are anaemic.
Pregnant women are especially susceptible to the condition. This can cause problems with pregnancy, including risk of death to the mother and low birth weight of the child.
It is the most common blood condition in the U.S., estimated to occur in three million Americans. People in the United States have their children screened for the condition at about 12 months. Additional supplementation may be necessary if the babies do not get enough iron from breast milk and formula. Preterm babies may be especially at risk for anemia. Your child’s pediatrician can recommend the best way to supplement iron in an infant’s diet.
Some forms are more common in people of certain races. The genetic disorder, sickle cell anemia, in particular, occurs among about 1 out of every 365 Black or African-American births and 1 out of every 16,300 Hispanic-American births. About 1 in 13 Black or African-American babies is born with sickle cell trait (SCT).
Symptoms
The most common signs and symptoms of anemia are feeling tired, shortness of breath, and feeling cold. These symptoms are a result of not receiving enough oxygen to the various organs and occur with all types of the condition.
Cleveland Clinic lists some additional common symptoms:
- Dizziness or weakness
- Headache
- Sore tongue
- Pale skin, dry skin, or easily bruised skin
- Unintended movement in the lower leg (restless leg syndrome)
- Fast heartbeat
Some patients experience additional physical signs such as brittle nails, hair loss, change in taste, or ringing in the ears. People with the sickle cell form of the disease, in particular, are prone to heart and lung problems. This disease can cause especially serious symptoms, including chronic pain, bone and joint damage, ulcers, and swollen hands and feet.

If left untreated, anemia results in further complications like arrhythmia (irregular heartbeat), an enlarged heart, or heart failure.
In children, anemia may cause lack of attention, delayed development of motor skills, and problems with learning. In contrast, older adults with the condition are more prone to confusion and depression.
Causes
Physical factors that affect the number of red blood cells include:
- chronic blood loss
- lack of red blood cell production
- high rates of destruction of red blood cells
Iron deficiency
The most common cause of anemia is not having enough iron. People need iron to make enough hemoglobin, the oxygen-carrying protein inside of red blood cells.
Some patients may have conditions that make them more susceptible to iron-deficient anemia:
- Heavy periods
- Pregnancy
- Ulcers
- Colon polyps or colon cancer*
*Learn more about colon cancer genetic testing in our special hereditary cancer series.
Vitamin deficiency
Vitamin deficiency anemia can occur if a diet does not have enough iron, folic acid, or vitamin B12. People need these vitamins to produce enough healthy red blood cells.
Inflammation
Anemia associated with inflammation can occur when a patient experiences diseases like cancer, HIV/AIDS, rheumatoid arthritis, kidney disease, Crohn’s disease, and other acute or chronic inflammatory diseases if they interfere with red blood cell production.
Genetic disorders
Genetic disorders include blood disorders such as sickle cell anemia and thalassemia, or cancer, as well as anemias associated with bone marrow disease, and hemolytic anemias (when red blood cells are destroyed too fast).
Patients can also inherit or develop hemolytic anemias later in life. Inherited types include sickle cell anemia and thalassemia. Sickle cell anemia, in particular, can lead to serious anemic symptoms. It forces red blood cells to assume a crescent (sickle) shape that cannot effectively carry oxygen and die prematurely. The metabolic disorder glucose-6-phosphate deficiency (G6PD) is also a genetic disorder that can cause the condition.
Aplastic anemia is another inherited or acquired rare condition. Infections, certain medicines, autoimmune diseases, and exposure to toxic chemicals can cause this condition.
Diagnosis
A diagnosis usually starts starts with a physical exam. In almost all cases, doctors diagnose anemia with a blood test called a complete blood count (CBC). To do this, a health care professional counts the number of blood cells, including red blood cells and white blood cells, in the sample.
Although normal adult hematocrit values vary, they are generally between 40% and 52% for men and 35% and 47% for women. Average adult hemoglobin values are usually 14 to 18 grams per deciliter for men and 12 to 16 grams per deciliter for women. Values below these standards are considered low and a classic characteristic of the condition.
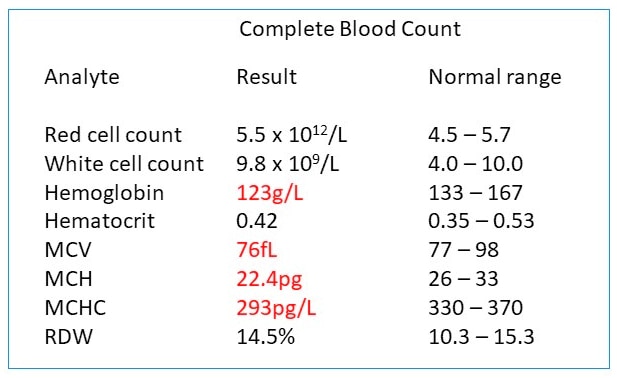
The blood sample may also be observed under a microscope to look for cells that are unusual sizes, shapes, and/or color.
If the condition is present, your doctor may order additional tests to diagnose the cause. These may include genetic testing to determine if you have genetic risks of congenital anemia.
Treatment
The treatment of anemia depends on the underlying cause and type.
Iron deficiency: This type is most often treated with iron supplements and changes to diet. Patients usually need these treatments long term. Any unusual blood loss is stopped.
Vitamin deficiency: This type is also treated with vitamin supplements and changes to diet. If the cause is related to poor vitamin B12 absorption from food, you may need supplemental shots of vitamin B12 on a regular basis.
Chronic disease: Doctors will focus on treating the disease that is causing the anemia.
Aplastic: This type is treated with blood transfusions or bone marrow transplants.
Bone marrow disease: Doctors may prescribe medication, chemotherapy, bone marrow transplants
Hemolytic: There are a number of different treatments that may be recommended depending on the type of hemolytic anemia present. These can include lifestyle changes like avoiding certain medications. Your doctor may also put you on immunosuppressants to prevent your immune system from attacking red blood cells.
Sickle cell: To treat this disease, you may be prescribed oxygen, pain relievers, and oral and intravenous fluids to reduce pain and prevent complications. Doctors also prescribe blood transfusions, folic acid supplements, and antibiotics.
Thalassemia: Most cases are mild anemia and do not require treatment. Some more severe cases may need blood transfusions, folic acid supplements, medication, removal of the spleen, or a blood and bone marrow stem cell transplant.
For more information, you may want to check out the National Institutes of Health.
If you liked this article, you should check out our other posts in the Nebula Research Library!
February 10, 2023
