Table of contents
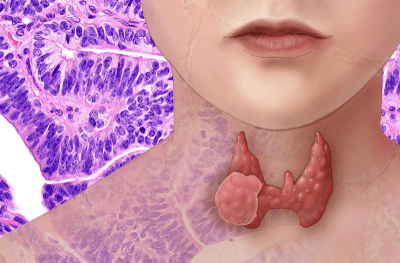
The thyroid is a butterfly-shaped gland located around the windpipe (trachea) at the base of your neck. It consists of two lobes that produce thyroid hormones that regulate metabolism, heart rate, blood pressure, and body temperature. Are you at risk? Read more to learn about genetic testing for thyroid cancer!
Cancer in this gland starts when thyroid cells grow out of control. At first, there might not be any symptoms at all. But, as it grows, it may cause discomfort and pain.
According to the American Cancer Society, there were about 44,280 new cases of thyroid cancer in the United States in 2021.
The thyroid gland is composed of two main types of cells:
- Follicular cells are in charge of producing hormones (TH) to regulate a person’s metabolism. Excess production of this hormone causes hyperthyroidism and lower than normal levels, hypothyroidism. The amount of this hormone depends on the thyroid-stimulating hormone (TSH), produced by the pituitary gland, located at the base of the brain
- Parafollicular cells (C cells) produce calcitonin, which controls the body’s use of calcium
- Lymphocytes, or immune system cells
- Stromal or supportive cells
Types of Thyroid Cancer
The type of cancer is determined by which type of cells are growing out of control. This is important to know as it helps establish how serious the cancer is and the best course of action for treatment.
Most tumors in the thyroid gland are benign. The malignant ones can spread to other parts of the body.
Examples of benign tumors are:
- Goiter is a condition in which the thyroid gland enlarges, either as a whole (diffuse) or with small nodules (nodular) in it. There are several reasons that may cause enlargement of the gland, and most of them are not cancer. One common reason for getting a goiter is a lack of iodine in the diet.
- Thyroid nodules, lumps, or bumps are usually not cancerous. Instead, these nodules tend to over-produce TH and produce hyperthyroidism.
The main types of thyroid cancers are:
Papillary thyroid cancer
This is the most common type (around 70% to 80% of cases). It grows slowly and develops from follicular cells. Papillary thyroid cancer can spread to the lymph nodes. The tumor looks similar to normal thyroid tissue under a microscope-a characteristic of differentiated thyroid cancer.
Follicular thyroid cancer
It is not as common as papillary thyroid carcinoma, but it also grows slowly from follicular cells. Follicular thyroid carcinoma is also a differentiated type that rarely spreads to the nodes.
Papillary and follicular thyroid carcinomas make up 95% of all cases. Most of the time, they are curable, especially when detected early and in younger people.
Hurthle cell cancer
Also called oxyphil cell carcinoma, this type makes up around 3% of the cases. It is a differentiated type, but it is harder to find and treat.
Medullary thyroid cancer (MTC)
MTC occurs in about 3% of cases and develops in the C cells. It can be treated if diagnosed before it spreads to other parts of the body. About 25% of MTC cases are familial, meaning that a patient’s family members might have a similar diagnosis.
Anaplastic thyroid cancer
This form is rare (around 1% of cases). However, it grows fast, making it particularly difficult to treat. Anaplastic thyroid cancer is undifferentiated and may start from a benign tumor or differentiated thyroid cancer.
Another classification is an indeterminate thyroid nodule, which may or may not be cancerous. Patients with indeterminate thyroid nodules are at a higher risk as up to 25% of these nodules turn into cancer.
Why Genetic Testing for Thyroid Cancer?
The exact cause of most of these cancers is yet unknown. Most people who develop a form do not have a family history or an inherited condition as a risk factor.
Changes in a person’s DNA can trigger cells to become cancerous. These changes can cause cells to grow abnormally at a faster rate or turn off tumor suppressor genes. Although we may inherit damaged DNA from our parents, most cancers are not caused by them. Alterations in genes happen during a person’s life and may be caused by environmental factors such as radiation or some random event inside the cell.
Genetic testing is recommended for people with a personal or family history of a specific type. For example, a condition known as multiple endocrine neoplasia type 2 (MEN2) is associated with medullary thyroid cancer. Individuals affected should get genetic testing. If a mutation is found in the RET gene of a person, their relatives should be genetically tested.
Benefits of genetic testing for thyroid cancer
Genetic testing has several benefits. We can mention the following:
- More targeted treatment has fewer side effects
- Patients can avoid unnecessary thyroid surgery
- Family members of a patient that tests positive for a gene mutation that may cause thyroid cancer can benefit from preventive surgery
- These cancers progress differently depending on the mutation associated with them
- This knowledge helps better prevent the potential development of a type of thyroid cancer
- Reduction of healthcare costs
Genes associated with thyroid cancers
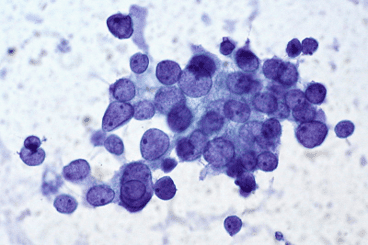
Nodules are usually detected during a routine physical exam. This is the first step into diagnosing thyroid cancer. Next, ultrasound imaging, blood testing, and fine-needle aspiration (FNA) biopsies can help plan better treatments according to the level of malignancy of the nodule.
Molecular markers found through these procedures can help predict how aggressive the disease is and predict the efficacy of therapeutic agents for each particular case.
Thyroid tumors may have some gene mutations. The following are some of the most relevant:
BRAF: Mutations in this specific gene are the most common and are typically found in papillary thyroid cancers. A BRAF mutation means that the risk of PTC is almost 100%. This gene alteration is also associated with aggressive forms of thyroid cancer and usually represents a higher risk of recurrence.
RAS: This is the second most common mutation and is usually associated with papillary or follicular thyroid cancer.
RET: Approximately 2 out of 10 medullary thyroid carcinomas (MTC) result from inheriting a damaged RET gene. These cases are known as familial medullary thyroid carcinomas (FMTC). The combination of FMTC and tumors in other endocrine glands is called multiple endocrine neoplasia type 2 (MEN 2).
PAX8-PPAR: Mutation in this gene is associated with follicular thyroid carcinoma.
APC: Patients with certain uncommon genetic conditions are at a higher risk of developing common forms of thyroid cancer. For example, defects in the gene APC cause familial adenomatous polyps (FAP) and a subtype of this syndrome called Gardner syndrome. These two conditions increase the risk of developing PTC, among other types.
PTEN: Changes in the gene PTEN cause Cowden disease, which puts patients at a higher risk of developing papillary or follicular thyroid carcinomas.
PRKAR1A: A syndrome known as Carney complex, type I, makes patients develop hormone problems and a series of benign tumors. They also are at an increased risk of papillary and follicular thyroid cancers. Defects in the gene PRKAR1A are responsible for Carney complex, type I.
Genetic Testing for Thyroid Cancer
Several genetic testing techniques can be applied depending on the type of tumor and suspected mutation. Some of these tests are:
Sanger Dideoxy Sequencing
This is the most widely used method to detect single nucleotide variants. Through this next generation sequencing technique, technicians copy target DNA sequences many times to create DNA fragments that are later separated.
Polymerase Chain Reaction (PCR)
This method is used to amplify a DNA sequence. This sequence is then used to identify markers at specific positions to confirm the presence of a mutation.
Fluorescence In Situ Hybridization (FISH)
This technique uses a tag with a fluorescent probe on DNA sequences of interest. These are then viewed under fluorescent microscopy.
Multiplex Ligation-Dependent Probe Amplification (MLPA)
This is a specialized form of PCR that identifies point mutations.
Afirma Gene Expression Classifier (GEC)
This new technology uses microarray technology to analyze messenger RNA expression of over 150 genes and was designed as a “rule out” test to more accurately diagnose patients and allow more patients to avoid surgery.
Types of genetic testing for thyroid cancer
There are a few commercially available genetic testing companies that test potentially dangerous nodules. The physician sends the nodule cells to these companies for genetic testing. This will help determine if the nodule is benign or malignant.
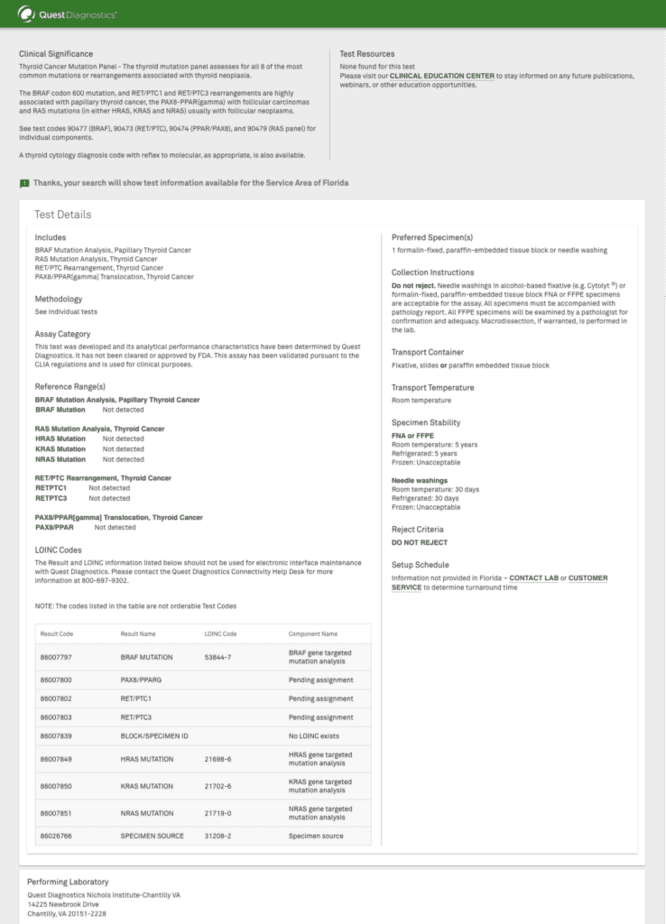
Quest Diagnostics
The objective of this company is to help physicians decide if there is a presence of thyroid cancer and if it needs surgical removal. This test consists of a panel with four gene markers:
- BRAF Mutation Analysis, Papillary Thyroid Cancer
- RAS Mutation Analysis, Thyroid Cancer
- RET/PTC Rearrangement, Thyroid Cancer
- PAX8/PPAR(gamma) Translocation, Thyroid Cancer
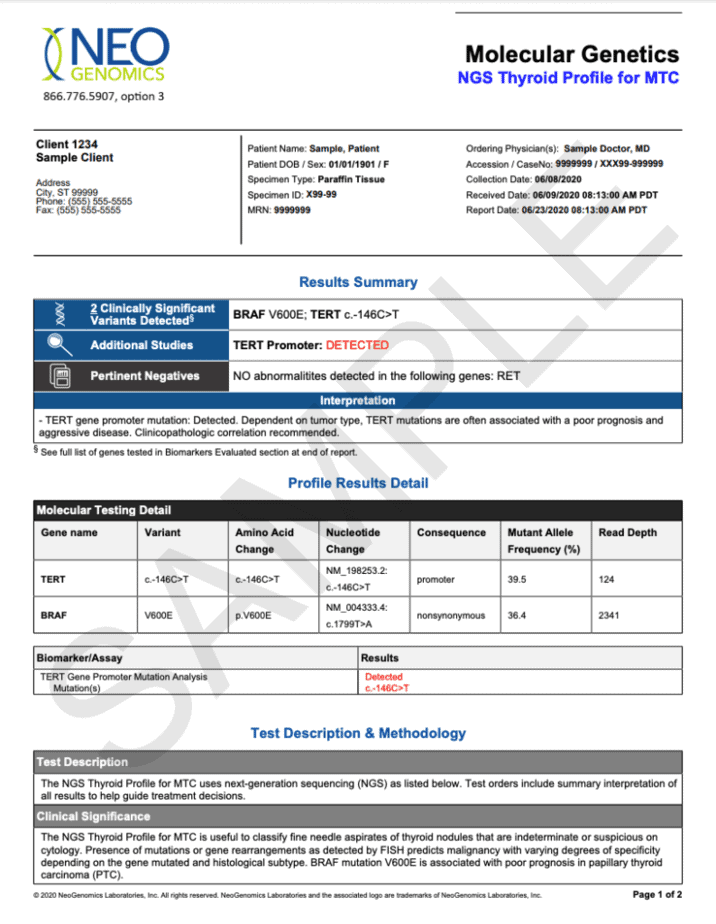
NeoGenomics
NeoGenomics offers its molecular testing services to patients with the advanced condition. They perform this under The Thyroid Cancer Testing Program sponsored by Lilly Oncology, a company that provides financial assistance to patients.
Patients eligible for this testing must be 12 years or older and have any of the following:
- Advanced or metastatic medullary thyroid cancer (MTC)
- Advanced or metastatic non-medullary thyroid cancer (non-MTC)
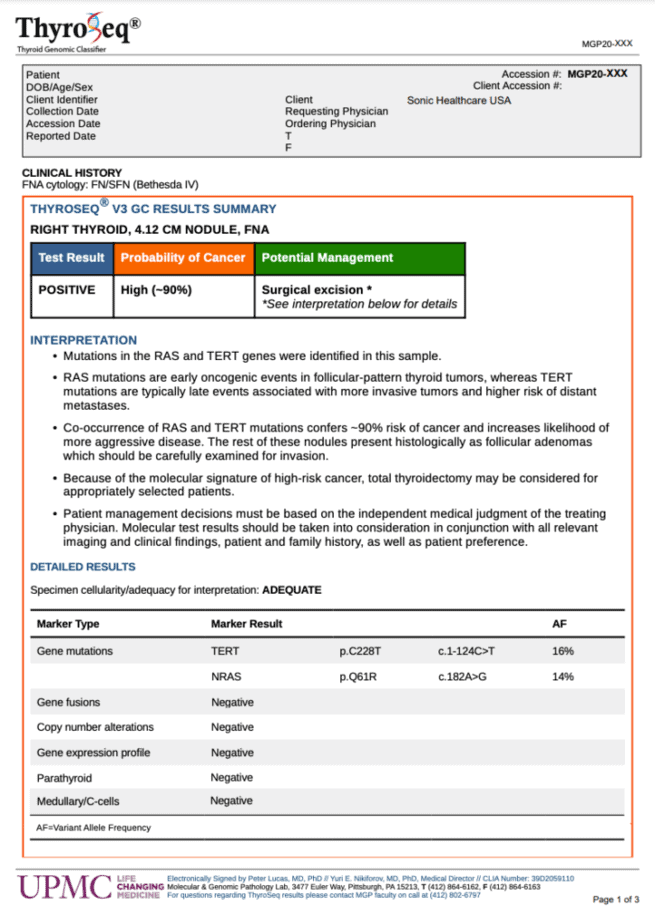
ThyroSeq
This is one of the most well-known genomic tests of this type. Branded as ThyroSeqⓇ Genomic Classifier, it distinguishes between benign and cancerous thyroid nodules using a tiny sample. The test aims to help avoid unnecessary diagnostic surgery.
If the test is positive, the report provides valuable information about the nodule to help the patient and physician decide on a customized treatment plan.
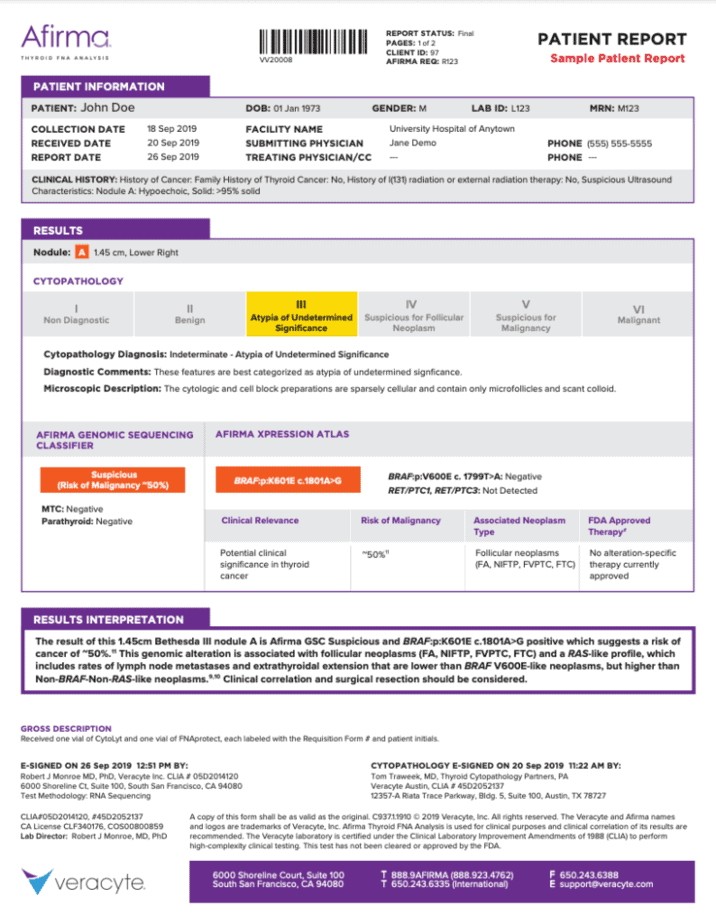
Veracyte (Afirma)
The Afirma Genomic Sequencing Classifier uses a “minimally invasive” fine needle aspiration (FNA) sample to assess potentially cancerous tissue. This test is known to detect MTC with almost 100% accuracy.
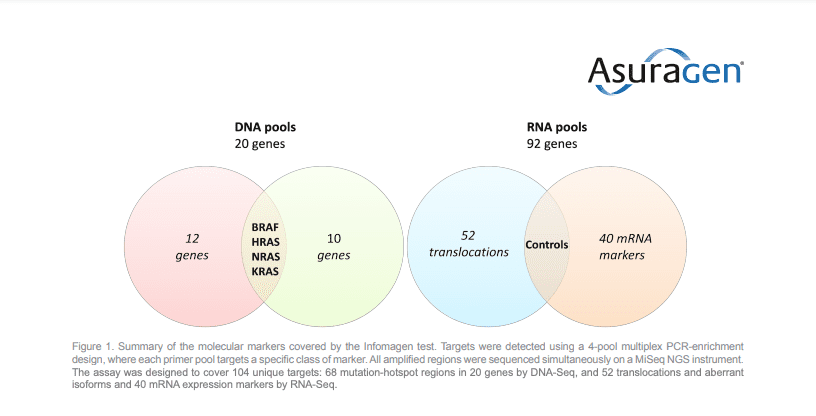
Asuragen
Since 2010, Asuragen has offered clinical testing for thyroid FNA biopsies through a product known as miRInformⓇ Thyroid. This test provides accuracy but not as much as it was needed. Asuragen then identified additional biomarkers associated with thyroid cancer. This led to the development of the Informagen NGS Thyroid Test in 2015, which significantly improved diagnosis and led to better treatment.
This test takes into consideration 20 genes involved in the disease and several relevant disease expression markers. The assay design includes four independent pools that are then combined into a single pool for sequencing.
Nebula Genomics
Nebula Genomics specializes in decoding the complete information hidden within your genes. Our 30x Whole Genome Sequencing (WGS) creates a full profile of your genetic composition. Nothing is left out, and you get valuable information that may include markers that may predispose you to cancer development.
Knowing your entire genetic composition is especially useful to help create a preventative program that reduces your risk of acquiring certain inherited diseases. This information is powerful, and you get to decide what to do with it to help avoid risks. While Nebula Genomics tests are not clinical tests, they are produced in labs of the highest quality and can be used in consultation with physicians and genetic counselors at various medical centers.
Get tested today and unravel the mystery that is not only your body composition but the blueprints that made it so.
For more information, you may want to check out the American Thyroid Association website.
If you liked this article, you should check out the other posts in the Genetic Cancer Testing series and explore the Nebula Research Library to learn about hundreds of other conditions influenced by genetics, including many cancers.
Other cancer genetic tests include:
- Colon Cancer Genetic Testing
- Pancreatic Cancer Genetic Testing
- Genetic Testing for Breast Cancer
- Genetic Testing For Prostate Cancer
- Ovarian Cancer Genetic Testing
- Lung Cancer Genetic Testing
Get your genome sequenced to receive personalized reports on all these conditions today!
November 16, 2021
Edited by: Christina Swords, PhD
