Table of contents
Nebula Genomics DNA Report for Mental Illness
Is mental illness genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Mental Illness?
A mental illness or mental disorder involves a condition that affects the brain and outward behavior. Experts all refer to them as mood disorders and can be accompanied by deviations in perception, thinking, feeling, or even self-perception. Mental illnesses often lead to significant personal suffering and stress, and problems functioning in several areas of daily life.
An essential component of these disorders is also often a reduced ability to regulate oneself. In this case, the affected person can hardly (or not at all) influence their disease. This is despite increased efforts, self-discipline, or willpower. Consequences include problems in coping with everyday life and impaired social relationships.
The World Health Organization estimates that around 300 million people worldwide are affected by depression, 47.5 million by dementia, and 21 million by the disorder of schizophrenia. Other mental health disorders include:
- Dissociative disorders
- Substance use disorders, eating disorders
- Post traumatic stress disorder (PTSD)
- Adjustment disorders
- Personality disorders.
Certain symptoms of those with an autism spectrum disorder may appear similar to those of a mental illness (e.g., anxiety and depression).
There are many resources available. For example. the National Survey on Drug Use and Health measures national mental illness prevalence and health care.
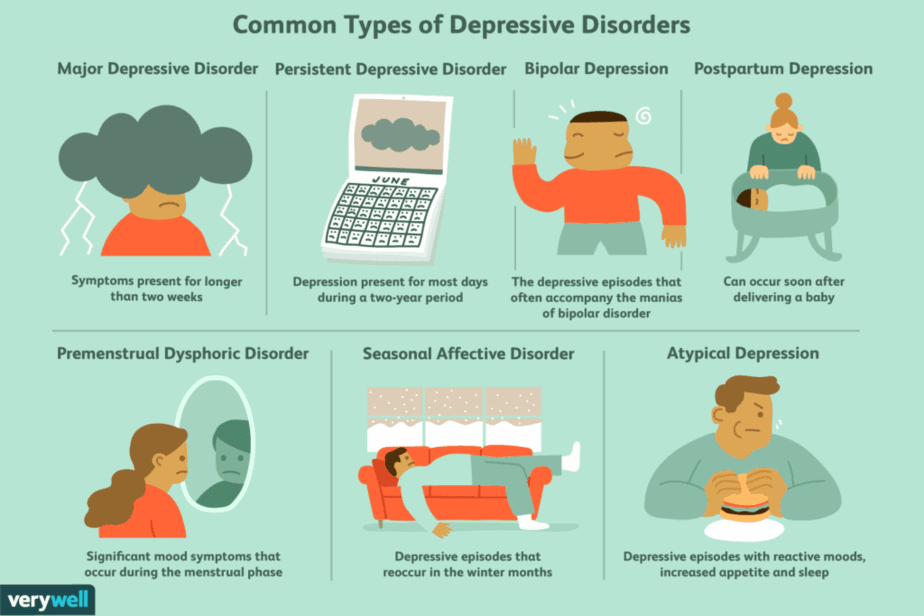
Depression
Depression is one of the most common mental illnesses in the world.
According to the American Psychiatric Association, people who experience typical symptoms of depression will feel a depressed mood, brooding, a feeling of hopelessness, and a diminished drive. Frequently, they lose joy and feelings of pleasure, self-esteem, performance, empathy, and interest in life. Quality of life is often impaired as a result.
These complaints occur in healthy people in the context of grief after a loss experience and appear as depression. However, they usually pass by on their own. Illness is present when the symptoms persist for a disproportionate length of time or when their severity and duration are out of proportion.
In psychiatry, experts assign depression to affective disorders. Doctors make the diagnosis according to symptoms and course (e.g., single or repeated depressive episodes). The standard treatment of depression includes psychotherapy and antidepressants, depending on the individual’s unique needs.
Medically, depression is a serious mental illness and medical condition. It requires treatment and often has many consequences not influenced by the willpower or self-discipline of the person affected. Depression is a major mental health crisis and is a significant cause of incapacity to work or early retirement and is a leading cause of suicide.
Is Mental Illness a Genetic Disorder?
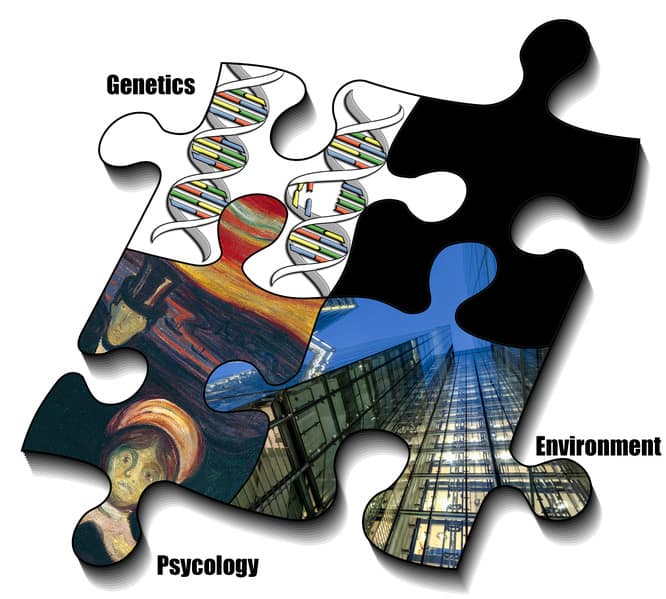
Depression can run in families, but can it be passed on in families through genes? Twin test results show that there is no single gene that determines the disease and that the genetic component is only one factor contributing to the disorder. Even with identical genetic make-up (identical twins), those with a sibling with depression tend to develop mental illness in less than half of the cases.
Scientists have also found differences between affected and non-affected twin partners in the subsequent (epigenetic) alteration of the genetic information. That is, influences of life history on the control of the genetic information. This is also impacting parents or siblings with an increased risk of developing depression.
This still begs the question, “is mental illness genetically inherited?” and “Is it passed on in family?” In any case, doctors use a full family history to help to address the genetic basis of each patient’s case in order to find family members with depression. However, the affected relative may never develop depression or other mental illness symptoms.
Furthermore, there is a gene-environment interaction between genetic and environmental factors that impact people who develop depression. For example, genetic factors can cause a certain person to often maneuver himself or herself into difficult life situations through a great willingness to take risks. Conversely, whether a person copes with a psychosocial burden or becomes depressed can depend on genetic factors.
Depression genes
After genetic testing in psychiatry, researchers suspect a significant genetic vulnerability factor for the occurrence of depression to be a variation in the promoter region of the serotonin transporter gene 5-HTTLPR. 5-HTTLPR stands for Serotonin (5-HT) Transporter (T) Length (L) Polymorphic (P) Region (R). This “depression gene” is located on chromosome 17q11.1-q12 and occurs in different forms in the population (so-called “different length polymorphism” with a “short” and a “long allele”).
Carriers of the short allele react more sensitively to psychosocial stress. As a result, they have up to twice the risk (disposition) of developing depression than carriers of the long allele.
Is there genetic testing for mental illness? Two meta-analyses in 2011 from genetic research and clinical trials identify the genetic association between the short allele and the development of depression after stress. In a meta-analysis in 2014, scientists found significant data in connection with depression for a total of seven candidate genes tested: 5HTTP/SLC6A4, APOE, DRD4, GNB3, HTR1A, MTHFR, and SLC6A3.
Some direct-to-consumer genetic testing companies include Genesight and Genomind.
However, certain abnormalities that are decisive for the development of depression have not yet been found despite an extremely extensive search on several genetic variants. The discovery of these will help better understand the genetic role in the development of mental conditions and the likelihood of developing something like depression.
Risk factors for developing depression include experiencing a traumatic event, having a history of other mental illnesses, taking certain medications, and experiencing severe or chronic disease. These contributions to mental conditions have long been documented.
Current Research on Genetic Mental Illness
There is no doubt that the COVID-19 pandemic has triggered cases of people with mental illness in the public. In April and May 2020, the Centers for Disease Control and Prevention conducted a study on the prevalence and increase of cases. But this is not the only study taking place on the effect the pandemic has had on all demographics. This very interesting study on The Impact of COVID-19 on individuals living with serious mental illness discusses how the pandemic exacerbated symptoms in patients with SMI.
Experts have found that a common highly heritable factor, called the p factor, is related to psychopathology in childhood and adolescence. The study, among other actions, assessed the stability of environmental and genetic influences on the p factor across time.
A more recent study: Identifying drug targets for neurological and psychiatric disease via genetics and the brain transcriptome find the relationship between the efficacy of certain drugs and genetic variants to help better target mental diseases towards good mental health.
There is strong evidence today for genetic markers responsible for mental illness, but there is still not much information on how gene expression differs from one psychiatric disorder to another. This article Deep transcriptome sequencing of subgenual anterior cingulate cortex reveals cross-diagnostic and diagnosis-specific RNA expression changes in major psychiatric disorders investigates a postmortem cortex to understand the link between the limbic system and mental illness.
Epidemiology
In an international comparative study updated in 2018, researchers compared the frequency in high-income countries with that in middle and low-income countries. The average lifetime and 12-month prevalence of depression was 14.6 % and 5.5 % in high-income countries. The ratio of women to men was approximately 2:1. According to the National Institute of Health’s National Institute of Mental Health, an estimated 51.5 million adults aged 18 or older in the United States (20.6% of all U.S. adults) had Any Mental Illness (AMI) in 2019.
In the United States, nearly 7% of adults experience depression. With the age of onset being an average of 31 years old. The range at which people experience mental conditions varies among populations and genders.
The burden of illness due to depression, for example, in older adults that presents itself in the incapacity to work, inpatient treatment, and early retirement, has risen sharply in recent years. Experts assume that the actual incidence of illness has changed much less severely and that the increased incidence is due to better recognition and less stigmatization of people with mental disorders. On the other hand, long-term studies tend to indicate a real increase, which is associated with various societal influencing factors.
Symptoms
Main symptoms
The main symptoms of depression, a mental illness, include:
- Depressed, depressed mood: Experts characterize depression by a narrowing of the spirit or, in the case of severe depression, the “feeling of numbness” or the feeling of persistent inner emptiness.
- Loss of interest and joylessness: Loss of the ability to feel joy or sadness; loss of affective resonance, i.e., the patient’s mood cannot be brightened up by encouragement
- Lack of drive and increased fatigue: Another typical symptom is drive inhibition. In a severe depressive episode, people affected can be so severely inhibited in their drive that they are no longer able to perform even the simplest activities such as personal hygiene, shopping, or washing up.
Additional symptoms
- Reduced concentration and attention
- Decreased self-esteem and self-confidence (feeling of insufficiency)
- Feelings of guilt and inferiority
- Negative and pessimistic prospects (hopeless): Characteristics are exaggerated concern about the future, possibly exaggerated anxiety due to minor disturbances in the area of one’s own body (see hypochondria), the feeling of hopelessness, helplessness, or actual helplessness.
- Suicidal thoughts or actions: Severely affected persons often feel that their life is entirely meaningless. Often this agonizing state leads to latent or acute suicidal tendencies.
- Insomnia
- Reduced appetite
People with depression often experience physical symptoms, such as pain in very different parts of the body, most typically with an agonizing feeling of pressure on the chest. During a depressive episode, patients have an increase in the susceptibility to infection.
People also observe social withdrawal, slowed thinking (inhibition of thinking), senseless circling of thoughts (compulsion to brood), and disturbances of the sense of time. Irritability and anxiety often exist. In addition, hypersensitivity to noise can be a problem.
Anxiety and bipolar disorder is also a subgroup of depression and occurs when patients experience severe bouts of mania, followed by prolonged depressive and anxiety spells. Depression can also occur with anxiety disorders.
Severity
Severity is classified according to the number of symptoms:
- Mild depression: two main symptoms and two additional symptoms
- Moderate depression: two main symptoms and three to four additional symptoms
- Severe depression: three main symptoms and five or more additional symptoms
The symptoms of depression can manifest themselves in different ways depending on gender. However, the differences in the core symptoms are minor. In women, phenomena such as despondency and brooding are more common. However, depression in mend can be reflected in a tendency to behave aggressively.
In a 2014 study, scientists associated the different manifestations in women and men with differences in the biological systems of the stress response.
Causes
The causes of mental illnesses and depressive disorders are complex and only partially understood. There are both predispositions and acquired susceptibilities to the development of mental illness. Biological factors and by life-historical social or psychological stress can trigger acquired susceptibilities. Season Affective Disorder is also a specific type of depression that correlates with seasonal changes.
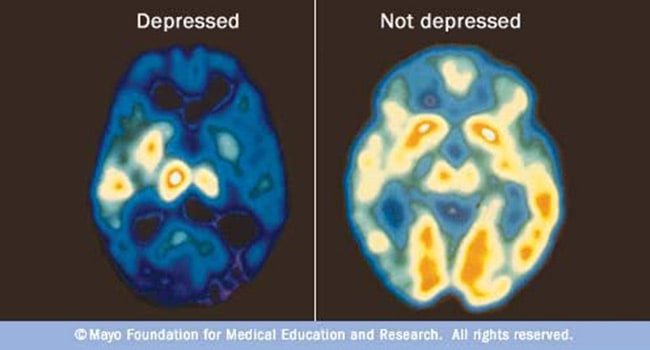
After the introduction of reserpine as a drug in the 1950s, patients treated with it observed symptoms of mental illness. Experts attributed this to the lowering of neurotransmitters in the brain. They consider certain signal transmission particularly involved in the monoaminergic neurotransmitters serotonin, dopamine, and noradrenaline.
Other signaling systems are also involved, and their mutual influence is highly complex. Although monoaminergic influencing drugs (antidepressants) can change depressive symptoms, it remains unclear to what extent these transmitter systems are causally involved in the development of depression. Thus, about one-third of patients respond only insufficiently to drugs that influence monoaminergic systems or do not respond at all.
Treatment
Doctors can successfully treat depression in the majority of patients. The Diagnostic and Statistical Manual of Mental Disorders proposes several alternatives based on recent research.
Possible options for treating depression include drug treatment with antidepressants, psychotherapy, or a combination of drug and psychotherapeutic treatment. Doctors are increasingly supplementing and supporting these efforts with online therapy programs. Other therapy methods for persistent depressive disorder, such as light therapy or sleep therapy, sports, and exercise therapy, complement the treatment options.
The current national treatment guidelines consider antidepressants to be equivalent to psychotherapy for moderate to severe depressive periods. For severe depression, doctors often recommend a combination of psychotherapy and antidepressant medication. Ultimately, health care professionals handle their approach to treat mental illness on a case-by-case basis.
Physicians or mental health professionals with psychotherapeutic training can carry out a combination of psychotherapy and drug treatment. Alternatively, a cooperation of physicians and psychotherapists can approach treatment on an outpatient basis or in psychiatric clinics or specialized hospitals.
Severe cases
In cases of high suffering and an unsatisfactory response to outpatient therapy and drugs for psychotic disorders, especially in cases of imminent suicide, experts consider treatment in a psychiatric clinic.
People with major depression and other mental health problems can also see their physical health affected. They are usually also at a higher risk for chronic problems such as heart disease.
Multiple hotlines exist, free for the public, for persons who have a mental illness. For example, the Substance Abuse and Mental Health Services Administration offers a National Helpline, a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
If you feel suicidal, you should call 911 or your local emergency number immediately. You can reach The National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Medications
Antidepressant
In depression, the signal transmission from the axon of one neuron (top) to the dendrite of another neuron (bottom) is increased, e.g., by blocking transporters that return released neurotransmitters to the axon. This increases the number of transmitters in the synaptic cleft between the cells and signal transmission from cell to cell. Drugs that block such transporters are typical for antidepressants.
The effectiveness of psychiatric medications to treat mental illness is strongly dependent on the severity of the mental illness. While the efficacy is absent or low in mild and moderate severity, it is higher in severe depression.
In the most severe forms, up to 30% of the treated patients benefit from antidepressants. Meta studies indicate that antidepressant drugs show great differences in their effectiveness from patient to patient. In some cases, a combination of different medications can have advantages.
Selective reuptake inhibitors
These active ingredients inhibit the reuptake of the neurotransmitters serotonin, norepinephrine, or dopamine, into the presynapses. Direct effects on other neurotransmitters are significantly weaker with these selective agents than with tricyclic antidepressants.
The most commonly used drugs for depression today are selective serotonin reuptake inhibitors (SSRIs). They are effective for a duration of two to three weeks. They (largely) selectively inhibit the reuptake of serotonin at the presynaptic membrane. This results in a “relative” increase in the messenger substance serotonin during signal transmission.
Monoaminooxidase (MAO) inhibitors
MAO inhibitors work by blocking the monoamine oxidase enzymes. These enzymes cleave monoamines such as serotonin, norepinephrine, and dopamine, reducing their availability for signal transmission in the brain. The MAO inhibitors inhibit these enzymes, which increases the concentration of monoamines and, thus, of neurotransmitters. This enhances signal transmission between the nerve cells.
MAO inhibitors are divided into selective or non-selective and reversible or irreversible. Selective inhibitors of MAO-A (e.g., moclobemide, reversible) only inhibit type-A monoamine oxidase and show an antidepressant effect. They are generally well tolerated, including with significantly less disturbance of digestive and sexual functions than SSRI’s.
Ketamine
In depressive emergencies (suicide risk), several studies confirmed a rapid antidepressant effect of ketamine. This is an antagonist at the glutamate NMDA receptor complex. Study results showed a significant improvement for up to seven days when administered once. There are recommendations for low-dose prescription, which, in contrast to using as an anesthetic or dissociative, shows hardly any side effects.
Alternative Approaches for those with mental health conditions
- Light therapy
- Exercise
- Nutrition
- Sleep Monitoring
- Sleep Deprivation
- Meditation
- Support groups
Did you enjoy this article? Read more articles like this in our Nebula Research Library! Here, you can find more articles on health topics such as depression, mental health disorders such as Alzheimer’s disease, and other disorders related to Alzheimer’s like dementia.
You may also be interested in medication reviews, like the antidepressants Lexapro and Zoloft.
June 10, 2022
