Nebula Genomics DNA Report for Heart Disease
Is heart disease genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
What is Heart Disease?
Heart disease can refer to various cardiovascular diseases that affect the functioning of the heart muscle or blood vessels. Ultimately, these disorders can lead to a life-threatening condition called congestive heart failure. Although heart disease is common and can easily be deadly, you can often reduce your risk through healthy lifestyle changes and medications when appropriate.
Common types of heart disease
- Arrhythmia: a heart rhythm abnormality
- Atherosclerosis: a hardening of the arteries
- Cardiomyopathy: a condition that causes the heart to harden or grow weak
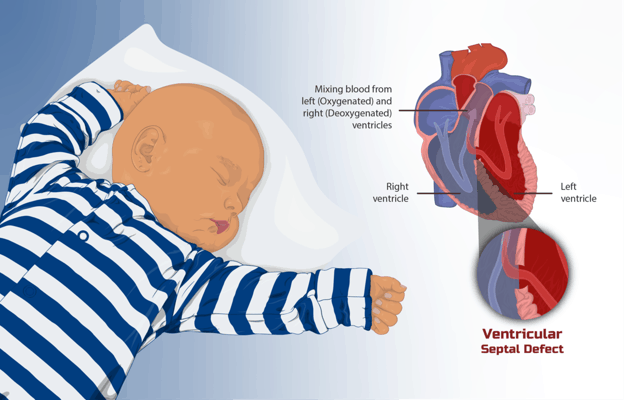
- Congenital heart defects: irregularities present at birth
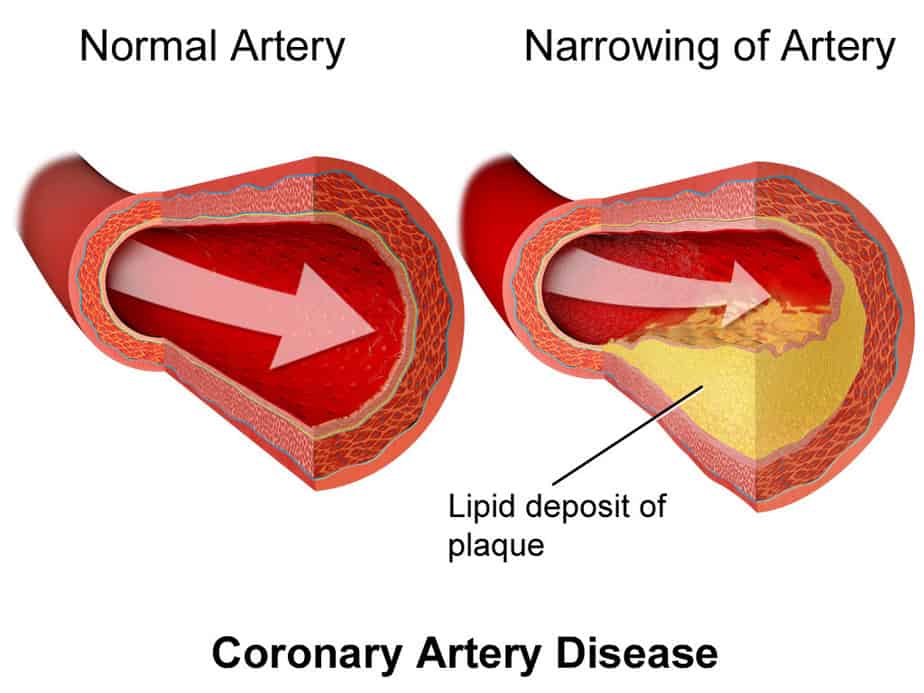
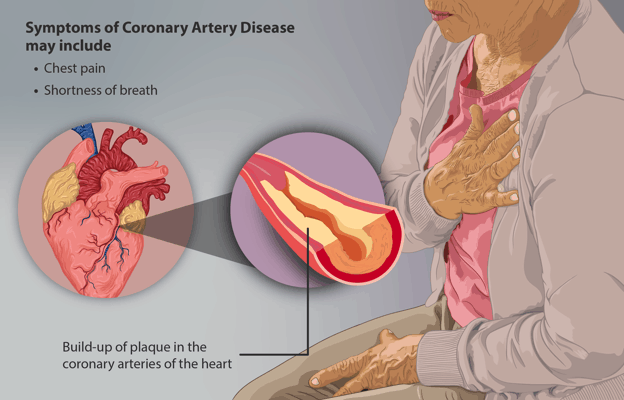
- Coronary artery disease (CAD): a blood vessel condition caused by the buildup of plaque in the heart’s arteries. It is often associated with atherosclerosis
- Heart infections: infections caused by bacteria, viruses, or parasites
- Valvular heart disease: a condition caused by damage to the blood valves
Risk factors
Those with high blood pressure or high cholesterol, or smokers are at the highest risk of heart disease.
Experts also consider certain medical conditions and lifestyle choices as significant factors in increasing risk. These risks for heart disease include diabetes, being overweight or obesity, an unhealthy diet, physical inactivity, and excessive alcohol use.
While patients can control many risk factors (smoking, diet, etc.), some risk factors they cannot. These include age, sex, and family history of heart disease.
Is Heart Disease Genetic?
While most cases of the condition are not genetic, family history does play a role in developing heart disease. That is, you are more likely to develop it if a close family member is known to have it. One explanation for this observation is that people in the same family are more likely to have the same environment and risk factors, such as smoking or being overweight.
There are some cases in which inherited heart conditions are passed on through genetic heart disease. Some of these inherited heart diseases are familial hypertrophic cardiomyopathy, familial dilated cardiomyopathy, and familial hypercholesterolemia.
People with a known family history of any of these genetic disorders are encouraged to talk with their doctor early to create a monitoring and early treatment plan. Genetic tests can also help detect these heart disorders.
Current Research on Heart Disease
Studies have shown that it is possible to inherit quite a number of heart diseases. The list includes long QT syndrome (LQTS), Brugada syndrome, hypertrophic cardiomyopathy, progressive cardiac conduction defect (PCCD), arrhythmogenic right ventricular cardiomyopathy, and dilated cardiomyopathy. People can also inherit other diseases that lead to cardiac conditions.
Variations in the genetic structure can lead to heart diseases. For this reason, once a doctor detects heart disease in a member of one’s family, it is wise for every member to test. The following are examples of heart diseases caused by genetic mutations and that can be passed down from parents to children.
Conditions with a genetic component
Long QT syndrome: Long QT syndrome is a heart condition that causes a disruption in the rhythmic beating. This disease causes the heartbeat to abruptly speed up. This abrupt increase in the beating rate can cause one to lose consciousness or even die suddenly. Genetic mutations cause long QT syndrome and can be either inherited or acquired.
Brugada syndrome: Brugada syndrome causes an erratic heartbeat, where the lower ventricles of the heart pump blood out of tempo. This causes a problematic flow of blood around the body that can lead to dizziness due to the poor supply of blood to some parts of the body and can even lead to sudden death in extreme cases.
Experts have recorded several cases where people with Brugada syndrome die suddenly in their sleep. Although Brugada syndrome is rare, it can be easily passed to offspring, requiring only one parent for it to be passed.
Hypertrophic cardiomyopathy: In this condition, the muscles of the heart become dense, which makes pumping blood difficult. Most people with hypertrophic cardiomyopathy lead normal lives as it often doesn’t have any symptoms. The symptoms experienced by only a small percentage of individuals with the disease include short breath and tightness of the chest. This condition can lead to complications in the heart’s nervous operations, which can cause sudden death in extreme situations.
Progressive cardiac conduction defect (PCCD): A disruption in the electrical system of the heart causes progressive cardiac conduction defect (PCCD). These disruptions in the impulses cause problematic pumping of blood, which can lead to cardiac arrest. The risk of sudden death in PCCD is somewhat lower than in the other conditions in this list.
Genetic testing
Current studies establish that the surest way to detect the susceptibility of an individual to heart diseases is through genetic testing. Evaluating the number of relatives with heart diseases as well as the gender and the age the disease became apparent can help make an informed decision on how likely an individual is to develop a cardiac condition.
Family members of people with any of the above-listed heart conditions should consider getting tested. Treatments for these heart diseases are most effective when patients start them early.
Epidemiology
According to the Centers for Disease Control and Prevention (CDC), heart disease is the leading cause of death in the United States, with 1 in 4 deaths resulting from the condition. This is equivalent to about 610,000 people per year.
It is the leading cause of death for most men, women, and racial and ethnic groups. For women of Pacific Island, Asian, American Indian, Alaskan Native, or Hispanic descent, deaths from heart disease are second only to cancer.
The southeaster area records the most deaths from heart disease in the United States.
Coronary artery disease is the most prevalent form of heart disease, killing 365,914 people in 2017. The CDC estimates that about 6.7% of all adults over 20 years have the condition. In the United States, someone has a heart attack as a result of the condition every 40 seconds.
The risk of heart disease increases with age, especially among men. Generally, the condition is also more common in men than in women. This is because men tend to develop heart problems earlier in life and are at an especially higher risk of coronary artery disease. On the other hand, women are more likely to be affected by stroke, especially at an older age.
Although people usually associate heart problems with getting older, more people at a young age are experiencing heart attacks. Experts contribute this change to lifestyle factors such as decreased physical activity and increased processed foods.
Symptoms
Although symptoms of all heart diseases are similar, they can be specific depending on the type.
Arrhythmia
This condition occurs when your heart beats too slowly, too quickly, or simply irregularly. Patients may experience:
- A fluttering in their chest
- A racing heartbeat (tachycardia)
- A slow heartbeat (bradycardia)
- Chest pain
- Shortness of breath
- Anxiety
- Fatigue
- Lightheadedness or dizziness
- Sweating
- Fainting (syncope) or near fainting
Atherosclerosis/Coronary artery disease
When plaque builds up on artery walls, atherosclerosis occurs. This can cause damage to blood vessels and the heart and can ultimately lead to a heart attack, chest pain, or stroke if the heart is unable to pump blood effectively. For men, the first sign tends to be mostly chest pain, while women report additional symptoms such as shortness of breath or extreme fatigue. Unfortunately, for many, doctors only diagnose coronary artery disease after the person suffers a heart attack.
Cardiomyopathy
There are three types of this condition called dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy. Sometimes, symptoms are only noticeable after the condition has progressed. Symptoms include:
- Breathlessness with physical activity or at rest
- Swelling of the legs, ankles. and feet
- Fatigue
- Irregular heartbeats that feel rapid, pounding, or fluttering
- Dizziness
- Lightheadedness
- Fainting during physical activity
- Arrhythmias (irregular heartbeats)
- Chest pain, especially after physical exertion or heavy meals
- Murmurs (unusual sounds associated with heartbeats)
Heart infections
There can be different types of infections based on where the infection occurs or what causes it. These include pericarditis (infection of the membrane surrounding the heart), endocarditis (infection of the valves or inner lining), or myocarditis (a rare disease caused by a viral infection or autoimmune response). Symptoms include:
- Shortness of breath
- Fatigue
- Lightheadedness and fainting
- Heart palpitations
- Chest pain or pressure
- Fever
- Abdominal or leg swelling
- Aching joints or muscles
- Blood in the urine
- Red, tender spots under the fingernails
- Tiny purple or red spots on the skin, whites of the eyes, or inside the mouth
Valvular heart disease
Depending on which valve is affected, symptoms may include:
- Fatigue
- Shortness of breath
- Irregular heartbeat
- Swollen feet or ankles
- Chest pain
- Fainting
If left untreated heart conditions greatly increase the risk of sudden cardiac death, a sudden death caused by loss of heart function.
Causes
Like the symptoms, the cause of heart disease is specific to the type. The buildup of plaque on the arteries causes coronary artery disease, the most common type of the condition. An unhealthy lifestyle that includes poor diet, lack of exercise, smoking, and being overweight is the most important risk factor for heart disease.
Arrhythmia is usually a side effect of other heart conditions. On its own, it is usually not deadly but may be a sign that something else is wrong. Congenital heart defects normally occur while the heart develops before birth. Certain conditions, medications, and genes may increase the risk of this occurring.
In many cases, the cause of cardiomyopathy is unknown. Experts believe damage to the heart causes the most common type, while others are inherited conditions. Bacteria, viruses, and parasites will cause heart infections.
Valvular disease may be present at birth, or conditions such as rheumatic fever, infections, or connective tissue disorders may trigger it.
Diagnosis
After taking a family history, your doctor will probably recommend blood tests and a chest x-ray to diagnose heart disease. Blood tests usually account for a lipid profile (total cholesterol, low density lipoproteins – LDL, high density lipoproteins – HDL, and triglycerides), lipoproteins, C-reactive protein (CRP), and homocysteine.
Patients who are at the highest risk may choose to undergo screenings on a regular basis.
Did you know that you can test for heart health at home? Check out this article to learn more!
Further tests that doctors perform in a clinic may include an electrocardiogram (EKG or ECG), which measures cardiac electrical activity. This is a common, noninvasive procedure that takes less than 5 minutes to perform. Your doctor will look for abnormalities that could signal a problem.
Another common visualization is an echocardiogram, which is an ultrasound of the heart. This procedure is also noninvasive and often takes about 45 minutes. Doctors perform both electrocardiograms and echocardiograms at rest or during stress (physical exercise like a treadmill).
Sometimes, an invasive test called cardiac catheterization may be necessary to better diagnose the condition. This procedure involves inserting a long, flexible tube into a blood vessel, usually in the wrist or groin, and gently guiding it to the heart. X-rays are used to help guide the catheter and determine how well blood is flowing through the heart and whether there are other structural problems.
Other imaging tests, such as a CT scan or an MRI, may also be recommended.
Treatment
Exercise and eating a heart healthy diet are lifestyle changes often recommended for people who want to treat or prevent heart disease.
There are several treatments for heart disease depending on the type and extent of the damage. Especially in the early stages, your doctor will most likely recommend lifestyle changes that reduce your risk. These lifestyle changes often include:
- Quitting smoking
- Eating a healthy diet
- Increasing physical activity
- Reducing alcohol consumption
Certain patients whose condition does not improve with lifestyle changes may be recommended certain medications. There are a lot of different medications that target different cardiac functions, and they are prescribed based on the type of disorder present. Some examples of heart disease medications include ACE inhibitors, ARBS, anticoagulants, antiplatelets, beta-blockers, calcium channel inhibitors, cholesterol medications, digitalis, and nitrates.
If the condition does not respond to either lifestyle changes or medications, surgery may be recommended. The type of surgery depends largely on the type of condition present. For example, coronary artery disease patients with blocked arteries may be prescribed a stint to be inserted in the blocked artery to return normal blood flow. The type of procedure may also depend on the extent of the damage.
You can find more options for treatment on the American Heart Association’s website.
If you liked this article, you should check out our other posts in the Nebula Research Library!
May 23, 2023
