Table of contents
What is Lung Cancer?
The leading cause of lung cancer is smoking. But what about the less than 20% of non-smokers that still get the disease? Lung cancer genetic testing has not only the answers to that but all the information you need to know about how the test works and its benefits.
Your lungs are two sponge-like organs located in your chest. The right one is composed of three sections or lobes, whereas the left one is composed of two. When you breathe, air goes inside via the trachea-what we usually call the windpipe.
The trachea divides into two tubes called bronchi, which branch out inside both lungs. The bronchi split into smaller sections called bronchioles, at the end of which we find the alveoli. This is where the exchange of oxygen and carbon dioxide in your blood takes place.
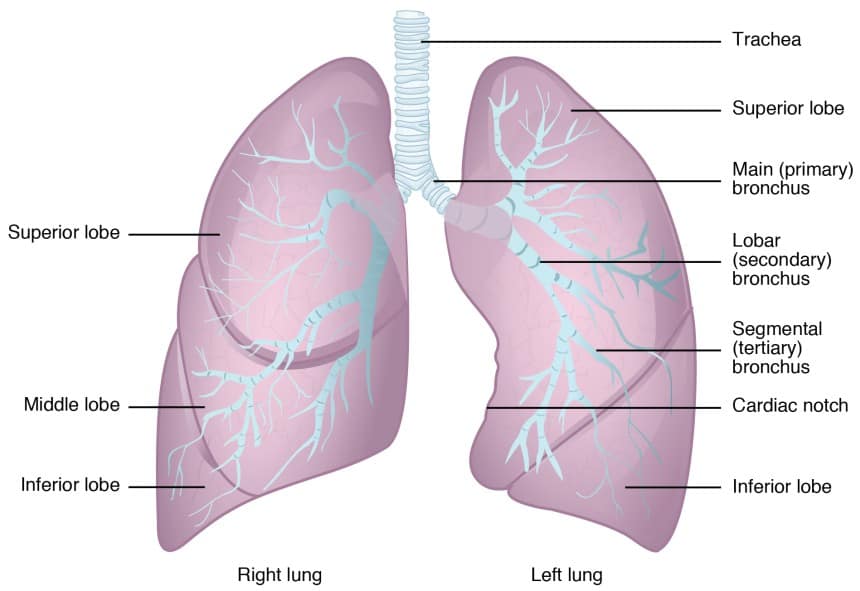
Typically, lung cancer starts in the cells that line the bronchi and other important sections, such as the bronchioles and the alveoli.
There are two main types of lung cancer:
- Non-small cell lung cancer (NSCLC). Around 80% to 85% are this type. They include adenocarcinoma, large cell carcinoma, and squamous cell carcinoma.
- Small cell lung cancer (SCLC). About 10% to 15% are this type. It grows faster than NSCLC, but it responds better to chemotherapy and radiation therapy.
Non-small cell lung cancer (NSCLC) is caused by more than one genetic mutation. The implication of this is that there are different decisions and treatments for the specific gene mutation causing the condition.
Why Genetic Testing for Lung Cancer?
Patients can greatly benefit from genetic testing for lung cancer. Doctors use this type of assessment to search for specific mutations and target cancer treatment accordingly.
Testing can also help rule out medications that may not be effective and cause serious side effects.
The American Lung Association explains that, through genetic testing, doctors can identify what changes in lung cells trigger and contribute to cancer growth through genetic testing. We know these changes as “biomarkers,” and doctors create a better approach to treatment for lung cancer by pinpointing them.
Perhaps one of the most significant benefits is that these targeted therapies do not destroy healthy cells as traditional treatments do.

Which genes are tested for lung cancer genetic testing?
Most of the genetic changes we have been talking about are found only in cancer cells, not healthy ones. This means that you cannot pass them on to your offspring.
Clinics specializing in lung cancer genetic testing use various technologies to screen for mutations in a large number of genes at once. The following are genes most commonly found with mutation testing:
EGFR mutation
EGFR (epidermal growth factor receptor) is a protein involved in cell division and growth. Around 10% of patients with non-small cell lung cancer have an anomaly in the gene responsible for producing this protein. This mutation is common in patients who have never smoked.
Targeted drug therapy for EGFR mutation lung cancer include the following inhibitors:
- Erlotinib (Tarceva)
- Getanifib (Iressa)
- Afatinib (Gilotrif)
- Osimertinib (Tagrisso)
- Dacomitinib (Vizimpro)
KRAS mutation
Clinics will also often test for a mutation in a gene called KRAS. About 25% of non-small cell lung cancer patients have a mutation in this gene. When this happens, cells will produce an altered protein that cannot regulate growth properly.
If your doctor detects this anomaly, they will prescribe a drug called Sotorasib (Lumakras) in pills, usually to take one a day. This inhibitor prevents the cancer cells from growing.
Rearrangement of the ALK Gene
When a mutation cannot be found in the EGFR or KRAS, it is probably is in the ALK gene. Close to 5 percent of patients with non-small cell lung cancer that have never smoked have this mutation.
The abnormality happens when ALK fuses with other genes. The most common one is EML4. When combined with this gene, a new mutant gene, EML4-ALK, emerges, causing changes in the functions of both genes.
The following are drugs that target an abnormal ALK protein:
- Crizotinib (Xalkori)
- Brigatinib (Alunbrig)
- Ceritinib (Zykadia)
- Alectinib (Alecensa)
- Lorlatinib (Lorbrena)
All of these drugs are taken as pills. They often shrink the size of the tumor in advanced patients with a change in gene ALK.
Other lung cancer biomarkers
As several biomarkers for lung cancer are found, the targeted treatment for each one becomes available. The following are some biomarkers that have treatments available.
- ROS1 rearrangement. This mutation is a fusion between ROS1 and another gene that results in the production of an abnormal protein.
- PD-L1 level. This is a protein that helps keep the immune system in check.
- NTRK fusion. When one chromosome piece containing an NTRK gene fuses with a gene in another chromosome, the result is called TRK fusion proteins, which leads to abnormal cell growth.
- BRAF V600E mutation. Common in smokers.
- RET rearrangements. An altered RET protein increases cancer spread.
- MET amplification. A mutation in the mesenchymal-epithelial transition (MET) gene triggers the production of abnormal proteins.
Who should get lung cancer genetic testing?
Most of the gene mutations that cause lung cancer are acquired. That is, they are triggered by external factors such as exposure to carcinogens. These somatic mutations are not present at birth and cannot be passed on to the offspring.
Anyone can develop a mutation that triggers lung cancer, so genetic testing is recommended for all patients. Although there is a type of lung cancer that can be passed from parent to child, hereditary mutations are far less common.
You should know what external factors put you at risk of developing the disease in its acquired form. If you feel you are at higher risk, you should speak with your doctor who can offer medical advice. Some of these risk factors are:
- Smoking (both passive and active)
- Asbestos
- Air pollution
- Radon
- Hormone replacement therapy
- Exposure to harmful chemicals or metals
Genetic Testing for Lung Cancer
When a patient is diagnosed with lung cancer, the next step is to take a genetic test to find the genetic mutation. This would be the biomarker that will help establish the most accurate line of action for treatment decisions.

There are two types of genetic testing for lung cancer tumor markers. They involve taking a tissue sample from a tumor or a blood sample.
Tissue biopsy
This is the standard procedure through which physicians obtain a sample for genetic testing. It involves saving a sample of a tumor during surgical removal.
Doctors can also get a sample of suspicious tissue to determine the exact cause of an abnormality and whether it is cancerous or not. If cancer is detected, this test will establish its molecular and genetic profile.
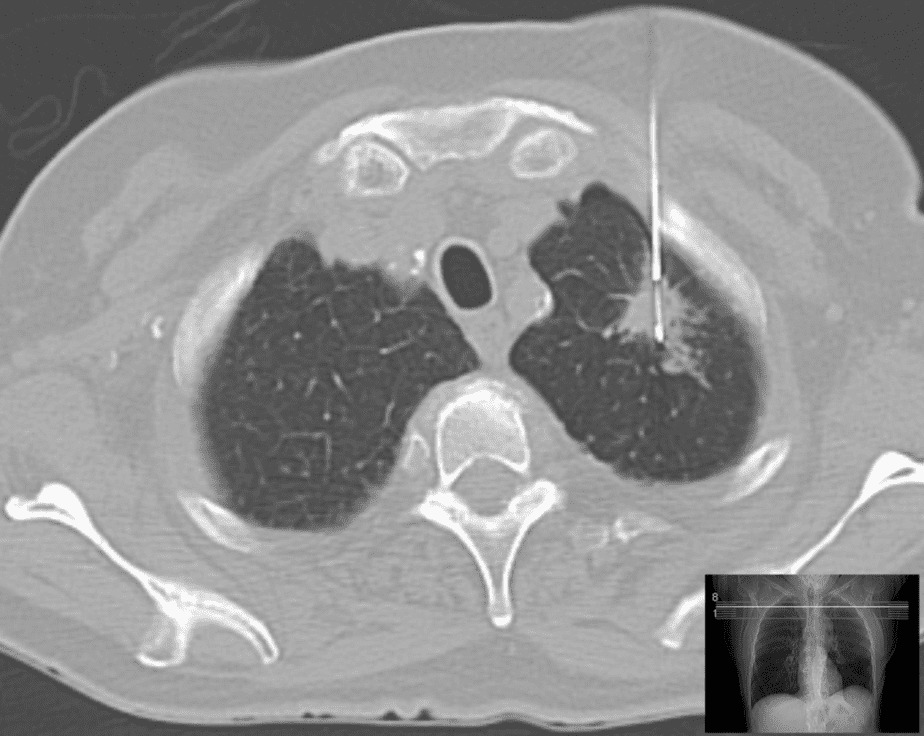
A tissue biopsy is done through several procedures. A pretty common one involves using a needle (needle lung biopsy) inserted from the back and into the lung. An ultrasound or a CT scanner helps guide the needle.
An open lung biopsy is much more invasive as it is done through surgery and, in some cases, may require separating the ribs or removing a portion of one. This method is used when all other ones have failed.
In a transbronchial biopsy, physicians obtain a sample during a bronchoscopy. This procedure involves inserting a scope down your mouth and into the upper airways of your lungs. When a scope is introduced through the chest wall and into the lung where the sample will be obtained, it is a thoracoscopic lung biopsy.
Liquid biopsy
Blood testing is used to find cancer cells that may be circulating in the blood. These cells are tested to detect the type of genetic mutation present. It is sometimes used in addition to the tissue biopsy.
Since this is a less invasive method, physicians will take blood samples to test how well a patient responds to treatment over time.
Nebula Genomics
Nebula Genomics has established itself as a benchmark in genetic testing. We offer plans that determine not only a tiny percentage of your genetic composition but your entire genome. Our 30x Whole Genome Sequencing (WGS) generates a complete genetic profile.
This information will help you create a program to lead a healthier lifestyle, among other things. Our at-home genetic tests are not meant to detect the genetic composition of potential lung cancer. The majority of these types of cancers are not inherited, and their biomarkers are specifically targeted. As we have seen, this requires a specialized procedure that currently takes place at specialized labs.
However, a Nebula Genomics test provides a clear picture of your genome and can be used to create a health profile that includes genetic predispositions to diseases such as lung cancer as well as other various health traits. Understanding your genes may influence your approach to health and this behavior change reduces your chances of acquiring lung cancer in any of its forms.
More information, including resources on treatment, research, and clinical trials, can be found on the National Cancer Institute’s website.
If you liked this article, you should check out the other posts in the Genetic Cancer Testing series and explore the Nebula Research Library to learn about hundreds of other conditions influenced by genetics, including many cancers.
Other cancer genetic tests include:
- Colon Cancer Genetic Testing
- Pancreatic Cancer Genetic Testing
- Genetic Testing for Breast Cancer
- Genetic Testing For Prostate Cancer
- Ovarian Cancer Genetic Testing
- Genetic Testing for Thyroid Cancer
Get tested today and open a window to new pathways of knowledge of your body and its blueprints.
November 2, 2021
Edited by Christina Swords, Ph.D.
