Nebula Genomics DNA Report for Fibromuscular Dysplasia
Is fibromuscular dysplasia genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
What is Fibromuscular dysplasia?
Fibromuscular dysplasia (FMD) is a rare systemic vascular disease affecting the arteries. This coronary artery disease causes abnormal growths or deformities in artery walls. This effect can lead to stiffening, narrowing (stenosis), or enlargement (aneurysm) of the affected blood vessels. If an artery is too stiff it will be unable to function when blood runs through it, which could lead to high blood pressure. On the other hand, if it is too weak, it can dilate and lead to an artery aneurysm.
Fibromuscular dysplasia can affect any artery in the body. Most commonly, it affects those leading to the kidneys and brain. However, artery involvement may also affect the neck, abdomen, and legs.
Types
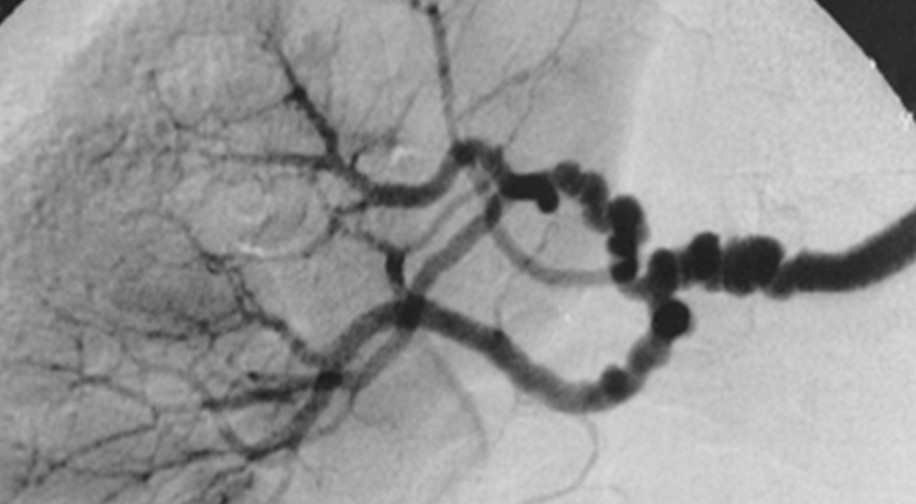
There are two types of FMD: Multifocal and focal. The former is more common and causes affected arteries to look like a string of beads with a repeated pattern of narrowing and bulging. This form represents areas that are too stiff and too week. Focal fibromuscular dysplasia is less common and involves abnormal area of tissue on the artery wall.
The exact cause of fibromuscular dysplasia is unknown, but it is believed to be a combination of genetic and environmental factors. It can occur at any age, but is more common in women around 50. Symptoms can vary depending on the affected artery. Complications include high blood pressure, headaches, dizziness, ringing in the ears, vision changes, abdominal pain, and leg pain.
A doctor may use a physical exam or imaging tests such as an ultrasound, CT scan, MRI, or biopsy to diagnose the condition. There is no cure for fibromuscular dysplasia, but treatment options aim to manage symptoms and prevent complications. Treatment may include medications to control blood pressure or manage pain, procedures to widen or bypass the affected arteries, or surgery in severe cases.
Is Fibromuscular Dysplasia Genetic?
Several studies suggest a genetic basis for FMD, as it can run in families. Additionally, specific genetic mutations have been associated with the condition. However, the inheritance pattern is unclear, as it can occur sporadically or be inherited in an autosomal dominant or autosomal recessive pattern depending on the underlying genetic mutation. It is important to note that not all cases of fibromuscular dysplasia have a clear genetic basis. Other factors, such as hormonal changes and smoking, have also been linked to its development.
Olin JW et al published one of the most comprehensive reports on the science of the condition in 2014.
In 2020, a paper published in Hypertension sought to link the PHACTR1 gene with FMD. While the authors did find an association, their study was limited by the small cohort and lack of significance after multiple testing corrections.
Authors of a 2021 paper published in Nature Communications reported the first genome-wide association meta-analysis of six studies to identify five genome wide significant loci potentially involved in the genetic cause of fibromuscular dysplasia. The genome-wide association study pinpointed locations previously been associated with multiple vascular disorders. The genes include PHACTR1, LRP1, ATP2B1, LIMA1, and SLC24A3. The risk genes for FMD were usually expressed in smooth muscle cells, fibroblasts, and arterial tissues.
You can read more about this paper in this commentary, with voices by the University of Michigan Health Frankel Cardiovascular Center.
Epidemiology
Experts do not entirely understand disease prevalence due to its rarity and the lack of symptoms in many people. Studies based in the United States estimate it affects 12 out of 100,000 individuals, with a much higher prevalence in women than men. Doctors typically diagnose FMD cases in middle-aged individuals, with a peak incidence when people are in their 50s and 60s. It can also affect younger women and accounts for 10% to 20% of the cases of renal artery stenosis.
Fibromuscular dysplasia can occur sporadically or familial, with a reported prevalence of up to 20% in first-degree relatives of affected individuals. Familial FMD is most commonly inherited in an autosomal dominant pattern, but other ways of inheritance have also been described. Fibromuscular dysplasia is also more common among people with certain connective tissue disorders (e.g., Ehlers-Danlos syndrome).
The paper above also cites the prevalence of renal FMD as 0.4 %, whereas craniocervical fibromuscular dysplasia is much lower at 0.1%. Among older hypertensive FMD patients who underwent renal angiography, scientists saw a prevalence of 5.8%.
Symptoms
Fibromuscular dysplasia is a cardiovascular disease that causes narrowing and enlargement of medium-sized arteries. The symptoms may vary depending on the location and severity of the disease.
Some individuals with fibromuscular dysplasia may not experience clinical manifestations, while others may develop serious complications.
The two most common symptoms for those who experience fibromuscular dysplasia of the renal arteries are high blood pressure (hypertension) and poor kidney function. Many patients with FMD will have renovascular hypertension, a renal arterial disease.
If the condition affects the carotid and vertebral arteries leading to the brain and neck, patients with the carotid artery version most likely experience migraine headaches, tinnitus, dizziness or vertigo, and neck pain. When serious, fibromuscular dysplasia can cause serious complications such as aneurysm ruptures, spontaneous coronary arterial dissection (SCAD), stroke, or a transient ischemic attack (TIA or mini-stroke). Stroke in fibromuscular dysplasia is associated with cervical artery dissection, which occurs when there is a tear in a carotid or vertebral artery.
Causes
The exact cause of fibromuscular dysplasia is poorly understood, but it is believed to be a complex interplay of genetic and environmental factors.
Some genetic factors that experts believe may be associated with FMD include mutations in genes that code for proteins involved in the structural integrity of arterial walls. These mutations can cause abnormal development of arterial walls, leading to the characteristic fibrous and muscular tissue changes seen in fibromuscular dysplasia. Although research is still being conducted, experts have observed that some cases may run in families.
Consistent with the observation that females are at greater risk, doctor believe that sex-specific hormones are risk factors for the disease development. Variables related to pregnancy do not appear to increase risk.
Environmental factors, such as smoking, may also play a role. When patients are diagnosed with the condition, smoking may make it worse.
Fibromuscular dysplasia can also occur as part of other underlying medical conditions, such as neurofibromatosis type 1 and Alport syndrome, but these cases are relatively rare.
Diagnosis
Diagnosis of FMD can be challenging, as the symptoms may be nonspecific or may not appear until the disease has progressed. Doctors often detect it incidentally during imaging studies performed for other conditions. Sometimes, a patient will only learn of it after suffering a life-threatening event like an aneurysm.
A doctor may start with ordering blood tests for related conditions, such as atherosclerosis, that can narrow arteries.
To diagnose fibromuscular dysplasia, the doctor will usually perform a physical exam, review the patient’s medical history, and order imaging tests to evaluate the arterial structure and blood flow. These tests may include ultrasound, magnetic resonance angiography, and computed tomography angiography.

The healthcare provider may also order additional tests to evaluate the function of the affected organ, such as a renal function test or cardiac stress test.
Treatment
While there is no cure for the condition, treatments can manage the symptoms and prevent complications. Fibromuscular dysplasia treatment depends on the location and severity of the disease, as well as the presence of any complications or symptoms.
Antiplatelet or anticoagulant therapy: These medications thin the blood, which can reduce the risk of blood clots or stroke.
Blood pressure control: If the condition causes high blood pressure, the first line of treatment is often medications to lower blood pressure, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or calcium channel blockers.
Angioplasty and stenting: In some cases, balloon angioplasty (a procedure that uses a balloon to widen the narrowed artery) and stenting (placing a small mesh tube to keep the route open) may be performed to restore blood flow in the affected artery.
Surgery: In severe cases or when other treatments are ineffective, doctors may use surgery to repair or bypass the affected artery.
It is important to note that FMD is a chronic condition, and lifelong monitoring and management are often necessary. Doctors often recommend annual imaging studies and lifestyle changes such as quitting smoking, reducing salt, and daily exercise.
If you liked this article, you should check out our other posts in the Nebula Research Library!
October 17, 2023
