As we covered in last week’s article, diabetes is a chronic condition that can lead to lifelong health problems. It occurs when the body does not produce or respond to insulin, causing elevated glucose levels. Patients often experience complications such as eye disease. Recently, researchers discovered an important cascade of molecular events that links periods of low blood sugar levels with diabetic retinopathy (blood vessel damage in the eye). Understanding this molecular pathway that links low glucose and diabetic eye disease may one day help doctors create better diabetes management plans and more effective drugs.
Diabetic eye diseases are conditions that affect people who have diabetes. They include diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma. Over time, these conditions can lead to blurred vision and blindness.

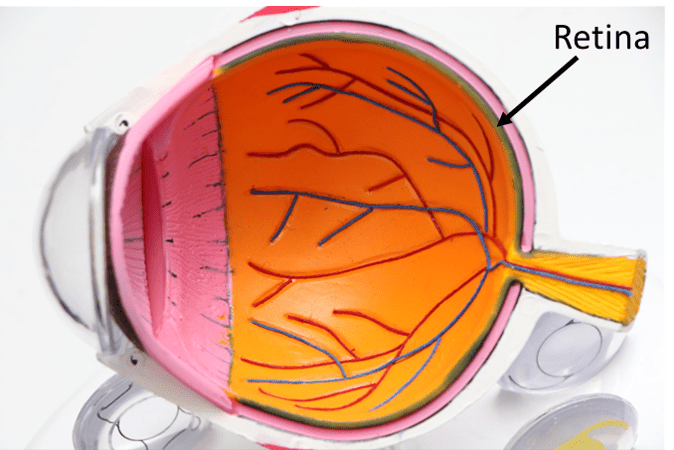
In particular, diabetic retinopathy occurs when a patient experiences abnormal, leaky blood vessels around the retina, the inner lining at the back of each eye that senses light and promotes vision. Experts agree that eye damage results from high glucose levels, a hallmark of diabetes.
However, new research suggests that in addition to elevated glucose levels, diabetic eye disease may also be linked to glucose variability (switching between high and low levels), causing molecular changes that lead to blood vessels in the retina being damage. A better understanding of the root cause of this disease may one day lead to better medications for those at risk of vision loss caused by diabetes.
The Study
Published in Cell Reports, the researchers at Johns Hopkins Medicine show that periods of low glucose lead to a molecular cascade of events that promote worsening eye disease. This result seems to contrast with the belief that chronically high glucose levels are the main culprit of eye damage caused by diabetes. It also questions the popular diabetes treatment, tight glycemic control (TGC). While the treatment decreases average glucose levels, it is also associated with worsening diabetic retinopathy.
To study this effect, the authors examined mice with occasional low glucose levels and human cells grown in the lab. First, they demonstrated that low glucose affects how the retina produces energy. Overall, cells produce less NAD+ and lactate, suggesting that energy production in the retina uses less glucose in an effort to preserve what little glucose is available.
But they need energy from somewhere. Therefore, the cells turn to oxygen as an alternative to meet energy needs. Using up oxygen available for energy creates a hypoxic (low oxygen) environment. This will be important later on.
They then examined specific glial retinal cells, a cell type that supports retinal neurons. In the presence of low glucose levels, these cells made more transcription factors that increase the expression of the GLUT1 gene, which encodes for a protein that moves glucose into the cell. Glial cells cannot use oxygen as a backup and must rely on glucose for energy production. Therefore, it makes sense that low glucose serum levels prompt an increase in the machinery needed to bring in more glucose.
The researchers discovered that as glial retinal cells produced more transcription factors, those molecules accumulated more in the cell nuclei. This previously unknown effect would lead to unintended consequences.
Results
Remember, the authors showed that low glucose levels produced a hypoxic cell environment. Then, there is also an increase in a specific transcription factor in the nucleus. Overall, they demonstrated that these two events, when they occur together, increase the expression of genes VEGF and ANGPTL4. Ultimately, the proteins such as VEGF damage blood vessels and may be the culprits of vision loss.
You may be wondering why brief periods of low glucose damage the eyes but constantly low glucose (i.e., someone without diabetes) does not. The answer lies in the role of glucose variability. If you don’t have diabetes, your glucose is steady and if you have uncontrolled diabetes your glucose is steady. It’s when it’s making major shifts that it seems to make this effect worse if eye disease has already started.
Conclusion
Overall, this research unlocks a newly discovered mechanism for why some people with diabetes seem to have a worsening eye disease, even when the patient is managing their glucose. Specifically, it shows that the eyes may be particularly vulnerable to brief periods of low glucose, which ultimately increases the production of proteins that damage the eye.
This study demonstrates that periods of low glucose may play a role in worsened vision outcomes. To prevent worsening diabetic eye disease, people with diabetes and their doctors should consider not just keeping glucose levels low but also keeping the low levels steady.
Citation
Guo C, Deshpande M, Niu Y, Kachwala I, Flores-Bellver M, Megarity H, Nuse T, Babapoor-Farrokhran S, Ramada M, Sanchez J, Inamdar N, Johnson TV, Canto-Soler MV, Montaner S, Sodhi A. HIF-1α accumulation in response to transient hypoglycemia may worsen diabetic eye disease. Cell Rep. 2023 Jan 31;42(1):111976. doi: 10.1016/j.celrep.2022.111976. Epub 2023 Jan 10. PMID: 36640318; PMCID: PMC9960808.
