Nebula Genomics DNA Report for Lung Cancer
Is lung cancer genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
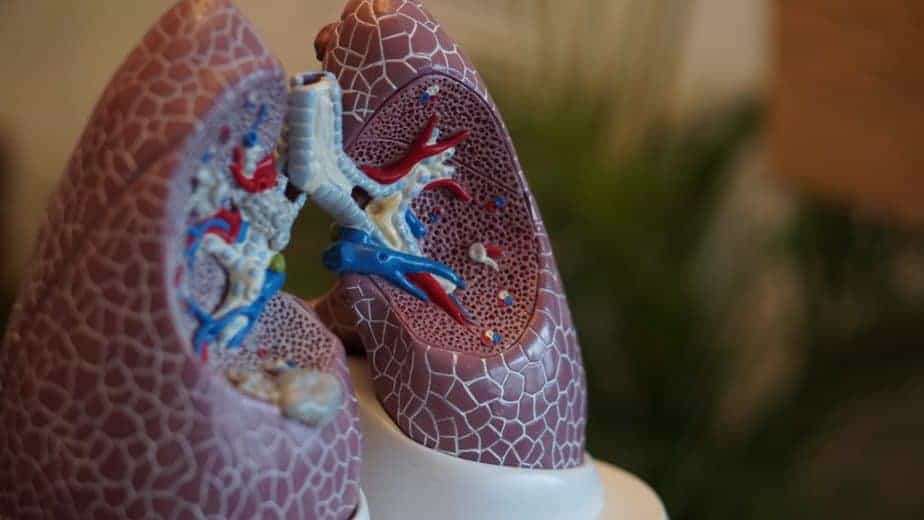
What is Lung Cancer?
Lung cancer is a malignant lung tumor in which cells that line the lung tissue divide uncontrollably and the cancer grows to form a tumor. About 98% of all lung cancers are carcinomas that originate from epithelial cells in the body. Another form, rarer than carcinoma, is sarcoma, which originates in the connective tissue (nerve, fat, muscle, bone). Other forms such as lymphomas and melanomas may also occur.
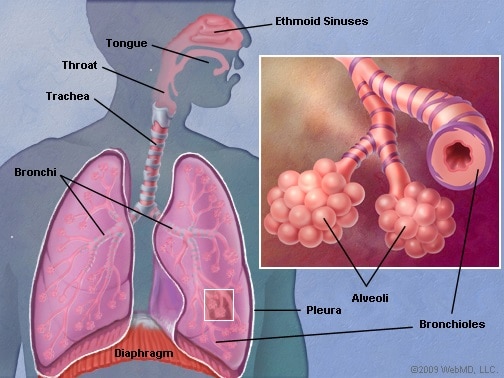
This disease is known for its ability to metastasize, or spread from the origin site to other parts of the body, after starting in the lungs. The two main types of lung cancer are non-small-cell lung cancer (NSCLC) and small cell lung cancer (SCLC). The main subtypes of NSCLC are lung adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Although they originate in different cells, experts group them together due to similarities in treatment and prognosis.
NSCLC accounts for 85 percent of diagnoses, while SCLC accounts for the remaining 15 percent. Common symptoms include coughing (possibly coughing up blood), weight loss, shortness of breath, and chest pains.
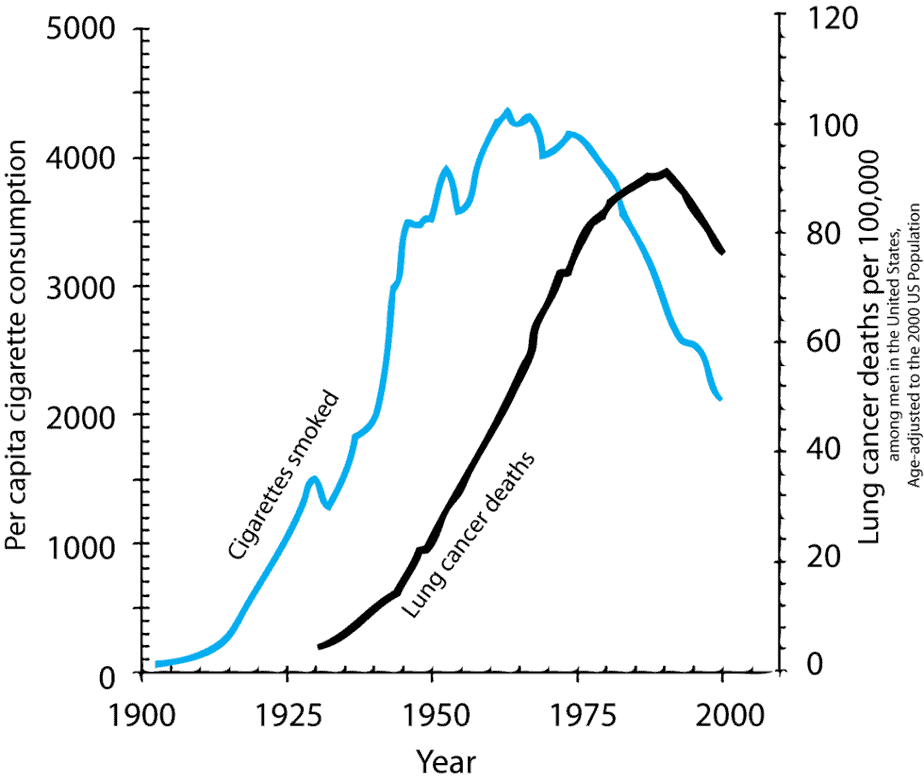
Smoking
Tobacco smoking is by far the most important risk factor for lung cancer. The history of lung cancer shows that patients increase the risk with an increased amount and duration of smoking. The American Lung Association estimates that tobacco products cause 90% of cases. However, lung cancer occurs in people who do not smoke as well.
Experts attribute the minority of cases not caused by smoking to radon, carcinogens, outdoor air pollution, and secondhand smoke.
The most important way to prevent the condition is through avoiding risk factors such as smoking and air pollution. There is no cure for lung cancer, and treatment largely depends on the type of cancer and the stage of the disease. If caught early, the prognosis tends to be better, almost to the point of a cure. Doctors may recommend chemotherapy, radiation, and/or surgery based on the overall case.
Is Lung Cancer Genetic?
Lung cancer can be genetic, but very few are hereditary. That is, lung cancer is caused by changes in the DNA acquired throughout a lifetime as opposed to being passed on from parent to child. Genetic mutations in the TP53, EGFR, and KRAS genes increase a person’s risk for lung cancer, even if they don’t smoke.
TP53: This gene codes for a protein, p53, in the nucleus that binds to DNA. It helps determine whether there is DNA damage and, if there is, whether it can be repaired or if the cell with the abnormal DNA should be self-destroyed through apoptosis.
Cancer destroys this protein’s ability to bind to DNA, resulting in an accumulation of DNA with errors and damage. These error cells continue to divide uncontrollably, carrying the damaged DNA with them. Changes to this gene occur in cases of both SCLC and NSCLC.
EGFR and KRAS: These genes both code for proteins in the cell membrane involved in cell proliferation. In cancerous cells, EGFR mutations and KRAS mutations cause the genes to be continuously turned on, prompting the cell to multiply all the time, resulting in a tumor. The majority of people with small cell lung cancer (NSCLC) have this type of mutation.
Experts link other acquired genetic mutations, such as the RB1 tumor suppressor gene, with the development of the lung cancer type SCLC.
Inheriting certain gene mutations such as those that cause faulty DNA repair mechanisms or a reduced ability to get rid of certain types of cancer-causing chemicals in the body may be at higher risk.
Current Research on Genetic Lung Cancer
When passed on, lung cancer has an autosomal dominant pattern (ADP).
A 2012 report on cancer genes describes this pattern. ADP means that the mutated gene is located on one of the autosomal (non-sex) chromosomes and that an individual only needs to inherit one copy of the altered gene from one parent in order to increase that person’s chance of disease development. However, the hereditary nature of the disease is not direct. That is, every person that inherits the genetic mutation is at higher risk of developing lung cancer, but not everyone will develop the disease.
All cancers are genetic. This means that they occur when mutations or alterations build up in critical genes that control cell growth and are responsible for repairing damaged DNA. Once these genes have alterations (caused by mutation) in their functioning, cells begin to grow uncontrollably and form a tumor. In most cases, people acquire the alterations over time during life, they do not inherit them.
TP53, EGFR, and KRAS
According to a 2017 NCBI cancer research report, acquired mutations in the TP53, EGFR, and KRAS genes are common in lung cancers.
The TP53 gene provides instructions for making a protein, called p53, located in the nucleus of cells throughout the body, where it attaches directly to DNA. The protein regulates cell growth and division by monitoring DNA damage. When DNA becomes damaged, p53 helps determine whether the DNA will be repaired or the cell will self-destruct and undergo apoptosis.
The epidermal growth factor receptor (EGFR) and KRAS genes each provide instructions for making a protein embedded within the cell membrane. When these proteins bind to other molecules, it triggers signaling pathways within cells that promote cell proliferation.
Experts have found that mutations in many other genes recur in lung cancer cases. Most of these genes are involved in regulating gene activity (expression), cell proliferation, the process by which cells mature to carry out specific functions (differentiation), and apoptosis.
Epidemiology
According to the Centers for Disease Control and Prevention (CDC), lung cancer is the third most common cancer in the United States. About 13% of all lung cancers are small cell lung cancers, and 84% are non-small cell lung cancers. It is the second most common in both men and women, only following prostate cancer and breast cancer in women. The average age of diagnosis is 70 years.
In 2021, the American Cancer Society estimated about 235,760 new cases and about 131,880 deaths from the condition. Overall, lung cancer accounts for 25% of all cancer-related deaths, making it the leading cause of cancer death in both men and women.
The incidences of lung cancer have been declining over the past few years, largely attributed to more people quitting smoking. In addition, advances in early detection and treatment have further served to reduce the death rate.
On average, men have a 1 in 15 chance, and women have a 1 in 17 chance of developing the condition in their lifetime. You have an increased risk of developing lung cancer if you are a smoker and a decreased risk if you are a non-smoker.
The risk of lung cancer is 15% higher in black men than white men and 14% higher in white women than black women. However, black men are less likely to develop SCLC than are white men.
Symptoms
Symptoms of the condition differ largely among patients, and patients do not exhibit symptoms until later stages of the disease. Because of the relatively few nerve endings in the lungs, early symptoms such as pain or discomfort go unnoticed. Often, doctors do not diagnose it until the later stages when specific symptoms become more pronounced.
Symptoms of lung cancer include:
- A cough that doesn’t go away and gets worse over time
- Hoarseness
- Constant chest pain
- Shortness of breath or wheezing
- Frequent lung infections such as bronchitis or pneumonia
- Coughing up blood
If the cancer has spread beyond the lungs and begins to affect other body systems, patients may also experience:
- Weight loss
- Loss of appetite
- Headaches
- Bone pain or fractures
- Blood clots
Causes
Environmental factors, particularly smoking, are the leading risk factor for lung cancer. As of 2021, experts linked smoking to about 90% of the cases of lung cancer, with many others to secondhand smoke. However, not everyone who smokes will get the disease, which suggests there are other risk factors that can increase or decrease the risk.
Non-smokers
Patients can develop lung cancer even if they have never smoked or stopped smoking. In these cases, people usually develop NSCLC as opposed to SCLC. Exposure to certain chemicals that influence the disease is the most common risk factor for people who don’t smoke.
These exposures can be radon, secondhand smoke, air pollution, or others. Workplace exposures to asbestos, diesel exhaust, or other chemicals can also cause lung cancers in some people who don’t smoke.
Patients with a family history of lung cancer may be at a high risk of developing the condition as well. This has less to do with genetics and more to do with cultural influences, such as smoking or living in an area with high air pollution.
Non-smokers may develop lung cancer at an earlier age. The tumors also tend to be different from those that occur in smokers.
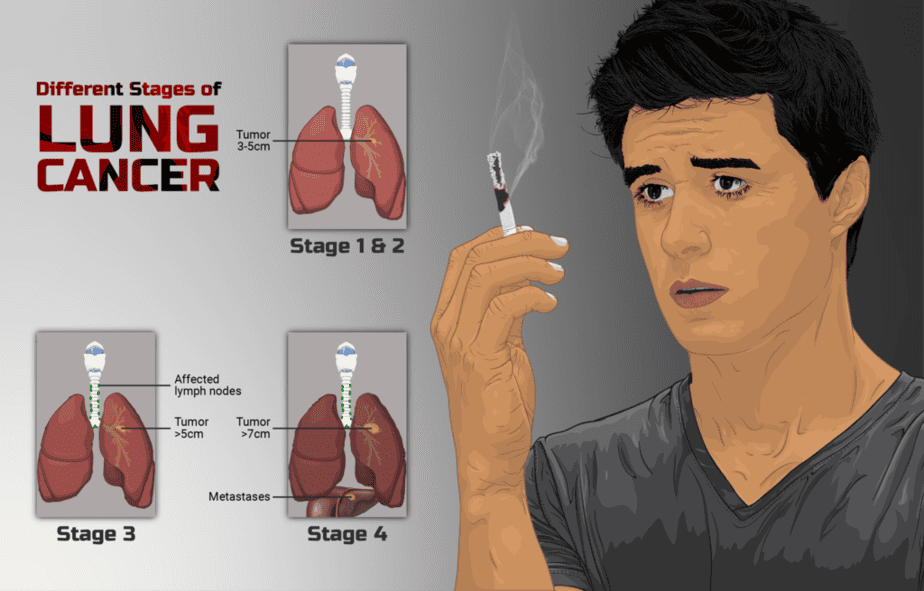
Diagnosis
Doctors normally diagnose the condition in persons 65 and older. Persons with higher risk may want to engage in screening on an annual basis at a younger age. Screening generally consists of observing the lungs with low-dose CT scans. Those who have smoked for many years (whether or not they are currently smoking now) or have other family members with the condition may want to talk with their doctor about this screening.
If your doctor suspects lung cancer, they may order the following tests:
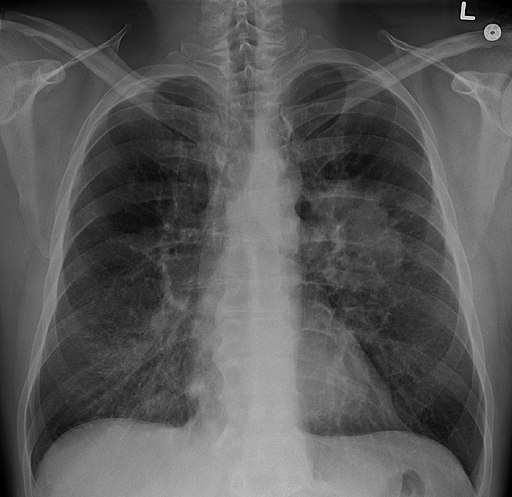
Imaging: Normally, the first diagnostic tests performed are x-rays and CT scans. These imaging tests will pick up on unusual masses or small legions.
Sputum cytology: If you are coughing persistently, looking at the produced sputum under a microscope may detect cancer cells.
Biopsy: To positively confirm the presence of the condition, a doctor will perform a tissue biopsy. In this procedure, a doctor removes a sample of cells from the affected area with the assistance of imaging technology and observed under a microscope. Experts can identify cancerous cells from their characteristics. Otherwise, a bronchoscopy can be performed in which a lighted tube is passed through the throat into the lungs, where the doctor can look for abnormalities.
Once a doctor confirms lung cancer, they may perform additional tests to determine its stage, which informs treatment options. Imaging tests, such as x-ray, CT scans, MRIs, and PET scans, will determine if the cancer has spread to other parts of the body. The extent of spread will classify the cancer in stages 0 to IV, with the lower stages indicating that the cancer is limited to the lungs and higher stages meaning it has spread.
Treatment
Treatment of lung cancer normally depends on factors such as the type and stage , as well as the overall health of the patient and personal preference. Some people with lung cancer may choose not to treat it, especially if the side effects of treatment outweigh the benefits. In these cases, there are options to treat the symptoms and make the patient comfortable.
Surgery
During surgery, surgeons will remove the lung cancer and some surrounding tissue. This can be either a wedge resection (small portion of the lung with the tumor and some surrounding tissue), segmental resection (larger portion of the lung), lobectomy (entire lobe of the lung), or pneumonectomy (entire lung).
A surgeon will typically perform surgery when the cancer is limited to the lung. The surgeon may also remove lymph nodes, which can carry cancer to other parts of the body, in the chest. If the cancer has spread to the lymph nodes, a doctor may recommend chemotherapy and radiation in combination with surgery.
Radiation therapy
This treatment uses high power energy beams to kill cancer cells. The patient lies on a table while the beams move around their body. This method is often used in combination with chemotherapy.
Chemotherapy
This treatment uses drugs to kill cancer cells. These medications are administered either intravenously or orally. In most cases, a combination of chemotherapy drugs is used. This method is often used in combination with radiation.
Targeted therapy
Some drugs are able to attack cancer cells by targeting certain cancer characteristics on the cells. There are a number of options for treatments, but most are reserved for patients with advanced stages of the disease.
Immunotherapy
This treatment bolsters your body’s immune system to better fight the cancer. It plays on reducing the cancer cell’s ability to hide from the natural immune systems. Most of these treatments are reserved for patients with advanced stages of the disease.
Palliative or supportive care in which patients work with their doctor to reduce signs and symptoms of the disease is also an important component of lung cancer treatment. Mood and quality of life are often improved when this component is included early in treatment.
For more information, you may want to check out the National Cancer Institute’s website or a review of the clinical practice guidelines for providers.
You can also see our posts in the Genetic Cancer Testing series and explore the Nebula Research Library to learn about hundreds of other conditions influenced by genetics, including many cancers.
May 18, 2023