Nebula Genomics DNA Report for Chronic Kidney Disease
Is chronic kidney disease genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
What is Chronic Kidney Disease?
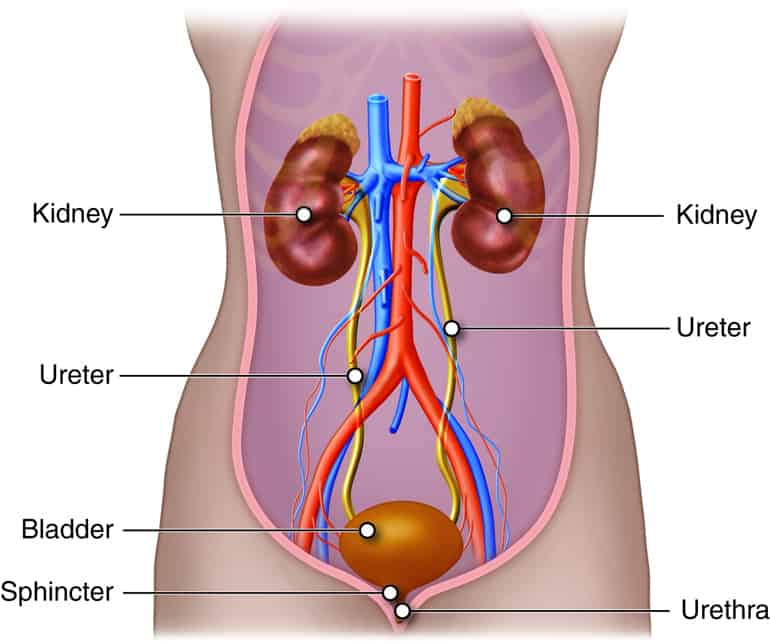
Kidneys filter blood and remove waste from the body. Chronic kidney disease (CKD) is a medical condition in which the kidneys are damaged and can’t perform these functions. When they stop working properly and no longer filter waste, toxins and extra fluid build up in the body and contribute to high blood pressure, heart disease, stroke, and early death.
The condition develops gradually, leading to permanent kidney damage if left untreated. Kidney disease worsens over time and can progress to kidney failure, requiring dialysis or kidney transplantation.
Is Chronic Kidney Disease Genetic?
The condition can have a genetic component, but it is not always inherited, or passed down from parent to child. Some types of kidney disease have a strong genetic link, but in most cases, lifestyle and medical conditions also play a role in its development.
In addition, having family members with kidney disease can increase a person’s risk of developing the disease. Several genes have been associated with kidney disease. Scientists have identified these variants through gene mapping, gene identification, and genome wide association studies.
PKD1 and PKD2: These gene variants can cause autosomal dominant polycystic kidney disease (ADPKD), a common inherited form of genetic kidney disease. On the other hand, autosomal recessive polycystic kidney disease (ARPKD) is much less common. Autosomal recessive inheritance affects 1 in 20,000 children. Genetic testing can be used in these cases to diagnose the condition.
COL4A3, COL4A4, and COL4A5: Variants can cause Alport syndrome, a rare inherited kidney disease.
NPHS1, NPHS2, and CD2AP: Variants can cause nephrotic syndrome, a condition that can lead to CKD.
MYH9: Mutations in this gene have been associated with several rare diseases, including the May-Hegglin anomaly and Fechtner syndrome.
HNF1B: Mutations in this gene have been associated with a rare form of CKD known as renal cysts and diabetes syndrome. It’s important to note that genetic variants can increase the risk of developing CKD, but they are not the primary cause. In most cases, lifestyle and medical conditions such as type 1 and type 2 diabetes and high blood pressure influence the condition’s development. Clinical trials are ongoing to help get a better sense of kidney disease genetics.
Epidemiology
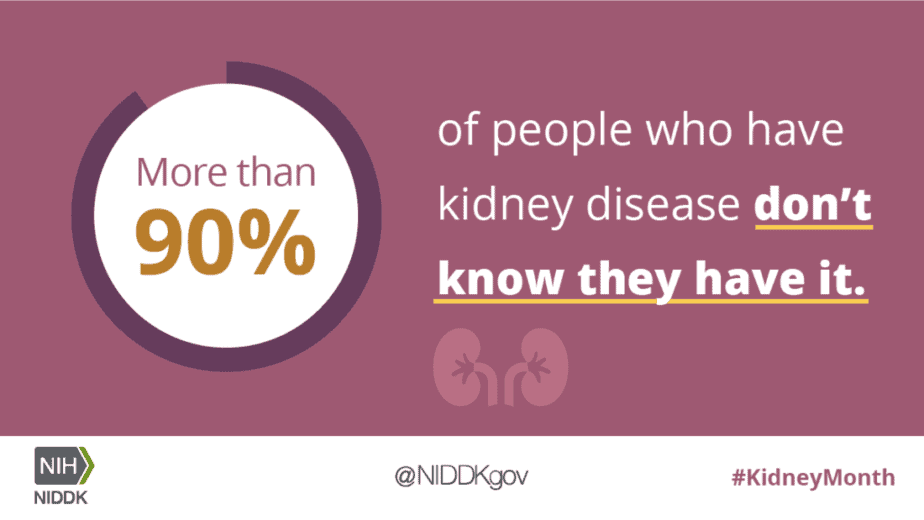
Unfortunately, many people, potentially as high as 9 in 10 adults, with chronic kidney disease are not aware that they have the condition. In its early stages, it can be asymptomatic. As a result, many cases go undiagnosed.
Chronic kidney disease is a significant public health problem that affects around 10% of the global population. In the United States, experts believe 15% of US adults or 37 million people have the condition. With an aging population and an increasing incidence of risk factors such as diabetes and hypertension, kidney disease prevalence is rising worldwide.
A critical kidney disease risk factor is age as it is more common in people over 65. Inherited genetic kidney disease is the most common cause for those diagnosed before the age of 30. Additionally, specific populations, such as African, Hispanic, and Native Americans, are at higher risk of developing kidney disease.
Symptoms
Chronic kidney disease (CKD) can progress slowly. Therefore, many people with early-stage CKD may not experience any symptoms. However, as the disease progresses, the following symptoms may develop:
- Fatigue and weakness: As the kidneys can produce less erythropoietin (a hormone that stimulates red blood cell production), people with kidney disease may experience fatigue and weakness.
- Swelling: Fluid retention is a common symptom of kidney disease, and it can lead to swelling in the legs, ankles, feet, face, and hands.
- Shortness of breath: Fluid buildup in the lungs can cause shortness of breath.
- Urinary changes: This includes things such as increased or decreased urine output or changes in the appearance of urine (such as foamy or dark urine).
- Nausea and vomiting: The condition can cause a buildup of toxins in the body, leading to nausea and vomiting.
- Itching: A buildup of waste products in the body can also cause dry, itching skin.
- Muscle cramps: Imbalances in electrolytes, such as potassium and calcium, can cause muscle cramps.
- Sleep problems: People with CKD may experience sleep problems, such as insomnia or restless legs syndrome.
Many other conditions can cause these symptoms. Because of how gradual the disease is, signs and systems may only be truly noticeable after irreversible damage.
Causes
Several conditions and diseases can lead to issues with kidney function that ultimately bring on chronic kidney disease.
- Diabetes: Diabetic kidney disease is the leading cause of chronic damage. High blood sugar levels can damage the small blood vessels in the kidneys, leading to the condition.
- High blood pressure: High blood pressure can damage the blood vessels in the kidneys, leading to CKD.
- Glomerulonephritis: This condition is a type of kidney inflammation.
- Polycystic kidney disease: Polycystic kidney disease is an inherited condition that can develop kidney cysts.
- Infections: Severe or recurrent kidney infections can cause scarring and kidney damage.
- Urinary tract obstructions: Blockages in the urinary tract, such as kidney stones or tumors, can cause urine to back up into the kidneys.
- Prolonged use of certain medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can cause kidney damage.
- Genetic conditions: Some genetic diseases, such as Alport syndrome, can cause CKD.
- Medical conditions: Other conditions, such as lupus, HIV, and hepatitis B and C, can also impact development.
It is essential to identify and manage the underlying cause to slow the progression of the disease and prevent complications.
You may also be at higher risk if you smoke or are overweight. Furthermore, recent research has shown that conditions associated with an enlarged prostate may contribute to kidney damage.
Diagnosis
Doctors typically diagnose kidney disease using a combination of medical and family history, a physical examination, and laboratory tests. Doctors commonly use the following tests to diagnose kidney disease:
Blood tests: Blood tests measure the creatinine level, a waste product of muscles, in the blood. The creatinine level is used to estimate the glomerular filtration rate (GFR), which measures how well the kidneys function. A GFR of less than 60 mL/min/1.73m² for three months or more indicates chronic kidney disease.
Urine tests: Urine tests check for protein or blood in the urine, which can indicate kidney damage.

Imaging tests: Doctors may use imaging tests, such as ultrasound, CT scan, or MRI, to visualize the kidneys and check for abnormalities.
Biopsy: Doctors may perform a kidney biopsy in some instances to help determine the cause of CKD.
Once diagnosed, your doctor will determine the stage of chronic kidney disease based on the GFR level and the presence of any complications. The five stages are:
- Stage 1: GFR greater than or equal to 90 mL/min/1.73m² with evidence of kidney damage.
- Stage 2: GFR between 60-89 mL/min/1.73m² with evidence of kidney damage.
- Stage 3: GFR between 30-59 mL/min/1.73m².
- Stage 4: GFR between 15-29 mL/min/1.73m².
- Stage 5: GFR less than 15 mL/min/1.73m², also known as kidney failure.
Early detection can help prevent disease progression and limit complications.
Treatment
Treatment depends on the disease’s stage, the underlying cause, and complications. The main treatment goals are to slow the progression of the disease, manage symptoms, and prevent complications.
Lifestyle changes: Lifestyle changes, such as following a healthy diet, staying physically active, maintaining a healthy weight, quitting smoking, and limiting alcohol consumption, can help slow the condition’s progression.
Medications: Medications may be prescribed to control complications such as high blood pressure, high cholesterol, and diabetes. Certain medications may also be prescribed to manage symptoms, including swelling, anemia, and bone disease.
If you liked this article, you should check out our other posts in the Nebula Research Library!
May 12, 2023
