Nebula Genomics DNA Report for Diabetes
Is diabetes genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is diabetes?
Diabetes mellitus is a chronic disease marked by increased blood sugar levels. Although sugars like glucose are necessary for proper cell and brain function, too much sugar in the blood can lead to serious health problems. Specifically, it is known as a disorder of carbohydrate metabolism. Some characteristics of this complex disorder include hyperglycemia, glucosuria, acidosis, and ketosis.

History of the disorder dates back to 250 BC when this term was coined by Apollonius of Memphis. The ancient Greeks and Persians have related diabetes with the sweet taste of urine. And this was due to the excessive excretion of sugars in the urine.
The idea of understanding the history of the genetics of this disorder has intrigued the scientists worldwide. In this context, studies from the 1970s have associated HLA genes with diabetes (type 1).
Published in 2000, results from genome wide screen for the susceptibility genes identified calpain-10 to be associated with diabetes (type 2) in a group of Mexican Americans. This work was among some of the first studies to map the susceptibility genes. In recent years, numerous other reports have identified more of the genetic architecture of the disease.
The Centers for Disease Control and Prevention (CDC) indicates that pregnant women should be especially aware of the complications that may arise while pregnant and trying to control the disease. It is important to obtain proper health care in order to avoid possible birth defects or complications for the mother.
Diabetes types
There are primarily three types of diabetes. They are Type 1, Type 2, and gestational.
- Type 1 diabetes: This type is autoimmune in nature in which insulin production does not occur. It occurs because the beta cells of the islets of Langerhans in the pancreas undergo destruction. For this reason, this type is also known as insulin-dependent diabetes. It occurs most often during the teenage years and is therefore also called juvenile diabetes.
- Type 2 diabetes: This more common type is less severe than type 1. Although insulin is produced, production is not sufficient. Also, it is likely that the body might not use insulin, leading to insulin resistance. It is also known as non-insulin-dependent diabetes.
- Gestational diabetes: Blood glucose level rises during pregnancy to cause gestational diabetes. This kind most likely affects the baby and can cause severe complications if not treated early.
Physiology and Genetic Diabetes
Insulin plays a crucial role in diabetes. It is a hormone made in the pancreas to promote the absorption of glucose throughout the body.
Prior to diabetes, a condition called prediabetes occurs. Prediabetes usually tends to precede Type 2 diabetes and go unnoticed. During prediabetes, blood glucose levels goes up but not high enough to cause the full disease.
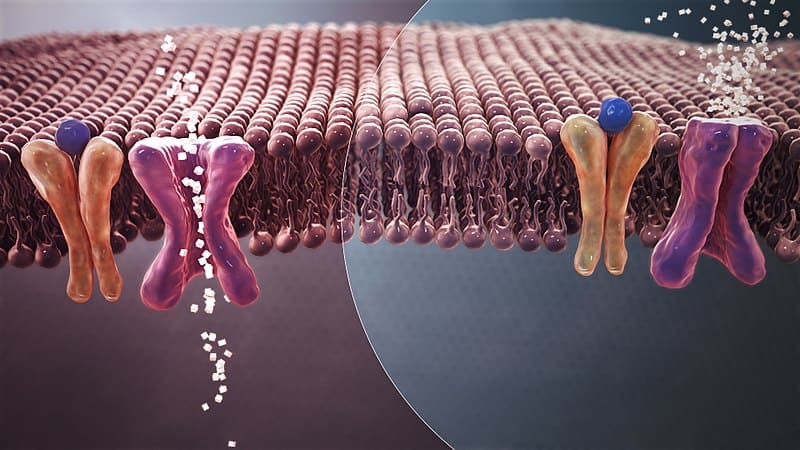
Mode of action of insulin
The digestive system breaks down complex carbohydrates (cereals, fruits, potatoes, etc.) into simple sugars, namely glucose. These sugars are then absorbed into the blood through the intestinal wall and distributed throughout the body. At the same time, the pancreas produces insulin in the β cells of the islets of Langerhans. Insulin causes glucose to be transported into the interior part of the cell.
Once inside the cell, glucose is consumed to produce energy in a process known as glycolysis. In addition, insulin also causes glucose to be stored in the form of glycogen in the liver as well as in the muscle cells. Hence, this keeps the blood sugar level constant within narrow limits (approx. 80-120 mg/dL or 4.5-6.7 mmol/L).
Even during long periods of fasting, blood sugar levels remains at a normal level due to the action of the liver. Glycogen previously formed in the liver is metabolized into glucose and released back into the blood. And on the other hand, the liver constantly produces glucose by a process known as gluconeogenesis.
In addition, insulin also has an adipogenic effect, aiding in the synthesis and storage of fat.
What happens during insulin shortage?
Sometimes, beta cells are unable to prepare sufficient amounts of insulin or no insulin at all. Thus, both the uptake of glucose into the body’s cells and the inhibition of glucose regeneration in the liver (which can produce up to 500 grams of new glucose daily in humans) is no longer possible.
When you have diabetes, your body experiences a rise in blood sugar levels, usually in the early morning. Either glucose remains in the blood, or the glucose production in the liver continues unchecked. A constant supply of glucose occurs, resulting in blood sugar level rises. Overall, it is a very complex and dynamic biochemical process in which synthesis, flux, and breakdown of glucose must be constantly balanced.
An increase in blood sugar compromises the body’s immune system. Hence, diabetic people are vulnerable to infections. Another common manifestation of severe, persistent insulin deficiency is weight loss.
This happens especially due to the utilization of the body fat and (muscle) protein for energy production. Although typically appetite is increased when your blood sugars are higher, which is why diabetes and obesity often occur together.
Mechanisms that lead to hyperglycemia are mainly based on insulin: absolute insulin deficiency, relative insulin deficiency due to insulin resistance, or both. Due to the long-term consequences of diabetes, the nervous and vascular systems undergo multiple changes.
Inheriting diabetes
Over two decades, reports have identified disease-associated genetic variants in populations worldwide. However, capturing the diversity of the population is important to understand the genetic architecture of diabetes.
Family members, such as a parent or sibling, with a history of type 1 diabetes is a potent risk factor in the development of the disorder in offspring. Much remains unclear when it comes to determining the extent to which family history and genetics plays a role in the development of type 2 diabetes.
Epidemiology
Type 2 diabetes is dominant in the majority of people with the disorder. As of 2019, diabetes has been responsible for 4.2 million deaths worldwide. Besides, 232 million diabetic people remain undiagnosed. Around 79% of diabetic people reportedly live in low and middle-income countries.
A rough estimate in 2018 described 1.5 million new cases in the United States. Incidence rates were higher in older adults than in young adults.
According to the 2020 update by the CDC, 34.2 million people are diabetic and account for 10.5% of the US population. And around 7.3 million people accounting for 21.4% of the diabetic population, remain undiagnosed.
Furthermore, prediabetes affects around 88 million of the adult US population of 18 years and over. This condition affects around 24.2 million people of age 65 years and above.
Factors associated with diabetes
A combination of various risk factors determines a person’s chance of developing both type 1 and type 2 diabetes.
Genetics of type 1 diabetes
To date, more than 50 genes have been identified that tend to be associated with the development of type 1 diabetes. Most of the gene alterations described are polygenic. This means that several genetic alterations must be present for type 1 diabetes to develop.
In particular, genetic alterations of the short arm of chromosome 6, the so-called MHC region, could be responsible for the development of type 1 diabetes. The genes HLA-A and HLA-B of this region contain the genetic information for cell-surface proteins of the immune system. This being said, the HLA genotype is essential in type 1.
Genes outside the HLA complex probably play a much smaller role in the genesis of type 1. These include the gene for insulin (INS) and the gene CTLA4, which is responsible for T-lymphocyte regulation.
Genetics of type 2 diabetes
The genetic risk of type 2 diabetes is not solely restricted to a single gene. In fact, multiple genes across the genome underline this type. Some of these genes that increase type 2 diabetes risk are TCF7L2, PPARG, IRS1, KCNJ11, WFS1, HNF1A, HNF1B, CAPN10.
Much about the interactions among these genes involved remains unclear. However, one of the few studies (in a population of Ashkenazi Jews) on genetic interplay has demonstrated that the TCF7L2-HNF4A and TCF7L2-WFS1 associations tend to increase the genetic risk of developing diabetes.
Environmental factors
In addition to the genetic component, environment and socio-economic status reportedly impacts the onset of type 2 diabetes. Although not causal, the physical environment, air pollution, and noise are linked with the increased incidence. Moreover, socioeconomic status is also associated with diabetes. For example, low socio-economic status has been attributed to about 40% – 60% of risk.
DNA viruses and RNA viruses have the potential to destroy cells in the pancreas, thereby interfering with insulin metabolism. Studies in mice have proved that such auto-immune disruption causes type 1. In another example, the Hepatitis C Virus that causes hepatic steatosis and insulin resistance may also lead to type 2.
Diet and lifestyle
Food intake is directly related to the development of type 2 diabetes. People who consume high amounts of saturated fats in some foods have a higher risk of developing the disease. On the other hand, micronutrients such as vitamins, magnesium as well as antioxidants like β-carotene might help reduce the risk. Lifestyle factors such as eating habits, insomnia, stress, and lack of physical activity correlate positively with diabetes.
Microbiome
The gut microbial composition is linked with diabetes and this is often accounted for by dysbiosis. In dysbiosis, the relative abundances of certain groups of microbes in diabetic people differ from those of non-diabetic people.
As an example, in a study cohort, Firmicutes decreased in relative abundance while Bacteroidetes and Betaproteobacteria increased in abundances in diabetic people. The researchers conducted this study to assess the bacterial communities via pyrosequencing.
In another study via a metagenome-wide association study, researchers observed a moderate extent of gut dysbiosis. However, infection-causing bacteria were higher in number while some butyrate producers showed a marked decrease.
If you want to learn more about your personal gut health, you could take a gut microbiome test to look at the DNA of microbes in your gut. Many are available such as:
- Biohm (gut health, including bacteria and fungi)
- DayTwo (gut health, personalized recommendations for blood glucose optimization)
- Onegevity (gut health and personalized recommendations)
- Psomagen (gut health and gene test)
- Rootine (personalized supplement and vitamins based on DNA test)
- Sun Genomics (gut microbiome testing and personalized probiotics for adults, children, and infants)
- Ombre (formally Thryve) (personalized probiotics)
- Viome (gut health and microbiome testing)
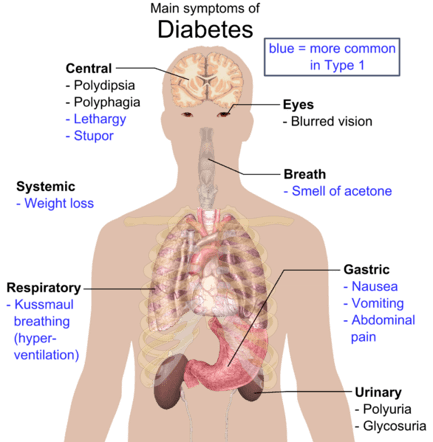
Symptoms
A number of symptoms are common to both type 1 and type 2 diabetes. Symptoms of diabetes include frequent hunger pangs, severe fatigue, frequent urination, dry skin and blurred vision, and slow healing of wounds.
Few specific symptoms:
Type 1 – People with this type find that the most obvious symptom of type 1 diabetes is weight loss. Besides, diabetic ketoacidosis is also an apparent symptom. In this condition, a build-up of ketones occurs thereby causing nausea and vomiting. This type mainly occurs in adolescence.
Type 2 – Yeast infection generally accompanies this type of diabetes. Usually, adults of over 40 years of age are at risk of developing type 2.
In a national survey, researchers found that patients who had been diagnosed with diabetes as middle age individuals (defined as 40-64 years) suffered from very different health problems than those diagnosed with type 2 diabetes later in life or earlier. For example, middle age diagnosed patients tended to have more cases of retinopathy, high blood pressure and cholesterol, and worse control over blood sugar. High blood pressure and cholesterol often predispose a person to heart disease as well.
Did you know you can test for both heart disease and cholesterol levels at home? Learn more on our blog!
Long term complications of diabetes
Diabetes plays a strong role in further developing a series of other health complications.
Skin problems
Specific skin problems include the following:
- Acanthosis nigricans: The folds of necks, armpits, genital areas develop pigmented patches. Overweight people are most likely to experience this condition.
- Diabetic dermopathy: Due to the changes in blood vessels, several pigmented circular, scaly patches form on the skin.
- Necrobiosis lipoidica diabeticorum: This is a rare condition similar to diabetic dermopathy, however, the spots are fewer and larger.
- Eruptive xanthomatosis: In this problem, the skin develops firm, yellow, pea-shaped blisters. And they are quite itchy. People with high levels of cholesterols in blood experience this condition.
- Calluses and ulcers: Due to poor circulation in diabetic people, callus formation escalates. Plus, the chances of developing foot ulcers follow.
Vision problems
Three specific diseases are common:
- Glaucoma: In glaucoma, pressure in the eye blood vessels interfere with the blood transport to the retina and optic nerve.
- Cataracts: Although non-diabetic people do develop cataracts, diabetics are most likely to develop this condition. In this condition, clouding of the lens occurs that severely impacts vision.
- Retinopathy: In the non-proliferative retinopathy, blocked blood vessels lead to leaking of the fluid into the macula. Following this, the macula swells up and ultimately causes blurry or lost vision. In proliferative retinopathy, complete damage of blood vessels occurs.
This damage induces new but weak blood vessel formation. Eventually, these new blood vessels start leaking blood and cause lost vision.
Nervous system damage
- Peripheral neuropathy: This causes numbness, pain, and weakening of hands and feet.
- Autonomic neuropathy: It damages the autonomic nerves regulating bladder and intestinal activities. This type of neuropathy is a common complication.
Type 2 diabetes and digestive and kidney diseases
Genetic factors, blood sugar, blood pressure determine the onset of kidney disease and kidney failure. In cases when this condition occurs, fluid build-up in the kidney is followed by poor appetite, upset stomach and severe weakness. You can learn more about the research and resources concerning these co-occurring health conditions through the National Institute of Diabetes and Digestive and Kidney Diseases (a part of the National Institutes of Health).
Diagnosis
At present, genetic testing is not universally available to health-care providers. The doctor makes the diagnosis mainly on the basis of the blood sugar level.
A1C Test
The A1C assay measures an average of the blood glucose level over the past three months. It is also known as glycohaemoglobin test. That is because it relies on the binding of the glucose to hemoglobin.
A higher concentration of blood glucose indicates a higher binding pattern. And such results are usually provided in the form of percentages.
Fasting Plasma Glucose Test
In this test, the doctor measures the blood glucose levels after 8 hours of fasting. This is one of the most preferred tests in diagnosis.
Oral Glucose Tolerance Test
It measures the blood glucose level after fasting overnight. Next, the consumption of a sugary liquid follows. After this, the doctor measures the blood glucose level over the next 2 hours.
| Condition | A1C Test | Fasting Plasma Glucose Test | Oral Glucose Tolerance Test |
| In normal condition | Less than 5.7% | Less than 100mg/dL | Less than 140mg/dL |
| In diabetes | 6.5% and higher | 126mg/dL and higher | 200mg/dL or higher |
Treatments
Diabetic patients should pay attention to their blood sugar levels. Treatments from a team of endocrinologists, ophthalmologists, nutritionists, etc. are also important to treat this condition.
Drugs
The prescribed drugs act via a number of mechanisms. For example, some drugs increase insulin production while others decrease intestinal glucose absorption. There are few other drugs that often improve the way in which the body uses insulin and improves insulin resistance. A number of drugs also inhibit glucose reabsorption into the kidney.
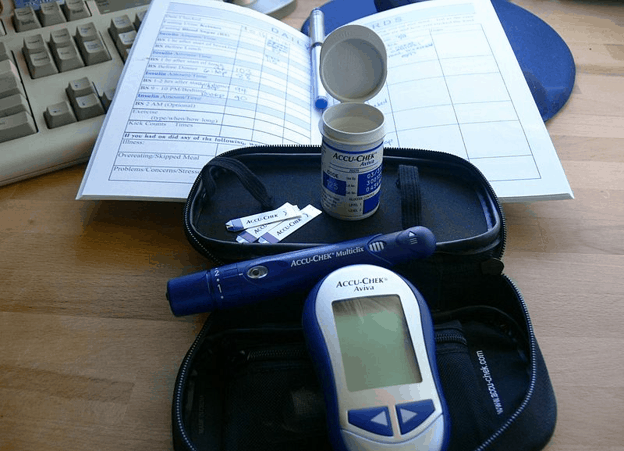
Diet and lifestyle management
A balanced diet, timing, and quantity of the food you eat also matters in order to allocate proper insulin dose. Other than these points, exercise is crucial for diabetic patients. It also provides relief from stress. Plus, the doctors often prescribe a glucose meter for measuring the blood glucose level as part of a patient’s diabetes care.
Are you interested in delving deeper into the genetics of diabetes? You should visit the Genetics Home Reference, which was merged into Medline Plus in September 2020. And for more resources and support, you can explore the American Diabetes Association.
You can find more diabetes reports on our website. If you liked this article, you should check out our other posts in the Nebula Research Library!
July 9, 2022
