Table of contents
Nebula Genomics DNA Report for Ulcerative Colitis
Is ulcerative colitis genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of October 2021 |
What is Ulcerative Colitis?
Part 1 of Is ulcerative colitis genetic?
Ulcerative colitis (UC) is a chronic digestive disease of the colon and rectum where these areas in the GI tract experience inflammation and ulcers. Patients most often experience abdominal pain and bloody diarrhea. Weight loss, fever, and anemia may also occur. The symptoms tend to appear gradually before becoming more severe.
The cause of ulcerative colitis is unknown, but most doctors suspect it is a combination of genetic and environmental factors, including changes to the normal gut bacteria. It is slightly more common in the developed world, suggesting that a western diet and lifestyle play an important role in the environmental drive of the disease.
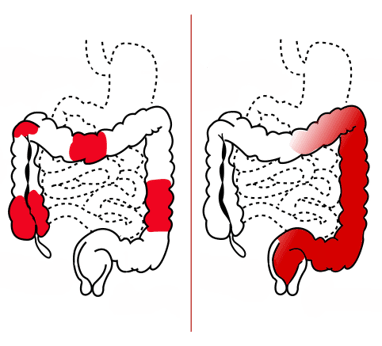
The condition is one of the inflammatory bowel diseases (IBDs) along with Crohn’s disease and microscopic colitis.
Diagnosis can be performed with either a colonoscopy, tissue biopsy, or both. Although the condition itself cannot be cured, there are several treatments aimed at reducing the symptoms. One of the most simple treatment options is a change in diet to high-calorie or lactose-free foods. Certain medications are also available. If the condition is particularly bad, your doctor may also recommend surgery to remove the colon and/or rectum.
Types
Types of the condition are classified based on how much of the rectum and large intestine (colon) are affected.
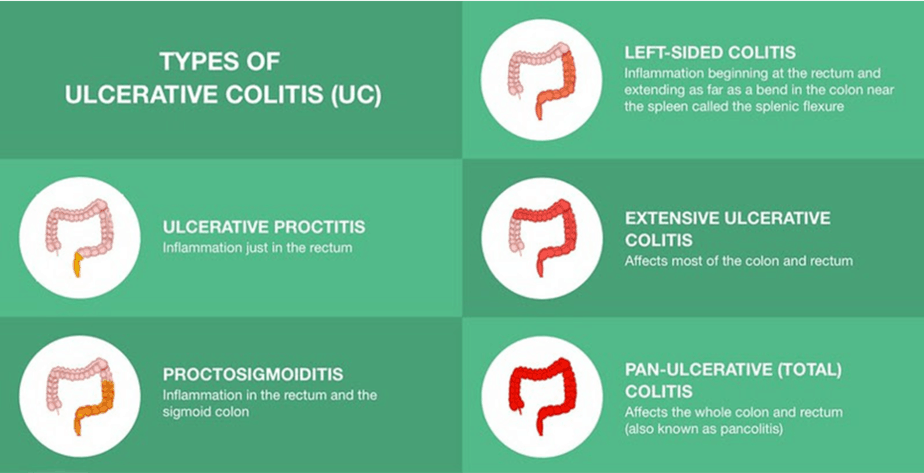
- Ulcerative proctitis: Inflammation is confined to the area closest to the anus (rectum)
- Proctosigmoiditis: Inflammation involves the rectum and the lower end of the colon
- Left-sided colitis: Inflammation extends from the rectum up through the sigmoid and descending colon
- Extensive: Inflammation often affects most of the colon and rectum
- Total: Inflammation affects the entire colon and rectum
Is Ulcerative Colitis Genetic?
Inherited genes seem to increase the risk of developing ulcerative colitis.
Although the inheritance pattern of the condition is unknown due to the fact that many genetic and environmental factors are involved, having a close family member with the disease does increase the likelihood that you will develop it as well. Some studies have found that 1 in 4 patients also have a family history of the condition. Another sign that it is linked to hereditary factors is that it is more likely to occur in certain ethnic populations.
Scientists have identified several dozen variants that may contribute to the condition. Many of them are involved in the protective barrier of the intestines. This barrier protects tissues from bacteria that live in the gut and toxins that pass through the digestive system. A breakdown of the barrier may lead to the immune response that ultimately causes the condition.
Mutations in genes related to the immune system are also likely to promote the disease. Some known genes associated with ulcerative colitis are IL23R, which codes for a protein embedded outside certain immune cells called T cells, and IRF5, which codes for a transcription factor that activates other parts of the immune system, including interferons and other cytokines.
Current Research on Ulcerative Colitis [Updated October 2021]
Most people that suffer from the condition have relatives with the disease. However, the genetic factors that influence it are complex and need more research to understand completely.
Researchers have had difficulty pinpointing the genes responsible for UC as suspected genes tend to be related to other Inherited Bowel diseases (IBD) such as Crohn’s and other types of infection. However, the clustering of IBD, which majorly includes Crohn’s and ulcerative cancer, has suggested that people who develop both diseases seem to have a relationship with a relative, including distant family members.
Generally, about 10 to 25 percent of people with UC have a parent or sibling with IBD (either UC or Crohn’s disease). The risk of UC is also higher among more distant relatives, like grandparents and cousins. UC that affects multiple family members often starts at an earlier age than in people with no family history of the condition.
A study from 2012 titled New Genetic Links for Crohn’s and Colitis discovered that many genes related to host-microbe interactions have a strong IBD relationship. The group studied both Crohn’s Disease and Ulcerative Colitis and acquired raw data that proved that the majority of genetic risk factors are associated with both diseases. Ramnik Xavier, an HMS professor of Medicine and team key member, explained that Crohn’s Disease and UC might not be two distinct diseases but collections of many different ones.
From the research conclusion, no specific gene was mentioned to be responsible for UC or Crohn’s Disease as almost all genes with risk contributed for IBD to be genetically passed.
Research continues into the genetic basis of UC as a means to better diagnose and treat the condition. In October 2020, a bioinformatics analysis was performed in mouse models to determine UC-related genes expressed during times of UC-induced inflammation that may be used in diagnostics.
Overall, 177 genes were identified in inflammation-related pathways. Seven clusters were found to be associated with UC. Three genes (CXCL13, NYP1R, and CXCR2) were identified in mouse models but only CXCR2 was found to be significantly different as an inflammation marker compared to non-UC mice.
In 2021, Nature Communications published a study investigating shared genetics between IBDs and multiple sclerosis (MS). The study revealed a strong overlap between UC and MS. Such research may lead to therapies that target both immune disorders.
Epidemiology
Part 4 of Is ulcerative colitis genetic?
Ulcerative colitis has the greatest prevalence in Northern Europe and North America, suggesting that a western diet plays a role in the disease. Ulcerative colitis has an incidence of 9 to 20 cases per 100,000 persons per year. Its prevalence is 156 to 291 cases per 100,000 persons per year. Of the IBDs, ulcerative colitis is more prevalent in adults, while Crohn’s disease is more common in children.
The typical age of onset is between 15-30 years, with a second onset between 50-70 years. Most studies suggest that the condition equally affects both men and women.
The removal of the appendix (appendectomy) before the age of 20 has been shown to be associated with a decreased risk of ulcerative colitis. This is the opposite pattern for Crohn’s disease.
Symptoms of Ulcerative Colitis
Part 5 of Is ulcerative colitis genetic?
The inflammation that causes the condition starts in the rectum and may spread to the colon.
Symptoms tend to be episodic, meaning that a patient will have periods of symptoms, known as flare-ups, followed by times of remission, when no symptoms are present.
Symptoms often start mild to moderate and then progress over time. According to Cleveland Clinic, some of the early signs are:
- Diarrhea or urgent bowel movements
- Abdominal (belly) cramping
- Tiredness
- Nausea
- Weight loss (as a consequence of lack of appetite)
- Anemia (low red blood cell count)
- Delayed growth and development in children
More advanced symptoms of ulcerative colitis include:
- Blood, mucous, or pus in bowel movements
- Rectal bleeding
- Severe cramping
- Fever
- Skin rashes
- Mouth sores
- Joint pain
- Red, painful eyes
- Liver disease
- Loss of fluids and nutrients
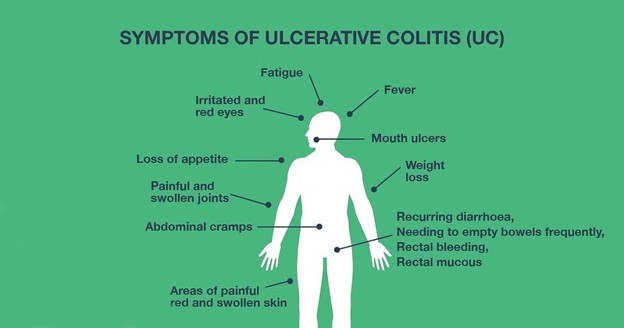
In certain cases, ulcerative colitis may be linked to conditions outside the digestive system, such as arthritis, eye inflammation, liver disease, and osteoporosis. These complications are thought to be a result of an overactive immune response associated with ulcerative colitis.
Causes of Ulcerative Colitis
Part 6 of Is ulcerative colitis genetic?
While the cause of ulcerative colitis is unknown, it is thought to be the combination of a number of factors, including an immune system response, genetics, and the environment.
Many doctors believe ulcerative colitis is an autoimmune disease in which the body’s immune system mistakenly attacks healthy cells in the digestive system. The result is the inflamed tissue in the affected area. There are several reasons being investigated as to the origin of the inflammation.
One theory is that the body mistakes the good bacteria in the gut for dangerous bacteria, while another theory suggests an outside bacterial infection that the immune system responds to but remains active after the infection clears. Others suggest that the immune system may simply malfunction on its own.
The condition is more prevalent in some regions of the world, suggesting a strong environmental factor. Namely, it is more common in developed countries in Northern Europe and North America. Some have suggested that air pollution, medication, and certain diets may all play a role. Improved sanitation systems leading to less bacterial exposure may also contribute.
Other ulcerative colitis risk factors include:
- Having a close family member with the disease
- Eating a high-fat diet
- Frequently using nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil® or Motrin®).
Those of Ashkenazi Jewish descent are also at a higher risk.
Diagnosis of Ulcerative Colitis
Part 7 of Is ulcerative colitis genetic?
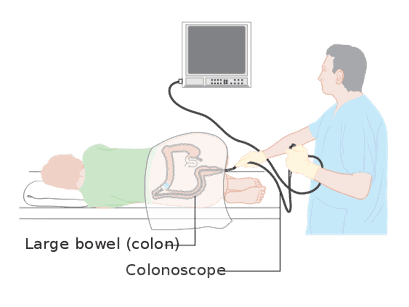
The only way to positively diagnose ulcerative colitis is through a tissue biopsy. Other tests and procedures may be conducted to rule out similar conditions, such as Crohn’s disease.
Lab tests
Blood tests for this condition usually look for signs of anemia, a lower-than-normal red blood cell count. Stool tests can also help diagnose the condition by analyzing for white blood cells in the stool or by ruling out other digestive disorders like bacteria or virus infections.
Endoscopic procedures
The most common method to diagnose this condition is through a colonoscopy. During this procedure, a thin, flexible, lighted tube with a camera on the end is weaved through the entire colon. A small amount of tissue for a biopsy is taken at this time. The biopsy is necessary for a conclusive diagnosis. If the colon is very inflamed, an alternative procedure called a flexible sigmoidoscopy may be used instead. In this very similar procedure, the doctor will only insert the tube into the rectum and lower end of the colon.
Imaging
Imaging techniques are only used if your doctor suspects severe complications from the disease. For example, X-rays or CT scans can reveal serious damage, such as a perforated colon. On the other hand, enterography scans are more sensitive tests that can identify inflammation through non-invasive procedures, especially if the inflammation has spread to the small intestine.
Did you know you can test for inflammation at home? Check out this review article on at-home inflammation tests to learn more!
Treatment of Ulcerative Colitis
Part 8 of Is ulcerative colitis genetic?
There is no cure for the condition, but medications and lifestyle changes can help treat the symptoms and improve quality of life. Medications are generally prescribed based on the severity of the disease and often have to be tailored to the individual patient.
Anti-inflammatories
Anti-inflammatory drugs, 5-aminosalicylates or corticosteroids, are often the first type of drug prescribed. 5-aminosalicylates can be taken by mouth or as an enema or suppository, depending on the location of the damage in your colon. Corticosteroids are generally reserved for short-term treatment of more severe cases as they may result in serious side effects.
Immunosuppressants
Immune system suppressors will decrease the effectiveness of the entire immune system in an effort to reduce the inflammation that is causing the ulcerative colitis symptoms. They can be prescribed alone or as a combination.
Mayo Clinic describes some of the most commonly used immunosuppressants:
Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan) are the most commonly prescribed types of this drug. You will keep regular check-ups with your doctor to check for side effects on the liver and pancreas.
Patients with ulcerative colitis who don’t respond well to those medications may try and take cyclosporine (Gengraf, Neoral, Sandimmune). However, this drug cannot be used in the long term due to serious side effects.
Finally, tofacitinib (Xeljanz) can be prescribed if other therapies do not work well. Recently, the FDA reported preliminary data showing an increased risk of serious heart-related problems and cancer from taking this drug. Therefore, patients currently taking it should consult their doctor.
Biologics
Biologics are special types of drugs that target proteins in the immune system. They are generally reserved for severe cases that do not respond well to any other treatment. They can either block certain proteins produced by the immune system or prevent inflammatory cells from getting to the site of inflammation.
Most patients will take additional over-the-counter medications that can help reduce symptoms of the condition. They can include antidiarrheal drugs, pain relievers, antispasmodics (to help with cramps), and iron supplements (to treat anemia).
Surgery
Surgery is usually an option for the most severe cases. During this procedure, a surgeon will remove the colon and rectum. This will usually involve the surgeon constructing a pouch from the end of your small intestine attached directly to your anus so that you can pass stools fairly normally. If this is not possible, the surgeon will create a permanent opening through which stool is passed into a bag.
Screening
People with ulcerative colitis or Crohn’s disease need to be especially careful to screen for colon cancer, which they are at an increased risk for due to their condition. Learn more about colon cancer genetic testing in our special hereditary cancer series.
You can learn more about diagnosis and treatment options from the American Society of Colon and Rectal Surgeons and the National Institute of Diabetes and Digestive and Kidney Diseases.
If you liked this article, you should check out our other posts in the Nebula Research Library!
October 5, 2021
