Table of contents
Nebula Genomics DNA Report for Addison’s Disease
Is Addison’s disease, a condition affecting the adrenal glands, genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Addison’s Disease?
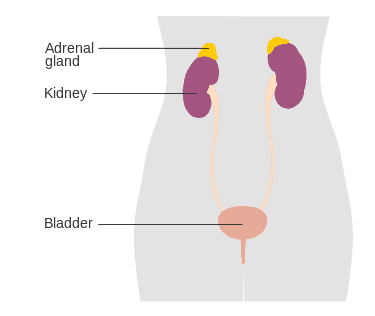
Primary adrenal insufficiency (Addison’s disease) is a rare disease experts characterize by long term endocrine issues. Notably, the adrenal glands, which sit on top of the kidneys, do not produce enough of the steroid hormones, cortisol and aldosterone. Secondary adrenal insufficiency occurs when the pituitary gland doesn’t make enough of the hormone ACTH. The condition is named after Thomas Addison, the first physician to identify it in the medical literature in 1855.
Addison’s disease may occur by itself or as part of a large disorder specifically the autoimmune polyendocrine syndrome type I (APS type-1) and type II (Schmidt syndrome).
Symptoms usually appear gradually and may include abdominal pain and gastrointestinal abnormalities, weakness, and weight loss. Other symptoms to look out for include darkening of the skin, low blood pressure, vomiting, lower back pain, loss of consciousness, and mood swings.
Signs that come on suddenly can indicate acute adrenal failure, which is a potentially life threatening medical emergency. Patients can trigger such failure, or adrenal crisis, when the body responds to stress, such as from a surgery, injury, or infection. In case of adrenal failure, patients should seek medical care immediately.
Addison’s disease is normally classified as an autoimmune disease, in which the body attacks healthy tissues. Doctors can diagnose it through blood tests, urine tests, and/or medical imaging.
Treatment involves replacing the missing hormones with synthetic corticosteroid, which occurs for the rest of your life. In most cases, patients take these hormone replacement therapies by mouth although serious cases of the condition may require injections. Patients receive regular followup monitoring for worsening symptoms or other conditions.
Is Addison’s Disease Genetic?
The condition appears to run in families to some extent. Overall, experts believe that both genetic and environmental factors lead to the disease and the genetics are complex.
Scientists think the genetic variants in Addison’s disease are largely based in the immune system. The most commonly associated genetic variations are those in the human leukocyte antigen (HLA) complex. This complex is an autoimmune regulator, helping the body distinguish between the body’s proteins and those made by foreign invaders. The most well-known risk factor for autoimmune Addison disease is a variant of the gene called HLA-DRB1. The dysregulation of this gene, along with potentially many others, causes the immune system to function incorrectly.
A 2021 study conducted by researchers at Karolinska Institutet, Sweden, and Bergen University, Norway noted increased genetic risk of Addison’s disease in patients with nine variants in the AIRE gene, which helps in the proper functioning of T cells.
It has been shown that you are at higher risk of developing genetic Addison’s disease if you or a close family member have another disease affecting the autoimmune system, such as vitiligo, type 1 diabetes, and hypothyroidism.
Epidemiology
According to the National Organization for Rare Disorders (NORD), approximately 1 in 100,000 people in the United States have Addison’s disease. Experts estimate the overall prevalence as 40 to 60 people per million of the general population. However, this number may be inaccurate as there is expected to be many undiagnosed instances in the population.
The condition affects males and females at the same rate. Although people of any age can develop Addison’s disease, it is most likely to occur in individuals between the ages of 30-50.
Symptoms
Symptoms of Addison’s disease tend to appear slowly and thus can be easily overlooked. Because of this, the first time someone may be aware of their condition can occur during an Addisonian crisis. You may want to discuss the possibility of this condition if you regularly feel tired, weak, or are losing weight. The other most common symptoms include muscle weakness and abdominal pain.
Other symptoms include:
- nausea
- vomiting
- diarrhea
- low blood pressure that drops further when you stand up, causing dizziness or fainting
- irritability and depression
- joint pain
- craving salty foods
- hypoglycemia, or low blood glucose
- irregular or no menstrual periods
- loss of interest in sex
- darkening of skin

Causes
Adrenal glands that do not produce enough of the hormones cortisol and aldosterone cause this condition. Damage to the outer layers of the adrenal glands is usually an underlying factor.
Cortisol helps the body respond to physical and mental stress and also helps maintain blood pressure, heart function, the immune system, and blood glucose (sugar) levels. Aldosterone affects the balance of sodium and potassium in the blood. This has a direct effect on kidney function.
This adrenal disease is an autoimmune disorder. In this case, the body mistakenly attacks the outer portion of the adrenal glands, sites of hormone production. Once the body damages 90% of these glands, symptoms are usually noticeable.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), tuberculosis (TB) is the most common cause of Addison’s disease worldwide, although it is much more common in underdeveloped countries. TB is a bacterial infection in the lungs that can spread to other parts of the body, such as the adrenal glands.
Other possible causes include:
- Infections caused by AIDS or fungus
- Bleeding in the adrenal glands, caused by meningitis or other types of severe sepsis
- Cancer in the adrenal glands
- Surgical removal of the adrenal glands
- Fungal infections
Diagnosis
The Mayo Clinic for Medical Education and Research notes that diagnosis is based on symptoms and a medical history, including whether certain autoimmune disorders run in your family. Doctors can then confirm it with various diagnostic tests
Blood tests: Through these tests, doctors will measure levels of sodium, potassium, cortisol and adrenocorticotropic hormone (ACTH), which stimulates the adrenal cortex to produce its hormones, in the blood. Low sodium, high potassium or low cortisol level may indicate Addison’s disease. The tests can also measure antibodies that can be a sign of the condition.

ACTH stimulation test: If cortisol is low, doctors may be able to confirm a diagnosis with this test. ACTH is the cortisol-stimulating hormone produced by the pituitary gland at the base of the brain. The test compares the level of cortisol in your blood before and after an injection of ACTH. Doctors usually confirm the disorder if the ACTH level is high but the cortisol and aldosterone levels are low.
Imaging: CT scans or MRos of your adrenal glands can help determine abnormalities that may be causing the disease.
Thyroid test: Patients with Addison disease often have hypothyroidism, which occurs when the thyroid does not produce enough hormones. Doctors often perform this test if they suspect Addison’s disease.
Treatment
The standard treatment for Addison’s disease is hormone replacement therapy, to replace the hormones that the adrenal glands are not producing.
Hydrocortisone (Cortef), prednisone, or methylprednisolone replace cortisol while fludrocortisone acetate replaces aldosterone. Doctors prescribe the former on a strict schedule to mimic the natural fluctuations of this hormone in the body.
Additional medication is often prescribed if your body is undergoing a lot of stress, such as from a surgery. Doctors normally only recommend the injected forms of the replacement hormones if you are unable to take the oral forms.
It is also recommended that patients get plenty of extra salt (sodium) in their diet, especially during heavy exercise, when it is hot, or if they are having gastrointestinal issues.
People with this disorder will often see a health care specialist called an endocrinologist. It is important for patients to keep regular checkups with their doctors, at least one per year, to monitor for worsening symptoms. Your doctor may also recommend regular screenings for other autoimmune disorders.
In case of acute adrenal failure, intravenous injections of corticosteroids, saline solutions, and sugar (dextrose) are used to quickly replace these missing components.
If you liked this article, you should check out our other posts in the Nebula Research Library!
June 11, 2022
