Table of contents
Nebula Genomics DNA Report for Glaucoma
Is glaucoma genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Glaucoma?
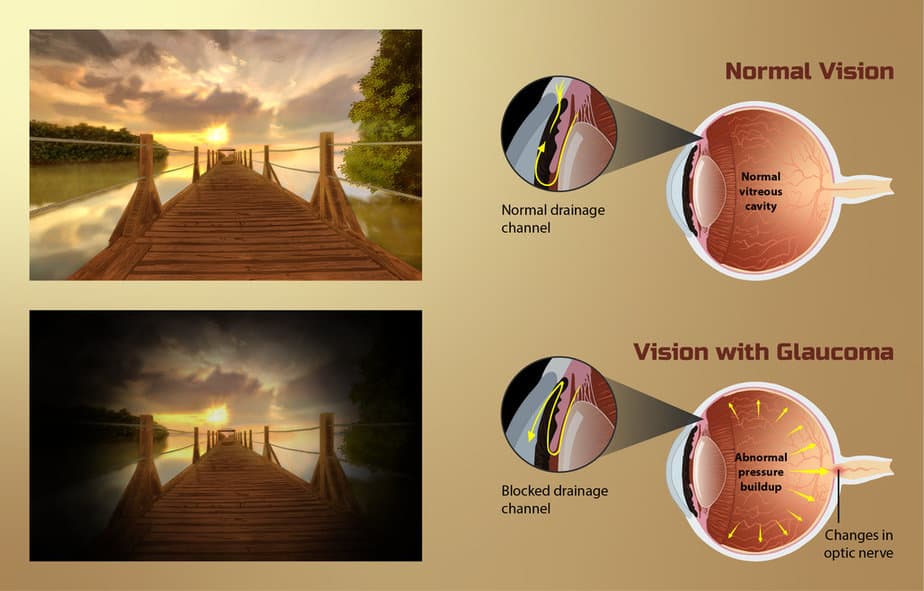
Glaucoma is a term that refers to a number of ocular diseases of different causes that result in irreversible damage to the optic nerve (the bundle of nerve fibers that carries information from the eye to the brain). This damage eventually causes the patient to lose vision. In most cases, fluid builds up in the eye, causing increased pressure that leads to optic nerve damage. It is one of the leading causes of blindness for people over 60.
One of the first studies that observed this connection between intraocular pressure and glaucoma was published in Arch Ophthalmol in 1991. in Invest Ophthalmol Vis Sci published additional investigations into the disease in the following years.
Types
There are eye abnormalities in all major forms of glaucoma:
Open-angle (wide-angle, chronic simple) glaucoma: This is the most common type of glaucoma and often results from increased eye pressure (although it can happen at normal eye pressure as well). In this type, the fluid drainage angle within the eye remains open. It occurs gradually over time with no pain.
People with open angle glaucoma notice that their side vision generally declines first, followed by the central vision. Blindness will occur if left untreated. There are specific forms of this system such as exfoliation syndrome, in which abnormal accumulation of a certain protein affects the drainage of the eye.
Closed-angle (narrow-angle glaucoma, acute congestive) glaucoma: This form of the condition is uncommon. It can occur gradually or suddenly. When sudden, symptoms may occur, including severe eye pain, blurred vision, dilated pupil, eye redness, and nausea. This type of closed angle glaucoma is a medical emergency and doctors need to release the pressure quickly.
As with open-angle glaucoma, blindness will occur if left untreated. The risk of angle closure glaucoma increases with age, family history, Chinese or Inuit ancestry, far sightedness, and being a biological female.

Normal-tension glaucoma: This form of the condition is uncommon. It occurs due to optic nerve damage.
Secondary glaucoma can occur if the cause of increased eye pressure is known, such as by injury, inflammation, certain drugs such as steroids, and advanced cases of cataracts or diabetes.
The condition affects most people in both eyes, although initially, it might be worse in one eye over the other. Once blindness occurs, it cannot be reversed.
Risk factors
Risk factors may include increasing age, high pressure in the eye, a family history of glaucoma, and the use of steroid medication. Doctors generally check eye pressures at standard vision exams. Pressures of 21 mmHg or 2.8 kPa above atmospheric pressure (760 mmHg) are considered high. High eye pressures may put a patient at greater risk of glaucoma, while others have consistently high eye pressures and never develop the condition.
An ophthalmologist usually makes a diagnosis of this condition with a dilated eye examination, where they view the optic nerve. Although there is no cure, treatment involving laser therapy or surgery can slow or stop the progression if diagnosed early.
Is Glaucoma Genetic?
Glaucoma can be hereditary, and it tends to run in families. There are also several genetic risk factors related to glaucoma.
Studies have identified several genetic mutations that can increase glaucoma risk. However, experts have not identified one gene variant as the cause, and increased susceptibility is likely a combination of genetic influences. These specific genes in relation to adult onset forms of the condition include caveolin 1 and 2 (CAV1/CAV2), CDKN2B antisense RNA, TMCO1, SIX1/SIX6, LRP12/ZFPM2, TBK1 and GALC genes in the case of open-angle forms of the condition. Other genes, including PLEKHA7, PCMTD1/ST18, and COL11A1, are associated with the closed-angle form.
Glaucoma in children
Some forms of glaucoma that affect young children are genetic.
An example of this is primary congenital glaucoma. This is the most common childhood form of the condition from birth to age 3. Scientists have associated autosomal dominant gene mutations in CYP1B1 with many cases worldwide. However, it is only found in 15% of children in the United States with the condition, so research is ongoing to identify additional factors.
This gene provides instructions for producing a form of the cytochrome P450 protein, which is located in structural components of the eye. Doctors have found the mutation in some cases of juvenile open-angle glaucoma (when the condition occurs in childhood or early adulthood).
Approximately 10-33% of people with juvenile glaucoma have mutations in the MYOC gene. This gene encodes instructions for the protein myocilin, which appears in structures regulating intraocular pressure. These mutations may also be associated with the primary congenital form of the condition.
CYP1B1 may interact with MYOC and inheriting both of these mutations may lead to earlier onset of the condition and/or more severe symptoms.
Genetic testing can help you or your children discover whether you are at a higher risk of developing the condition and take steps to monitor for the disease.
Current Research on Genetic Glaucoma
In 2017, Human Molecular Genetics published an article about genetic glaucoma. This paper resulted from a series of genetic and genomic studies on the discovery of genes contributing to glaucoma. In addition, it lists the mutations linked to molecular and cellular events that lead to the onset of the disease.
At the turn of the century, an estimated 3 to 6 million people in the United States were at risk of developing primary open-angle glaucoma (POAG) because of elevated intraocular pressure (IOP). The Ocular Hypertension Treatment Study was a trial study that began in February 1994 and was completed in 2019.
If you would like to learn about testing for risks to developing primary angle-closure glaucoma (PACG), check this article on non-contact tests.
This paper shows the roles of animal models in glaucoma research. Rodents and non-human primates have been important to insights into how to treat the condition more effectively.
Epidemiology
About 3 million people in the United States have glaucoma and 2.7 million are those over 40 with primary open-angle glaucoma. Doctors use the term early-onset glaucoma when the disorder appears before the age of 40. Worldwide, it is estimated that 57.5 million people are affected by this type, which is the most common form of glaucoma.
Overall, it is the second leading cause of blindness after cataracts.
The condition is three to four times more common in African Americans than in non-Hispanic Whites and is fifteen times more likely to cause blindness than in Caucasians.
Symptoms
In the early stages of glaucoma, most people don’t realize that they have open-angle glaucoma since there are no symptoms.
Typically, the first sign of glaucoma is loss of peripheral or side vision. Since glaucoma damages optic nerve fibers, blind spots in your vision begin to appear.
Vision loss tends to occur gradually, and glaucoma patients may not notice it for years. This initial loss will happen in the peripheral vision. By the time doctors detect significant vision loss, the condition has usually already progressed into permanent damage.
In later stages, symptoms include:
- Hazy or blurred vision
- Rainbow-colored circles around bright lights
- Severe eye and head pain
- Nausea or vomiting (accompanying severe eye pain)
- Sudden sight loss
In the closed-angle form of the disease, symptoms tend to be very noticeable and damage occurs quickly. However, there are cases in which the angle is closed, but the eye pressure may or may not be high, and the optic nerve is not affected yet.
Causes
People can get the condition at any age, but the risk of developing glaucoma increases as you get older. African American or Hispanic patients also have a higher risk and are more likely to develop the condition earlier in life.
Certain non-eye-related situations are risk factors for glaucoma. Other risk factors that play a key role in glaucoma include abnormalities in the eye and diseases that irreversibly damage the eye:
- Diabetes
- Family history of the disease
- Farsightedness (closed-angle glaucoma)
- Nearsightedness (open-angle glaucoma)
- High blood pressure (hypertension)
- Long-term use of corticosteroids
- Previous eye injury or surgery
Although the condition can occur without an identified cause, the most critical factor is intraocular eye pressure. Fluid naturally covers the eye to keep it hydrated and leaves through the drainage canal between the iris and cornea. If the canal becomes blocked, it leads to a buildup of fluid in the eye, which causes increased pressure and eventual damage to the optic nerve, ultimately leading to the condition.
Diagnosis
The condition is not always easy to diagnose. In most cases, doctors use a comprehensive eye examination to diagnose glaucoma. The five most common tests will include:
- Tonometry: measures the intraocular pressure
- Dilated eye exam: tests for optic nerve damage
- Visual field test: checks for areas of vision loss
- Pachymetry: measures corneal thickness
- Gonioscopy: inspects the drainage angle
If a diagnosis is challenging, doctors may referr people with glaucoma to a specialist.
To have the best chance of early detection, you should have your regular eye exams. Most people start baseline screenings at age 40, as this is the most common time in which early symptoms of glaucoma appear. Your eye doctor will recommend a frequency of screening based on your exam and risk factors.
Treatment
There is no cure, but glaucoma treatments can prevent vision loss from getting worse, especially if doctors catch the condition early. The main goal of all treatments is to lower eye pressure.
Eyedrops
Prescription eye drops are usually the first course to treat glaucoma. These drops, depending on the type, may be used to improve how well the fluid drains from your eye or decrease the amount of fluid your eye makes, both strategies to reduce the pressure. Depending on the drops, instructions may be to use them once or up to three times a day. Some examples of these treatments include:
Prostaglandins: increase the outflow of the fluid in your eye. Doctors prescribe this class of drug for once-a-day use.
Beta-blockers: reduce the production of fluid in your eye. Doctors prescribe these once or twice daily depending on your condition.
Alpha-adrenergic agonists: increase the outflow of the fluid in your eye. Doctors prescribe these two or three times per day.
Carbonic anhydrase inhibitors: reduce the production of fluid in your eye. Doctors prescribe these two or three times per day.
Eye drops are absorbed into your bloodstream, causing side effects unrelated to your eye. You can often minimize this absorption by closing your eyes for 1-2 minutes after application or pressing lightly at the corner of your eyes.

Oral medications
If eye drops are not enough to lower eye pressure, your doctor may recommend an oral medication containing a carbonic anhydrase inhibitor, which reduces the fluid. Possible side effects include frequent urination, tingling in the fingers and toes, depression, stomach upset, and kidney stones.
Surgery
Surgeries will aim to improve fluid drainage from the eye, reducing pressure. Some examples of options include:
Laser therapy: Used to treat open-angle glaucoma, your doctor will use a tiny laser beam to open clogged channels in the eye.
Filtering surgery: In this procedure, your surgeon creates an opening in the white of the eye and removes part of the trabecular meshwork (eye tissue).
Drainage tubes: a small tube shunt is inserted into your eye to drain away excess fluid to lower your eye pressure
Minimally invasive glaucoma surgery (MIGS): There are several options in this category that are less invasive and complicated than the other surgical options. These are often combined with cataract surgery.
Follow-up exams after surgery are necessary to determine if additional treatment is needed in the case that the pressure begins to build again.
Unlike open-angle glaucoma, closed-angle glaucoma comes on suddenly and is a medical emergency. Urgent medication and surgical procedures are often used. Sometimes, this includes an iridotomy, where your doctor uses a laser to create a small hole in your iris to release fluid and thus the pressure.
If you liked this article, you should check out our other posts in the Nebula Research Library!
March 16, 2023
