Emerging research consistently finds new ways our body systems connect and the correlation between diverse diseases. Hypertension, a condition marked by persistently high blood pressure throughout the day, is a common condition. It puts extra strain on the heart, compelling it to work harder to pump blood throughout the body. The World Health Organization estimates that hypertension impacts around 1.28 billion adults between the ages of 30-79.
If left untreated, hypertension can increase the risk of heart attack, stroke, and other significant health issues. Thus, doctors recommend adults monitor their blood pressure at least once every two years. Prevention and control of high blood pressure often hinge on healthy lifestyle choices, including a balanced diet, regular exercise, and avoiding smoking. Additionally, a doctor may prescribe medication to patients struggling to control their blood pressure despite lifestyle modifications.
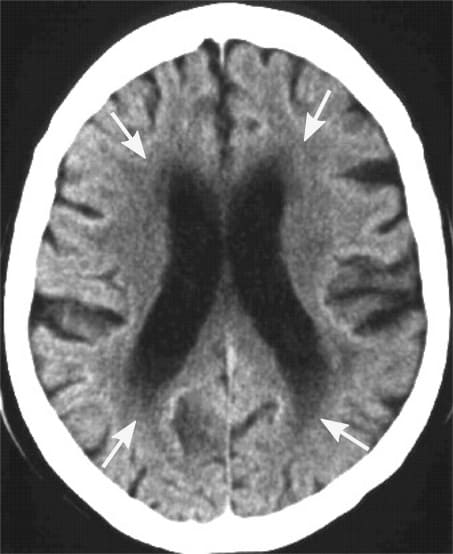
However, the implications of blood pressure go beyond the heart. Earlier clinical trials demonstrate that hypertension treatment can shield the brain from progressing white matter lesions (WMLs). WMLs are abnormal areas of myelination, often indicative of cerebral small vessel disease. Their development could signal advanced brain aging and neurodegenerative disease.

A recently published study in JAMA explored the association between intensive blood pressure management and the reduction of small vessel disease markers, including WML progression. The authors hypothesized that a more rigorous approach to treating hypertension could enhance the protection of the frontal brain regions, where WMLs typically originate.
| This post may interest those with a higher polygenic risk score for hypertension. |
The Study
The study analyzed a group of patients from the Systolic Blood Pressure Intervention Trial (SPRINT). The trial, consisting of 14,692 participants, compared the impact of intensive blood pressure control (systolic BP target <120 mm Hg) versus standard control (systolic BP target <140 mm Hg) in participants aged 50 years or older. These individuals were diagnosed with hypertension but did not have diabetes or a history of stroke. The trial’s primary focus was cardiovascular disease, with supplementary kidney and cognitive function analysis.
This new study analyzed data from a subset of SPRINT participants who underwent magnetic resonance imaging (MRI). The MRI scans offered crucial insights into brain health. Initially, 670 participants had MRIs, and 458 returned for a follow-up MRI 48 months later. Approximately half of these participants received intensive blood pressure treatment, with the remainder receiving standard therapy.
Results
Participants undergoing intensive blood pressure treatment showed less growth in white matter volume than their counterparts on standard therapy. This result implies that intensive blood pressure management might slow the progression of white matter lesions and improve brain health.
While these results align with prior studies regarding brain health, it is the first to segment results by brain regions in a large patient cohort.
The authors acknowledge certain limitations in their study, such as the 4-year gap between the initial and follow-up MRI scans and the reduced number of participants who completed the follow-up MRI. The authors recommend larger cohort sizes in future trials to address these limitations.
In conclusion, the study determined a positive correlation between rigorous blood pressure management and reduced occurrence of small vessel disease markers (e.g., a slowed progression of white matter lesions) in specific brain regions. These results could help researchers target certain brain regions in small vessel disease research. It also suggests that keeping blood pressure in check through healthy habits and medication, if needed, can improve brain health.
Citation
Rashid T, Li K, Toledo JB, Nasrallah I, Pajewski NM, Dolui S, Detre J, Wolk DA, Liu H, Heckbert SR, Bryan RN, Williamson J, Davatzikos C, Seshadri S, Launer LJ, Habes M. Association of Intensive vs Standard Blood Pressure Control With Regional Changes in Cerebral Small Vessel Disease Biomarkers: Post Hoc Secondary Analysis of the SPRINT MIND Randomized Clinical Trial. JAMA Netw Open. 2023 Mar 1;6(3):e231055. doi: 10.1001/jamanetworkopen.2023.1055. PMID: 36857053; PMCID: PMC9978954.
