Nebula Genomics DNA Report for Migraines
Are migraines genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of September 2021 |
Table of contents
- Nebula Genomics DNA Report for Migraines
- What are Migraines? (Part 1 of Are migraines genetic?)
- Are Migraines Genetic?
- Current Research on Migraines
- Epidemiology (Part 3 of Are migraines genetic?)
- Symptoms (Part 4 of Are migraines genetic?)
- Causes (Part 5 of Are migraines genetic?)
- Diagnosis (Part 6 of Are migraines genetic?)
- Treatment (Part 7 of Are migraines genetic?)
What are Migraines? (Part 1 of Are migraines genetic?)
A migraine is a common neurological disease typically characterized in adults by intense, recurrent, throbbing, and pulsating headaches on one or more sides of the head that can range from mild to severe. These types of headaches may be accompanied by additional symptoms such as nausea, vomiting, sensitivity to bright lights (photophobia), or sound (phonophobia). It can also worsen through exposure to physical activity and smell.
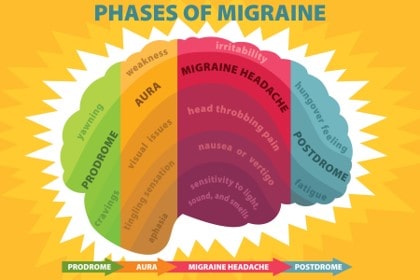
No matter the type, the condition is usually divided into four distinct stages: the period leading up to the headache (the premonitory or prodrome phase), the aura, the headache phase, and the period following the headache (the postdrome phase).
Types
There are several distinct types of migraine headache based on its physical symptoms. Migraine symptoms may include:
- Migraine with aura: Around 15% to 20% of people who have this condition experience an aura before the headache. An aura is described in “Symptoms” below.
- Migraine without aura: This type occurs without the warning of an aura.
- Migraine without head pain: A “silent migraine” or “acephalgic migraine” includes the aura symptom but not the headache that typically follows.
- Hemiplegic: This type causes temporary paralysis or neurological or sensory changes on one side of your body. Onset may be associated with temporary numbness or weakness on one side of your body, a tingling sensation, a loss of sensation, and dizziness or vision changes. A headache may or may not occur.
- Retinal: You may notice temporary, partial, or complete loss of vision in one of your eyes, along with a dull ache behind the eye that may spread to the rest of your head. Retinal migraines may be a sign of a more serious issue.
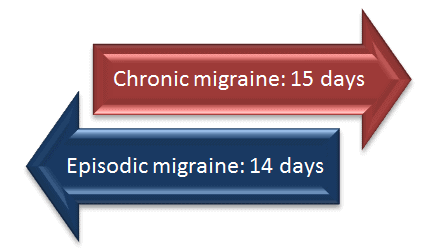
- Chronic migraine: A chronic migraine is when it occurs at least 15 days per month. The symptoms and severity may change frequently.
- Migraine with brainstem aura: This type will often cause vertigo, slurred speech, double vision, or loss of balance, which occur before the headache. The headache pain may affect the back of your head. These symptoms usually occur suddenly and can be associated with the inability to speak properly, ringing in the ears, and vomiting.
- Status migrainosus: This is a rare and severe type that can last longer than 72 hours. The migraine pain and nausea can be extremely bad. Certain medications, or medication withdrawal, can cause you to have this type of migraine.
These conditions can last from a few hours to a few days. About one-third of patients also experience a distinct range of sensory events right before the headache phase called an aura. Some of the most common symptoms of this experience include temporary visual changes such as blind spots, flashing lights, and zigzag lines of color. Motor disturbances are also possible.
The cause is usually attributed to both environmental and genetic factors. Although the underlying mechanisms are unknown, it is suspected to be associated with the nerves and blood vessels in the brain. There is no blood test or other procedure, and diagnosis is usually made with the help of a medical history after excluding other diseases as causes.
Are Migraines Genetic?
These episodes are thought to be a combination of genetic and environmental factors. There are many genes involved to various degrees, most of them associated with the muscles that surround blood vessels in the brain. These genes regulate blood flow to the brain by widening or narrowing the vessels. Genes that affect certain neurotransmitters like glutamate and the activity of certain nerve cells have also been identified.
While the inheritance pattern is unknown, most people with the condition will have a family member who is also affected.
Familial hemiplegic migraine is a specific form of migraine known to run in families. Like other types, the condition is more common in women than men. Four genes were found to be associated with this type of genetic migraines:
CACNA1A, ATP1A2, and SCN1A: These genes encode for proteins responsible for the transport of charged atoms (ions) across cell membranes. This transport chain is responsible for the proper signaling between brain cells.
PRRT2: The exact function of this gene is unknown. However, it is generally believed that it helps control signaling between neurons.
Overall, gene mutations in these genes create abnormal signaling between neurons in the brain, which leads patients with the condition to develop severe headaches. There is little evidence to suggest that any of these genes are responsible for the other headaches common in the general population.
A paper published in Nat Genet in 2016 identified 38 areas in the genome that may be linked to the condition.
Current Research on Migraines
Migraines often have a genetic component. Research has shown that one affected parent has a 50% chance of passing it on to a child. The probability increases to 75% if both parents suffer from it. Over 50% of people suffering from migraine have a family history.
A study in 2018 has led to the discovery of almost 50 locations in the genes where variations can cause this condition. It is believed that not one, but the interaction of many gene variations is the root cause.
Genome wide association studies (GWAS) have, however, made it easier to pinpoint those genes. Gene sequencing has been used to compare the genes of thousands of people who have migraines and those who don’t. This research led to the discovery of a dozen parts of the DNA sequence that are likely involved in causing the condition. Research using this method has led to a belief that migraines with auras are more commonly genetic than those without auras.
Familial hemiplegic migraine (FHM), for example, can be transmitted directly to offspring if they receive a copy of the mutated gene. FHM is an aura-type migraine. It leads to severe headaches and can even induce paralysis on one side of the body. Certain genes have been discovered to be linked with FHM. The genes causing FHM in individuals led to the creation of a classification system based on causal genes.
As noted in this review from 2019 by Griffiths, LR and colleagues, different classes of familial hemiplegic migraine are classified based on the genes that cause them.
Type 1: This is the most prevalent class of FHM. It is induced by variations in the CACNA1A gene.
Type 2: This type of migraine often causes seizures. It is induced by variations in the ATP1A2 gene.
Type 3: This type of migraine arises as a result of variations in the SCN1A gene.
Type 4: A person is said to have type 4 FHM if no gene is linked to the person’s migraine.
These episodes are a genetically complex disease that are influenced by environmental triggers. Further research into their genetic foundations may help future diagnosis and treatment.
Epidemiology (Part 3 of Are migraines genetic?)
Migraines are a very common and often debilitating condition. In 2018, the Centers for Disease Control and Prevention (CDC) reported that migraines affect 15.3% of American adults when they were asked about occurrences in the previous 3 months. It is a major cause of disability and accounts for things like physical impairment and reduced productivity at work or school.
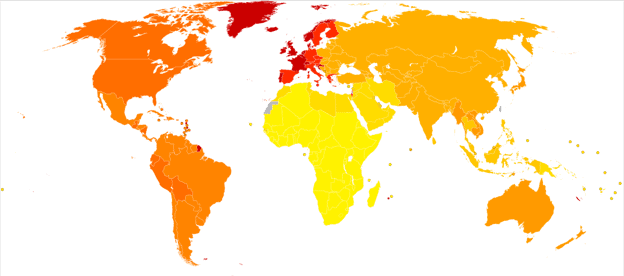
In 2019, researchers at Albert Einstein College of Medicine estimated that 12% of the US population gets episodic migraines while 1-2% of the global population suffers from chronic migraines. These are headaches that occur for at least two weeks out of the month, with the majority being migraines. The condition is associated with heart disease, psychiatric disease, and sleep disorders.
Although the occurrence is similar in boys and girls before puberty, it occurs about three times more frequently in adult and adolescent women than men. It is thought that fluctuating hormones play a role in this difference. This may also be why certain types of birth control have a side effect of severe headaches.
Symptoms (Part 4 of Are migraines genetic?)
The primary symptom of a migraine is a pounding or throbbing headache. The pain can start out as mild as progress to moderate and severe if left untreated. Pain may be on one side of the head or the entire head and can also encompass the eyes, temples, and other areas of the face.
Other symptoms described by the Cleveland Clinic include:
- Being sensitive to light and sound, and sometimes odor
- Nausea and vomiting, upset stomach, and abdominal pain
- Loss of appetite
- Feeling very warm (sweating) or cold (chills)
- Pale skin color (pallor)
- Feeling tired
- Dizziness and blurred vision
- Tender scalp
Most forms of the condition last about four hours (although they can last longer). The frequency of the condition can be as high as once a week or as low as once a year. The most common occurrence is 2-4 times per month.
A common characteristic that often occurs before a migraine is an aura, an event that normally involves sensory symptoms like
- Seeing bright flashing dots, sparkles, or lights
- Blind spots in your vision
- Numb or tingling skin
- Speech changes
- Ringing in your ears (tinnitus)
- Temporary vision loss
- Seeing wavy or jagged lines
- Changes in smell or taste
Auras normally last less than an hour and act as a warning sign that an episode is about to begin.
Causes (Part 5 of Are migraines genetic?)
Headaches are generally caused when nerves in blood vessels send pain signals to the brain. The signals then lead to an inflammation response. The mechanism of this process is largely unknown.
There is a strong association between genetics and migraines. At least 80% of patients who experience migraines will have a first-degree relative with the condition. Other causes include gender (with women being more at risk than men), increased stress, and smoking.
There are also a number of triggers that can lead to an increased risk of migraines. Emotional stress is believed to be the most common migraine trigger. Upon strong emotional response, various hormones are released in the brain, which can trigger a migraine. Further emotion can lead to additional physical responses such as muscle tension and dilated blood vessels, which can make a migraine worse.
Missing meals, sensitivity to certain chemicals and foods, caffeine or alcohol overuse, and fluctuating hormones are also thought to play a role. These triggers can also cause stomach pain, cramping, and nausea that some people refer to as abdominal migraines.
Diagnosis (Part 6 of Are migraines genetic?)
A positive diagnosis can only be made based on family history and physical description of the symptoms. There is no blood test or other measure to diagnose migraines. A neurologist will normally ask about family members with the condition, your medical history, and any physical symptoms you are having.
Some questions you may be asked include:
- How long have you had headaches?
- How many times in a week/month do these occur?
- How severe are they (mild, moderate, severe)?
- How long do they last?
- Do they keep you from doing activities or keep you from being at your best when doing activities?
- Do you get any warning that a migraine attack is about to happen (such as zigzag lines or dark spots in your vision)?
- Do you throw up or feel nauseated?
- Do odors, noise, or light make them feel worse?
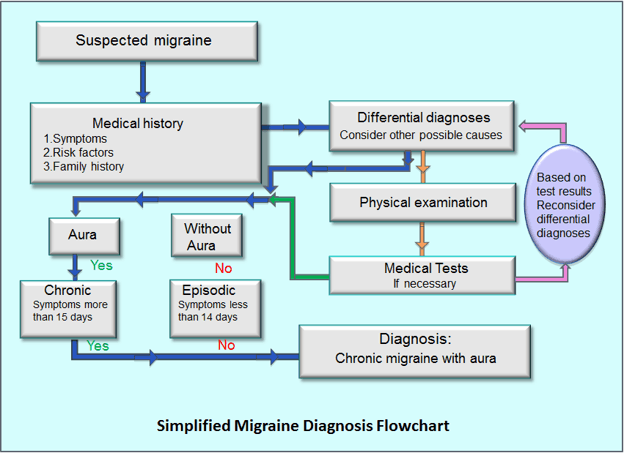
If the headaches become complex, unusual, or suddenly severe other diagnostic tests may be performed to rule out an underlying condition. Namely, an MRI or CT scan can check for tumors, strokes, infections, and other neurological conditions that may be causing the headaches.
Treatment (Part 7 of Are migraines genetic?)
Medications that either reduce pain or prevent occurrence are usually the first recommendations to treat migraines.
Medications for pain
These migraine medications are best taken when you first believe you are having an episode. In many cases, they include over-the-counter pain relievers such as aspirin or ibuprofen. Migraine-specific medications that combine additional ingredients like caffeine and acetaminophen are also available.
Some prescription medications are also available for those that need additional strength. These drugs, known collectively as triptans, block pain pathways in the brain. They may not be right for patients with heart problems.
According to Mayo Clinic, there are newer treatments, many just finishing clinical trials, available that work well for specific types of the condition.
Prevention medication
Some patients may experience frequent, recurrent headaches that respond poorly to acute treatment. In this case, your doctor may recommend medications designed to prevent migraines from occurring and reduce the length and intensity of the ones that do happen.
Most of these treatment options are medications used for other conditions. For example, blood pressure medication has been found to be especially useful for preventing the condition when it is accompanied by an aura. Various types of antidepressants are another option.
Anti-seizure medications have been recommended for some patients, but side effects such as dizziness, weight changes, and nausea mean that they are not prescribed as often. They can also be dangerous for pregnant women or women trying to become pregnant.
Some patients have found that botox injected about once every 12 weeks has a preventative effect in reducing migraine episodes.
You can visit the American Migraine Foundation for more resources and support.
If you liked this article, you should check out our other posts in the Nebula Research Library!
April 22, 2022
