Obstructive sleep apnea (OSA) occurs when breathing during sleep is interrupted for longer than 10 seconds at least five times per hour. In brief, it causes someone to start and stop breathing, often resulting in a restless night’s sleep. It is the most common sleeping-related breathing disorder, affecting around 1 billion adults.
OSA involves periods when throat muscles intermittently relax and block the airway, lowering oxygen levels in the blood. People with this condition often wake up suddenly but not long enough to remember it. The most common sign of OSA is snoring, although it can also cause daytime sleepiness, morning headaches, and difficulty concentrating. It is also associated with the risk of hypertension, cardiovascular disease, and depression.
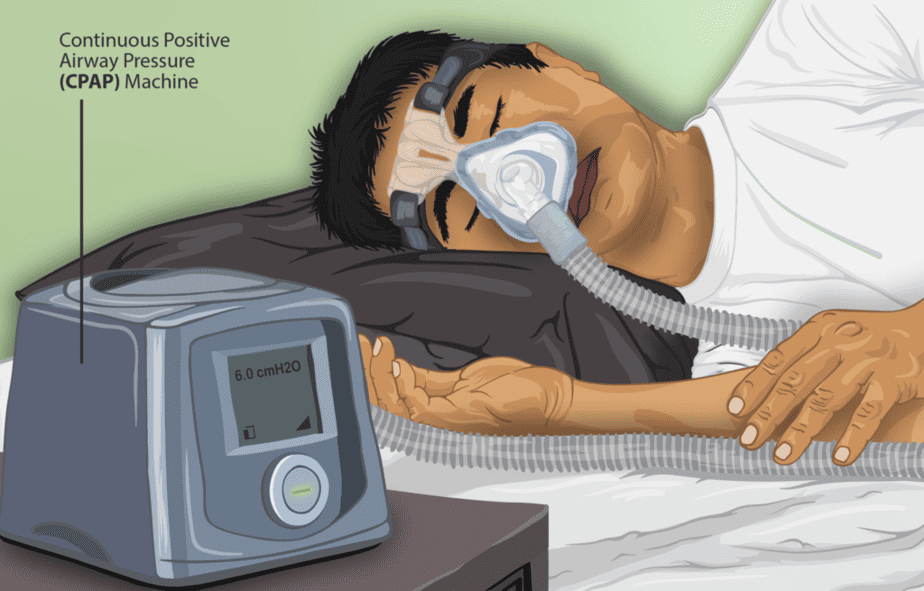
Doctors may recommend a combination of therapies to treat OSA, including lifestyle changes, positive airway pressure assistance, or surgery if the OSA is severe enough. The most common approach is using a Continuous positive airway pressure (CPAP) machine. This machine has a hose connected to a mask or nosepiece and delivers constant, steady air pressure while you sleep.
Sleep apnea variability
A relatively new observation regarding OSA is how severity can fluctuate from night to night. Researchers believe this variability may contribute to higher risks of heart problems.
A new study published in npj Digital Medicine seeks to understand the potential association between night-to-night variability in OSA severity and blood pressure. The authors found that those with the highest variability also had a 50-70% increased likelihood of uncontrolled hypertension compared to those with the lowest variability. This result could help doctors personalize treatments for sleep apnea patients, especially for patients with other cardiovascular risk factors.
| This post may interest those of you with a higher polygenic risk score for snoring or daytime sleepiness, both common symptoms of sleep apnea. |
The Study
The authors analyzed sleep and blood pressure data from over 12,000 adults. Participants had a mean age of 50 and were 88% male. Most lived in Europe or North America.
The study monitored the participants for about 180 nights using an under-mattress sleep sensor and combined that data with about 30 blood pressure measurements over that 6-month period.
Participants took their blood pressure measurements with an at-home device. The authors defined uncontrolled hypertension as having a mean systolic blood pressure ≥140 mmHg or mean diastolic blood pressure ≥90 mmHg.
Results
Both OSA severity and variability were associated with increased uncontrolled hypertension after controlling for age, sex, and BMI. Notably, uncontrolled hypertension was more common for participants with any OSA level (mild, moderate, or severe) than those without OSA. The greater the OSA level, the higher the risk of hypertension.

After accounting for OSA severity, the authors found that OSA variability alone was an independent variable for uncontrolled blood pressure. In other words, whether participants had more severe or less severe OSA, those with higher variability had a 50-70% greater chance of having uncontrolled blood pressure.
This study, conducted over six months, provides greater insight than previous findings that only looked at single-night readings. It also uses a larger sample size and at-home, non-invasive data collection, which captures real-world events. The authors believe these results will be valuable in helping doctors identify OSA patients at major risk for cardiovascular problems.
Some limitations of the study include fewer physiological inputs from the under-the-bed sensors than traditional apnea measurements. Additionally, the study did not consider confounding variables that may affect blood pressure, such as diet, exercise, medication, or tobacco or alcohol use. Finally, the study notably recruited more males than females. The authors recommend a follow-up study that includes a larger cohort of females to confirm that the relationship between OSA variability and hypertension exists among both sexes.
Citation
Lechat B, Loffler KA, Reynolds AC, Naik G, Vakulin A, Jennings G, Escourrou P, McEvoy RD, Adams RJ, Catcheside PG, Eckert DJ. High night-to-night variability in sleep apnea severity is associated with uncontrolled hypertension. NPJ Digit Med. 2023 Mar 30;6(1):57. doi: 10.1038/s41746-023-00801-2. PMID: 36991115; PMCID: PMC10060245.
