Table of contents
Nebula Genomics DNA Report for Inflammatory Markers
Are inflammatory markers genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What are Inflammatory Markers?
What is inflammation?
It is the body’s natural defense mechanism to protect against harmful infections and normally appears as redness, swelling, hyperthermia, pain and functional impairment at the sight of infection. The inflammatory process occurs as the result of a cascade of messenger signals in the immune system that ultimately results in anti-inflammatory chemicals. The function of inflammation is to eliminate the initial cause of cell injury, remove dead or damaged cells and tissues, and initiate tissue repair.
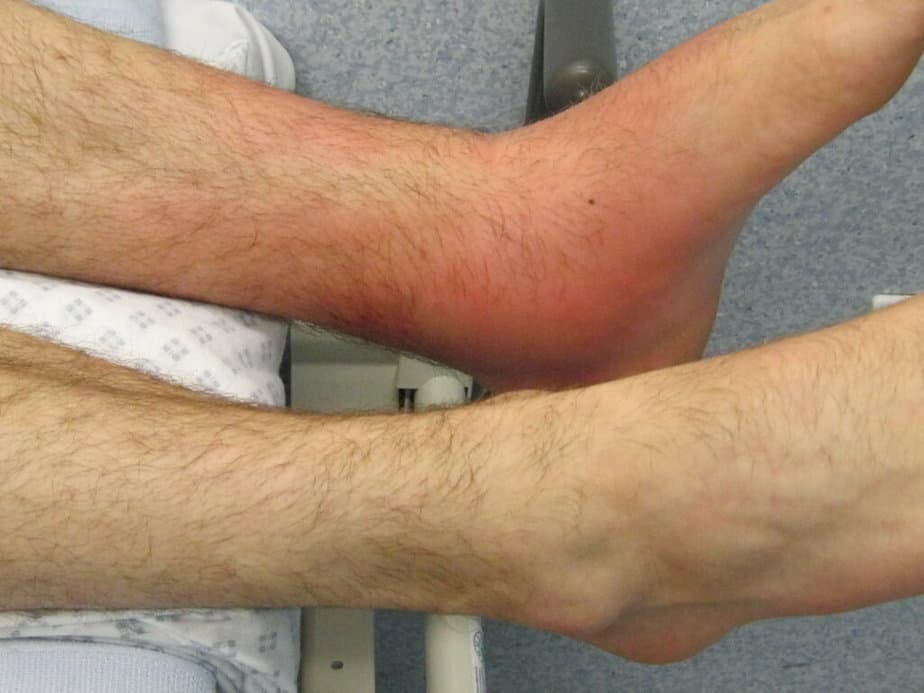
Inflammation can be either acute or chronic. Acute inflammation occurs as a response to harmful stimuli by driving white blood cells to the area of injury. On the other hand, chronic inflammation is a prolonged episode of the condition that involves an overall change in the types of cells present.
In most cases, inflammation is a necessary process to protect a person from foreign substances. It also plays a role in hemostasis and coagulation, which is an important component of wound healing. However, sometimes unregulated inflammation can cause more harm than good—autoimmune disorders like Addison’s disease, lupus, vitiligo, and rheumatoid arthritis. Other conditions that are not considered to be autoimmune disorders may be implicated by uncontrolled inflammation, such as inflammatory bowel disease and giant cell arteritis.
What are inflammation markers?
These refer to dissimilar biological markers that indicate the presence (or absence) of inflammatory disease activity.
Experts have associated chronic presentations of the condition with many diseases, including type 2 diabetes and cardiovascular disease. Doctors most often assess inflammation by measuring the C-reactive protein level (CRP) in the blood, which typically increases if there is an inflammation.
Did you know you can test inflammation markers at home? Learn more in our article about at home inflammation tests.
Are Inflammatory Markers Genetic?
Many of the disorders linked to chronic inflammation have both genetic and environmental components. You can read more about these disorders and other genetically influenced conditions on our blog.
Traditionally, the genes directly related to inflammation through genome wide association studies regulate immune responses such as IL-6, IL-1 cluster, and IL-10.
IL-6: This gene codes a cytokine that functions in inflammation and the maturation of B cells. It may also induce fever in people with autoimmune diseases or infections. The protein is primarily produced at acute and chronic inflammation sites, where it is secreted into the serum and creates an inflammatory response through binding to a receptor.
Certain phenotypes may increase susceptibility to diabetes and systemic juvenile rheumatoid arthritis. Experts have also found elevated levels of the encoded protein in virus infections, including COVID-19 (SARS-CoV-2).
IK-1 cluster: This group of genes encodes 11 cytokines that produce a pro-inflammatory cytokine network and regulate immune and other inflammatory responses.
IL-10: This gene codes an anti-inflammatory cytokine. It downregulates the expression of MHC class II antigens, Th1 cytokines, and co-stimulatory molecules on macrophages. It also enhances B cell survival, proliferation, and antibody production. IL-10 can block NF-κB activity and is involved in the regulation of the JAK-STAT signaling pathway.
Other genes involved in the insulin/IGF-I signaling pathway and genes that counteract oxidative stress (PON1) also play a role in chronic inflammation.
Current Research on Inflammatory Markers
One of the most well-known of the elevated inflammatory markers is undoubtedly the C-reactive protein (CRP). As we have seen, raised inflammatory marker levels like this one indicate an infection or inflammation. The World Health Organization (WHO) confirmed this observation in a previously reported 2017 revised paper.
Many of the markers known to diagnose inflammation may vary in their accuracy to reveal a potential inflammation. This study puts the most well-known inflammatory markers (CRP, ESR, and PV) to the test of accuracy.
An interesting study from 2018 evaluated the effects of vitamin D’s anti-inflammatory properties in patients with heart failure. Up to this time, there had not been studies regarding this relationship. Still, this particular research found some evidence (although not significant enough) for a difference in the effects of inflammation on patients with HF and those who do not have heart failure.
This paper, also from 2018, provides a more in-depth study of the clinical significance and potential role of C-reactive protein in chronic inflammation and neurodegenerative diseases.
Epidemiology
The prevalence of conditions that cause unbalanced levels of inflammatory markers in the blood has been rising in the United States. In 2005, 44% of Americans were living with chronic conditions, and 13% had three or more. In comparison, nearly 60% of Americans had at least one chronic illness, and 42% had more than one in 2014. Worldwide, 3 of 5 people die due to chronic inflammatory diseases like stroke, chronic respiratory diseases, heart disorders, cancer, obesity, and diabetes.
Symptoms
Inflammation has a number of hallmark symptoms usually noticeable by physical inspection. Experts often call these symptoms the five cardinal signs of inflammation:
- Heat
- Pain
- Redness
- Swelling
- Loss of function

Other systemic symptoms that can be diagnosed with special equipment include:
- Fever
- Fatigue
- Headaches
- Loss of appetite
- General feeling of illness
- Increase or decrease in leukocytes (white blood cells)
- CRP increase (immunologically active acute phase protein)
- Acute phase reactants (APR) increase or decrease
- Accelerated blood cell count (BKS or BSG for blood cell count)
- Procalcitonin increase (hormone precursor)
Signs and symptoms of acute inflammation may last from a few days to up to six weeks. The symptoms of the chronic form of the condition can continue for up to months or years.
Conditions linked to chronic inflammation include:
Causes
Sudden injuries, like broken bones or illnesses, including infections caused by bacteria or viruses can cause acute inflammation. The process occurs quickly and can be severe. Acute inflammation can last anywhere from a few days to a few months, depending on the injury or disease.
Injuries typically result in local inflammation, while illnesses result in systemic inflammation, in which the whole body generates an immune response.
The cause of chronic inflammation is largely unknown. Using diagnostic tools to measure inflammation markers in the blood is a common way to identify it.
Long-term forms of this condition can last for years or even an entire lifetime, and it can begin when there is no injury or illness present. While it is associated with many disease types, it does not appear to serve a protective purpose and even leads to tissue damage.
Doctors commonly associate heart disease and diabetes with chronic inflammation. Many of the same causes that contribute to these disorders are also linked to inflammation through the production of excess inflammatory chemicals or lowered production of anti-inflammatory molecules:
- Physical inactivity
- Obesity
- Diet
- Smoking
- Low sex hormones
- Stress
- Sleep disorders
- Advanced age
Diagnosis
There is no single test to identify inflammation in clinical practice. Doctors can diagnose most local cases through physical examination of the infected area and are correlated with injury. Since acute inflammation clears up relatively quickly, it is usually self-diagnosed and does not require treatment.
With chronic inflammation, which is not as easily recognizable, your doctor may recommend a blood test for inflammation to look for inflammatory markers in blood. Everyone has some amount of these biomarkers within a certain range. When lab test results indicate markers that drop below or exceed the acceptable extent, doctors consider them a hallmark of inflammation.
These markers of inflammation are not specific to a particular condition. Therefore, if abnormal levels are found, your doctor will often recommend follow-up tests to determine what is causing the chronic inflammation.
Blood tests
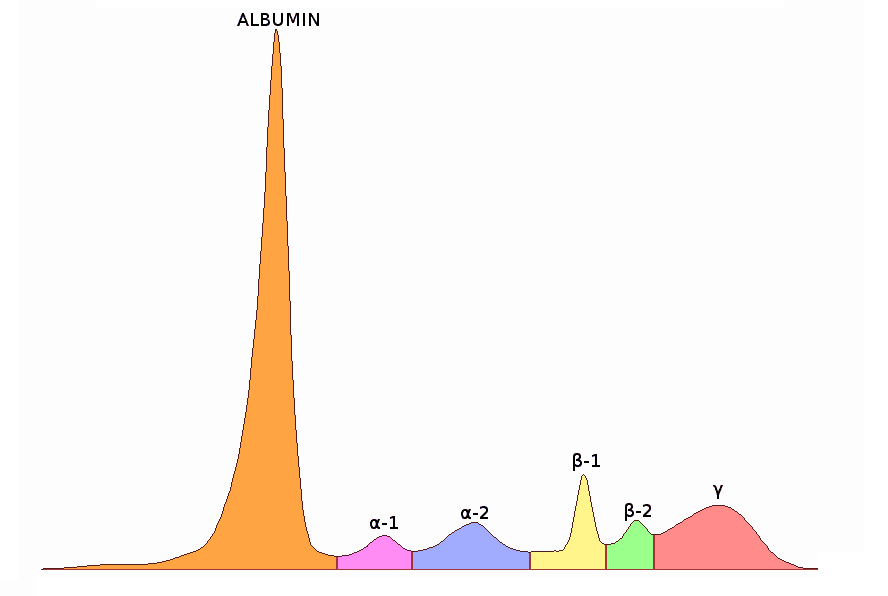
Serum protein electrophoresis (SPE): SPE is considered the best way to confirm chronic inflammation. It measures several different proteins in the blood’s plasma. Either too much or too little of these proteins can indicate inflammation and markers for other ailments.
C-reactive protein (CRP): The liver naturally produces the protein CRP protein in response to inflammation. If a severe form occurs, your liver will overproduce the protein, and tests can detect elevated CRP levels through an inflammatory markers test.
This inflammation test diagnoses have a high sensitivity. However, the level of CRP will be elevated in both acute and chronic inflammation. Identification of other symptoms is needed to determine if chronic inflammation is occurring or if it is only temporary.
Low levels of C-reactive protein are found with a high-sensitivity C-reactive protein (hs-CRP) test. Decreased levels of this marker can indicate a higher risk of heart disease for people without the condition.
Erythrocyte sedimentation rate (ESR or sed rate): The ESR test indirectly measures inflammation by quantifying the rate at which red blood cells sink in a tube of blood. The quicker they drop, the more likely you’re experiencing inflammation. Doctors rarely perform this test alone but it can be a quick way to monitor the inflammatory condition.
Erythrocyte sedimentation rate (ESR) and C reactive protein are some of the oldest laboratory tests still used in the clinic today. Both erythrocyte sedimentation rate and C reactive protein tests detect acute and chronic inflammation.
Plasma viscosity: This test measures the thickness of blood. Thicker than normal plasma can signal inflammation or infection.
If your doctor believes the inflammation is due to viruses or bacteria, they may perform more specific tests.
Treatment
Inflammation treatment relies largely on the underlying cause. It’s important to note that in most cases no treatment is necessary and it clears up on its own.
However, some forms require immediate medical attention, usually from a primary care professional. For example, inflammation may be caused by an infection. Left untreated, infections can become serious and lead to sepsis, a life-threatening condition.
Medications
Nonsteroidal anti-inflammatory drugs: Also called NSAIDs, these medications help relieve pain, swelling, fever, and other symptoms by affecting a protein involved in the inflammatory response. Although the treatment is working if it reduces the symptoms, they do not remove the cause of inflammation.
Examples of over-the-counter NSAIDs include naproxen, ibuprofen, and aspirin.
Acetaminophen: Sold as paracetamol or Tylenol, acetaminophen is used to relieve pain. It does not affect the underlying inflammation.
Corticosteroids: Corticosteroids, such as cortisol, are a type of steroid hormone. They can affect many of the processes involved in inflammation and are often prescribed for specific conditions. They are available as pills, injections, in an inhaler, or as creams or ointments.
It’s important to remember that long-term use of corticosteroids can be harmful.
Some of these drugs work by repressing the body’s immune system. They can help relieve symptoms of rheumatoid arthritis, psoriasis, and other similar autoimmune reactions. However, they can also leave a person’s body less able to fight an infection if it occurs.
People who have undergone transplant surgery also use immunosuppressant drugs to prevent their bodies from rejecting the new organ.
Besides traditional medications, some patients also include other types of treatments. These may consist of special herbs (ginger, turmeric, and cannabis are examples) or by eating an anti-inflammatory diet.
Diet
An anti-inflammatory diet may include:
- olive oil
- high fiber foods
- tomatoes
- nuts, such as walnuts and almonds
- leafy greens, including spinach and kale
- fatty fish, such as salmon and mackerel
- fruit, including blueberries and oranges

Fried and processed food may aggravate existing inflammation.
If you liked this article, you should check out our other posts in the Nebula Research Library!
June 13, 2023
