Table of contents
Nebula Genomics DNA Report for Thyroid Cancer
Is thyroid cancer genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Introduction
The thyroid is a butterfly-shaped gland located at the base of your neck. It produces hormones that regulate your heart rate, blood pressure, body temperature, amount of calcium in the blood, metabolism. Although it may not produce any symptoms at the early stage, it can grow and result in pain and swelling in the neck area. As tumors grow, signs of the disease include:
- A lump (nodule) that can be felt through the skin on your neck mass
- Changes to your voice, including increasing hoarseness
- Difficulty swallowing
- Pain in your neck (especially the front of the neck) and throat
- Swollen lymph nodes in your neck
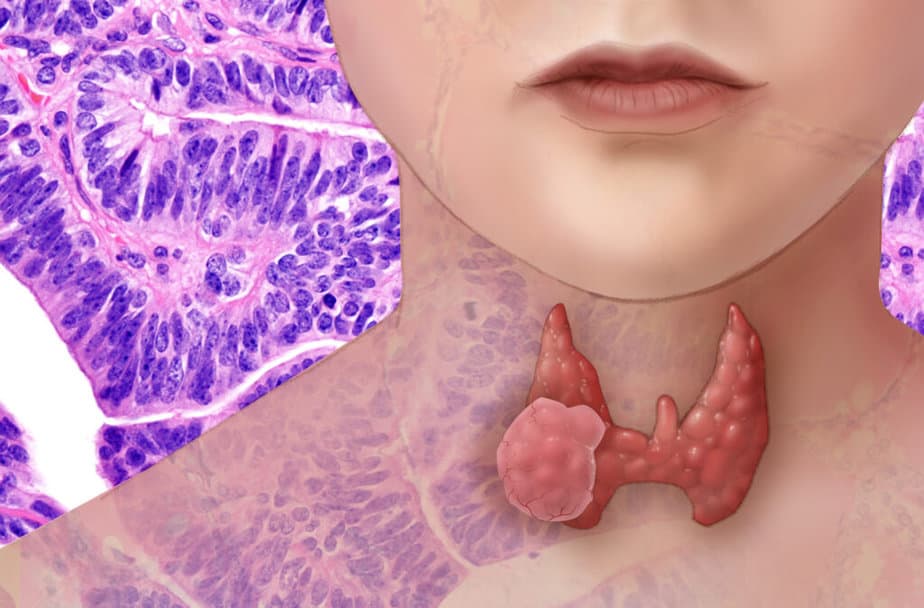
What is thyroid cancer? This cancer is generally slow growing and highly treatable. In aggressive forms, it may spread to lymph nodes, causing further complications. The thyroid cancer ribbon is three colors: purple, teal, and pink.
Epidemiology (Part 2 of Is thyroid cancer genetic?)
According to the American Thyroid Association, ATA, this type of cancer is rare relative to other cancer types. In recent decades, incidence has risen worldwide. There are significant differences depending on region and ethnicity. Experts contribute some of this increase to improved testing techniques.
This cancer is the eighth most common cancerous disease in the United States, accounting for 4% of all new cases. According to the National Cancer Institute, the rate of new cases of thyroid cancer was 15.7 per 100,000 men and women per year. The death rate was 0.5 per 100,000 men and women per year. Additionally, approximately 1.3 percent of men and women will be diagnosed with it at some point during their lifetime, based on 2015–2017 data.
Types
Thyroid cancer is the most common tumor of the endocrine system. It is divided into different types, of which the most common type often occurs in young adulthood. The age peak is on average 52 years for women and 55 years for men.
Disturbing thyroid nodules are usually the first symptom. The most common types of thyroid cancer include:
Papillary
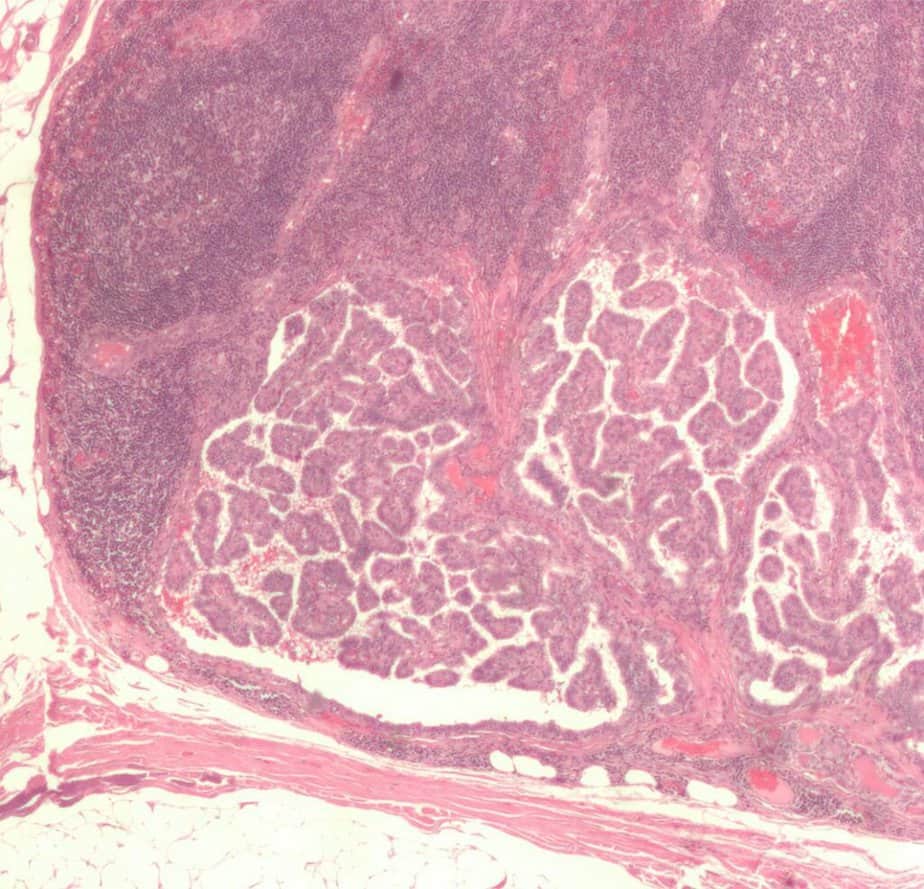
These are 75 to 85% of cases, normally occurs between ages of 35 and 60. These carcinomas originate from the thyroid cells and form finger-like branched (papillary) structures. They are the most frequent malignant neoplasms of this disease. They metastasize (spread to distant parts of the body) mainly via the lymph vessels (lymphogenic metastasis) into the lymph nodes of the neck.
Women with familial adenomatous polyposis and patients with Gardner syndrome have an increased risk of developing papillary thyroid cancer, papillary type. Defects in the gene APC cause these syndromes.
Follocular
These are 10 to 20% of cases, normally occurs between ages of 40 and 50. Doctors occasionally see this form of thyroid cancer in people with Cowden syndrome. Some include Hürthle cell carcinoma as a variant and others list it as a separate type. In this carcinoma, the tissue structure largely resembles the structure of a mature or developing thyroid gland. The diseased cells originate from the thyroid cells and form metastases (distant metastasis) in the lungs, skeleton and brain, and blood vessels, mainly via the bloodstream.
Medullary
These are 5 to 8% of cases, normally occurs between ages of 40 and 50. Cancer of the parafollicular c cells, calcitonin-producing cells (also called C-cells), which are located in the thyroid gland due to developmental connections, but are not related to the actual thyroid function.
Anaplastic
These are less than 5% of cases, normally occurs around 60 years of age. It is not responsive to treatment and can cause pressure symptoms. Chemotherapy may be recommended as a treatment of anaplastic thyroid cancer at the time of diagnosis.
Poorly differentiated thyroid cancer is a malignant neoplasm of follicular cell origin showing intermediate histopathological patterns between differentiated and undifferentiated thyroid cancers
Is Thyroid Cancer Genetic?
The causes are not fully understood in detail although a combination of environmental and genetic factors are each thought to play some role, especially for the hereditary forms.
Familial medullary thyroid carcinoma (FMTC), occurring in about 2 out of 10 medullary thyroid carcinomas (MTCs), results from inheriting an abnormal gene.
According to the American Cancer Society, experts call the combination of FMTC and tumors of other endocrine glands “multiple endocrine neoplasia type 2 (MEN 2)”. There are 2 subtypes, MEN 2a and MEN 2b, caused by genetic mutations in the RET gene.
“In MEN 2a, MTC occurs along with pheochromocytomas (tumors that make adrenaline) and with parathyroid gland tumors.
In MEN 2b, MTC is associated with pheochromocytomas and with benign growths of nerve tissue on the tongue and elsewhere called neuromas. This subtype is much less common, but also more aggressive, than MEN 2a.”
In these inherited forms of MTC, the cancers often develop during childhood or early adulthood and can spread early. Having a first-degree family member (parent, brother, sister, or child) with the disease, even without a known inherited syndrome in the family, increases your risk of thyroid cancer.
The papillary type often runs in families. Experts suspect genes on chromosome 19 and chromosome 1 of causing these familial cancers.
Persons who have Carney complex, type I or Cowden disease have a higher risk of developing thyroid cancer, both papillary and follicular. Defects in the gene PRKAR1A cause the former while defects in the gene PTEN most often cause the latter.
Non-genetic Causes
This disease occurs more often in women than in men.
There is also a causal connection with iodine deficiency (about 2.3 times higher risk). Radiation (especially in childhood and adolescence) also plays a significant role. After the atomic bombs were dropped on Hiroshima and Nagasaki, the risk of this cancer increased many times over in the affected areas. The same applies to the areas affected by massive radioactive fallout after the Chernobyl disaster.
People living in the United States during the atomic bomb tests between the 1940s – 1960s may also be exposed. The radioactive substance, Iodine 131 (or I-131) released from these atomic explosions collects in the thyroid gland, which causes the increased risk. You can reduce your risk by avoiding areas with high levels of radioactivity.
Symptoms
When thyroid cancer develops, doctors and patients notice a nodule formation in the area of the thyroid gland. This gland is either enlarged or normal in size. Enlarged neck lymph nodes can also appear before a palpable thyroid node. Dysphagia, hoarseness as an expression of vocal cord nerve paralysis, a lack of thyroid gland ability to shift the swallowing action, rough consistency, and fused lymph nodes are late symptoms of thyroid cancer.
Diagnosis
A medical provider will physically examine the neck area to check for indications of an enlarged thyroid. They will also inquire about thyroid cancer risk factors such as radiation exposure and personal or family history of thyroid cancer. Minimally invasive tests such as blood tests, ultrasound imaging tests on the neck, PET scans, and CT scans may help the doctor determine whether the organ is functioning properly and if suspicious nodules are present.
Doctors may acquire a fine needle aspiration (thin needle) biopsy of the thyroid tissue to determine if cancerous cells are present. In the case of medullary thyroid cancer, the doctor may recommend a genetic test and/or genetic counseling to look for genes that may increase your risk for other cancers. To learn more about clinical DNA tests, take a look at our blog. You may be particularly interested in:
- Ambry Genetics – risks of various disease types
- Color – risks of cancer, genetic forms of heart disease, and medication responses
- Invitae – diagnostics, proactive health, and reproductive health
- Myriad Genetics – diagnostics, reproductive tests, and precision medicine tests
- Veritas Genetics – disease risks and carrier screenings
Some very small tumors that have a low risk of spreading in the body might not need treatment right away. Instead, you might consider active surveillance with frequent monitoring of the cancer. Monitoring might require blood tests and a thyroid cancer ultrasound exam of your neck once or twice per year.
Treatment
To treat thyroid cancer, treatment options include thyroid surgery to remove all or part of the thyroid, radioiodine therapy, and radiation therapy.
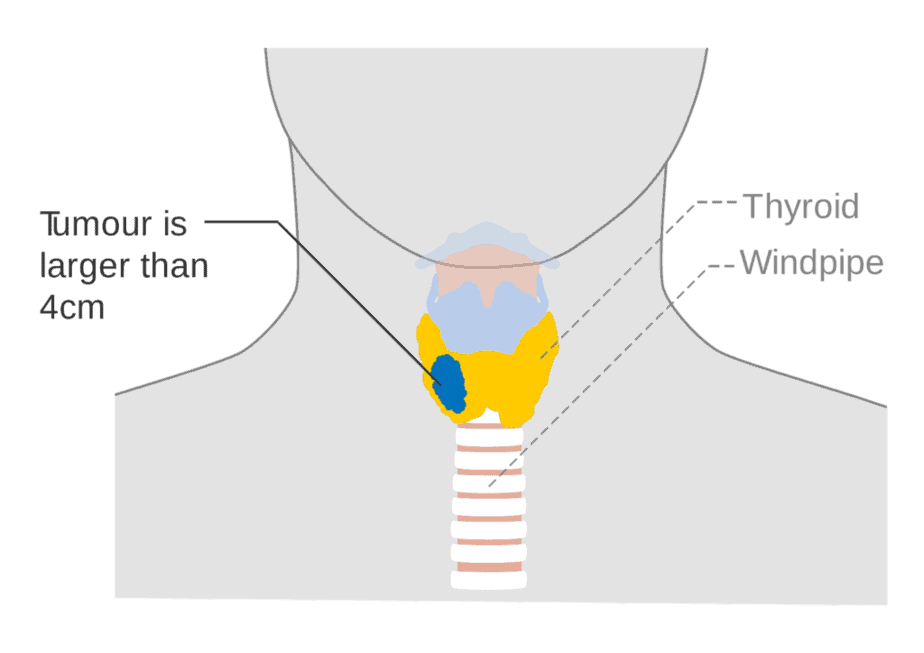
Surgical removal
In most cases, surgeons may completely remove the gland (total thyroidectomy). If the disease is not aggressive, medical providers may choose to save some of the thyroid (thyroid lobectomy), especially if the patient is under 45 years old. Doctors diagnose the majority of these cancers before they have metastasized, or before the disease spreads outside of the thyroid.
An exception is the so-called microcarcinoma. In this case, surgeons remove only the affected lobe and do not perform subsequent radioiodine therapy.
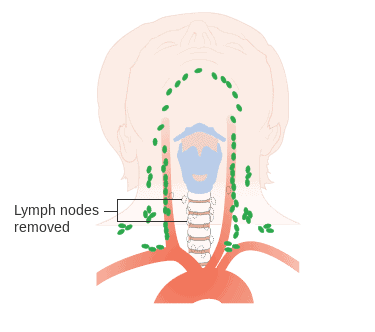
In addition to the removal of the gland, occasionally surgeons also remove the lymph nodes around that area (lymphadenectomy), since the cancer can also affect the lymph nodes. However, at least in the case of papillary and follicular thyroid cancers, experts only recommend this if there is clinical evidence or suspicion of regional lymph node metastasis. In medullary thyroid carcinoma, the corresponding guidelines recommend unilateral or even bilateral cervical lymphadenectomy.
Following the operation, doctors replace the gland function with thyroid hormone replacement therapy called levothyroxine. This medication supplies the missing hormone the organ would normally produce, and it suppresses the production of thyroid-stimulating hormone (TSH) from your pituitary gland, which could stimulate any remaining thyroid cancer cells to grow.
Radioactive iodine therapy
After surgery, iodine-storing carcinomas are followed by radioactive iodine treatment to remove the postoperative remaining thyroid tissue (ablation) in cases of papillary or follicular carcinoma. Doctors administer radioactive iodine-131, which accumulates exclusively in the gland tissue. Some side effects of this therapy include:
- Metallic taste in your mouth
- Dry mouth
- Sore throat
- Neck pain
- Nausea or vomiting, which is usually mild
- Constipation or diarrhea
- Fatigue
- Unusually low (hypothyroidism) or unusually high (hyperthyroidism) thyroid levels
Treatment of advanced carcinoma
Advanced carcinoma is defined as a thyroid carcinoma with distant metastases (e.g. lung metastases) or a non-operable carcinoma. In this case, a complete cure is usually no longer possible. The aim of the therapy is to prolong life with the highest possible quality of life and to reduce thyroid tumor-related symptoms.
Several tyrosine kinase inhibitors (TKI), a type of targeted therapy, have been approved for metastatic differentiated cancer that no longer responds to radioiodine therapy, including sorafenib and lenvatinib. Cabozantinib and vandetanib are approved for advanced medullary cancer. Clinical trials for other drugs are ongoing.
Radiation therapy
External radiation therapy may be advised if surgery isn’t an option and the cancer grows after radioiodine therapy. Doctors may also recommend radiation therapy after surgery if there’s an increased risk that your cancer will recur.
Recurrence
This disease may come back, even after surgery and treatment. This could happen if diseased cells spread to other areas of the body before the gland is removed. Reoccurrence may happen in:
- Lymph nodes in the neck
- Small pieces of thyroid tissue left behind during surgery
- Other parts of the body, such as the lungs and bones
It is important to monitor signs and symptoms with a medical provider long term.
Prognosis and Survival Statistics
Differentiated carcinomas
In most cases, average 10-year thyroid cancer survival rates are more than 90% for these thyroid cancer patients undergoing management of papillary thyroid carcinoma and approximately 80% for the follicular variant (on treatment). According to the National Cancer Institute, the overall 5-year survival rate for patients with thyroid cancer is 98%.
Prognosis factors include patient age as well as tumor type and stage, tumor size, spread and histological differentiation; lymph node metastases do not appear to significantly affect the prognosis. Due to the higher risk of thyroid cancer recurrence, consistent follow-up is extremely important.
Medullary and anaplastic thyroid carcinoma
The following 5-year survival rates for patients with anaplastic thyroid cancer and medually cancer apply on average (at treatment):
- Medullary carcinoma: 60-70%
- Anaplastic carcinoma: about 5 %
Did you know you can test for thyroid hormone levels at home? Learn more in our article about at home thyroid tests.
You can also see our posts in the Genetic Cancer Testing series and explore the Nebula Research Library to learn about hundreds of other conditions influenced by genetics, including many cancers.
January 26, 2023
