Table of contents
Nebula Genomics DNA Report for High Blood Pressure
Is high blood pressure genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of May 2021. |
What is High Blood Pressure?
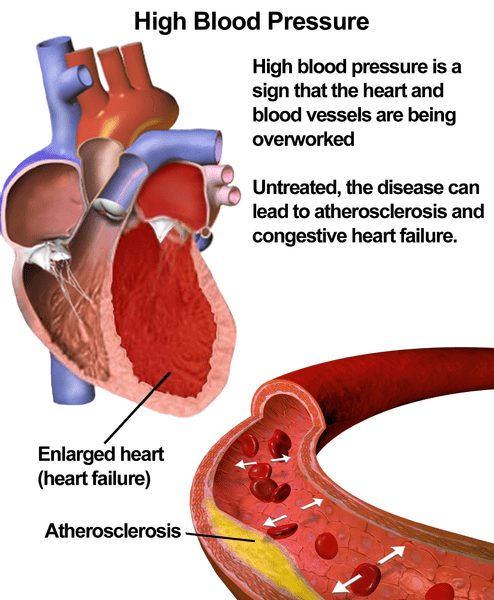
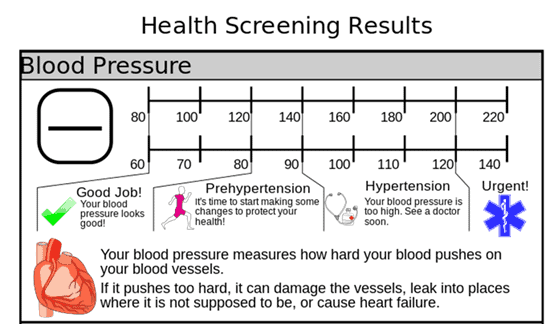
High blood pressure, or hypertension, is a medical condition in which the blood pressure of the arterial vascular system is chronically elevated. Eventually, the force of the blood against artery walls causes additional damage. When measuring blood pressure, the top number is defined as systolic blood pressure and measures the pressure in your arteries when your heart pumps blood. The bottom number is diastolic pressure, which measures the pressure in your arteries in between beats.
According to the Centers for Disease Control and Prevention (CDC) revised guidelines, high hypertension is blood pressure at or above 130/80 mm Hg. Stage 2 hypertension is defined as blood pressure at or above 140/90 mm Hg. This definition does not include temporary increases in blood pressure due to illness, medication, pregnancy, or during physical exertion.
Is High Blood Pressure Genetic?
High blood pressure runs in families. For example, if your parents already suffer from high blood pressure, you are at a higher genetic risk of developing hypertension. The condition is most likely a combination of many genetic variants.
More than 100 genetic variations have been associated with primary hypertension. While these variations have been found more commonly in people with essential hypertension than in unaffected individuals, none are common causes of the condition.
The most studied genetic association in essential hypertension is with genes involved in the renin-angiotensin-aldosterone system. This system produces hormones to regulate blood pressure and the balance of fluids and salts in the body. These genes play an essential role in normal blood pressure control.
AGT: This gene controls the production of the protein angiotensin. Angiotensin is eventually converted to a form called angiotensin II, which serves to narrow blood vessels. Angiotensin II produces the hormone aldosterone, which ultimately facilitates absorption of salt and water by the kidneys. The increased amount of fluid in the body also increases blood pressure.
AGTR1: This gene controls the production of the angiotensin II receptor type 1 (AT1 receptor). Angiotensin II binds to the AT1 receptor to stimulate chemical signaling. This signal controls the narrowing of blood vessels and stimulation of the hormone aldosterone.
Other genes associated with essential hypertension are essential for the lining of blood vessels (the vascular endothelium). Changes in these genes are thought to impair this cell layer. Such changes may result in vessels that are abnormally constricted or narrowed, which raises blood pressure.
Researchers suspect epigenetic changes to the DNA also play a role in the development of primary hypertension. Epigenetic changes modify DNA without changing the DNA sequence. They can affect gene activity and the production of proteins, which may influence blood pressure.
Genetics may have an important role in drug development for hypertension by revealing which drug targets are best for certain patients.
Current Research On Genetic High Blood Pressure
A study was published in Scientific Reports titled “Examining the effect of mitochondrial DNA variants on blood pressure in two Finnish cohorts.”
Since the effect of mitochondrial DNA single-nucleotide polymorphisms (mtSNPs) on BP is less understood than that of nuclear SNPs, the research sought to examine the mitochondrial genetic determinants of systolic, diastolic, and mean arterial BP.
Its results agree with several previous studies suggesting that mtDNA variation does not significantly impact BP regulation.
Another research study was published in Kidney360, titled “Association of Blood Pressure Genetic Risk Score with Cardiovascular Disease and Chronic Kidney Disease Progression: Findings from the CRIC Study.”
The study investigated whether blood pressure genetic risk predicts cardiovascular disease and kidney failure progression in patients with chronic kidney disease.
It found that higher genetic risk was not associated with chronic kidney disease progression. Thus, it concluded that while genetic risk for elevation in blood pressure was associated with increased risk of cardiovascular disease, it did not contribute to chronic kidney disease progression.
Epidemiology
According to the Centers for Disease Control and Prevention, hypertension is a major condition for nearly half of adults in the United States (108 million, or 45%). People with high blood pressure will have a systolic blood pressure above 130 mm Hg or a diastolic blood pressure greater than 80 mm Hg or are under hypertension treatment.
High blood pressure puts patients at risk for life-threatening diseases, such as heart disease and stroke, which are leading causes of death in the United States. In 2018, nearly half a million deaths in the United States included hypertension as a primary or contributing cause.
A greater percentage of men (47%) have high blood pressure compared to women (43%). The disorder is also more common in non-Hispanic black adults (54%) than in other ethnicities, including non-Hispanic whites.
There also appear to be differing levels of prevalence based on geography, with more cases in the southeastern United States than in other areas of the country.
Symptoms
Hypertension is often asymptomatic and can go undetected for years. In many cases, it only becomes noticeable through the subsequent damage, which is why it is sometimes also referred to as the “silent killer.”
A typical symptom is a headache occurring in the morning, which can be reduced by raising the head of the bed. Other possible symptoms include nausia, dizziness, nosebleeds (epistaxis), fatigue, and insomnia. If blood pressure is severely elevated, shortness of breath (dyspnea) on exertion, angina pectoris, and visual disturbances may occur. Noticeable changes in the feeling of thirst, in the frequency of urination, in the tendency to sweat, or in the ability to exert oneself may also be signs of elevated blood pressure.
Causes
The risk of developing the condition is generally a combination of genetic and lifestyle factors.
Primary hypertension
This is the most common form of high blood pressure. It builds up gradually over time, and in most cases, there is no underlying cause. However, genetics, physical changes to your body, and environmental risk factors are thought to play a role.
Secondary hypertension
In this case, patients develop high blood pressure as the result of an underlying condition. It is not as common as primary hypertension. It tends to come on suddenly, and the blood pressure value is often higher than in primary hypertension. Some disorders that are known to contribute to hypertension include:
- Obstructive sleep apnea
- Kidney disease
- Adrenal gland tumors
- Thyroid problems
- Certain congenital anomalies in blood vessels
- Certain over-the-counter pain relievers, some prescription drugs, birth control pills, cold remedies, and decongestants
- Illegal drugs, such as cocaine and amphetamines
Environmental risk factors
The risk factors for high blood pressure are similar to those for any cardiovascular disease, including heart attack and stroke. You may want to talk to your doctor if you have a number of the following risk factors that affect blood pressure:
- Age. The risk of high blood pressure increases with age.
- Race. African Americans tend to have an increased risk at a younger age than other ethnicities
- Family history
- Being overweight or obese
- Not being physically active
- Smoking or chewing tobacco
- Too much salt (sodium) or too little potassium in your diet
- Too much alcohol
- Stress
- Health problems that include certain chronic conditions

Diagnosis
Because the disorder is often asymptomatic and the symptoms are nonspecific, the only way to know if you have hypertension is to get regular blood pressure readings to check if your blood pressure rises. Most doctors’ offices take a blood pressure reading at every appointment.
This test is performed by placing a pressure cuff around the upper arm before manually or electronically inflating it. This inflated cuff momentarily stops the blood flow by compressing the artery. The specialist will then slowly release the air in the cuff while listening to the patient’s pulse with a stethoscope. More advanced methods use sensors in digital devices to monitor artery vibrations.
Blood pressure readings are divided into 5 categories:
| Reading systolic / diastolic (mm Hg) | Type |
|---|---|
| 120 / 80 | Normal |
| 120 – 120 / 80 | Elevated (also called prehypertension) |
| 130 – 139 / 80 – 89 | Stage 1 hypertension |
| ≥ 140 / ≥ 90 | Stage 2 hypertension |
| ≥ 180/120 | Hypertensive crisis |
The American Heart Association recommends that if you are within the normal range (less than 120/80 mm Hg), you should screen your blood pressure yearly during regular medical visits if you are 20 or older. If you have a family history of heart disease or other risk factors, your doctor might recommend you get readings more often than regular appointments.
Treatment
Controlling blood pressure is usually a combination of lifestyle changes and prescription medications. It is important to note that this article does not provide medical advice. Patients should speak with a healthcare professional.
Lifestyle changes
Changes to diet and exercise are typically the first treatment options patients discuss with their doctor. The change includes:
- Eating a heart-healthy diet with less salt
- Getting regular physical activity
- Maintaining a healthy weight or losing weight if you’re overweight or obese
- Limiting the amount of alcohol you drink
If changes to diet and exercise are not enough, your doctor may recommend medication to help keep blood pressure down.
Prescription medications
If medication is needed to manage high blood pressure, doctors often prescribe two or three different ones simultaneously. The combination appears to work better than a single treatment alone. Sometimes, it takes time and multiple tries to find a combination that works best for an individual.
Diuretics: These medications help your kidneys eliminate sodium and water from the body. Unfortunately, a side effect of the drugs is increased urination, which may also eliminate too much of the healthy potassium.
Angiotensin-converting enzyme (ACE) inhibitors: These medications help relax your veins and arteries by blocking the formation of angiotensin II, an enzyme that narrows blood vessels.
Angiotensin II receptor blockers (ARBs): These medications relax blood vessels by blocking the action, not the formation, of a natural chemical that narrows blood vessels.
Calcium channel blockers: These medications are used as antihypertensive drugs and help relax the muscles of your blood vessels. Some slow your heart rate. Calcium channel blockers may be more effective for older people and people of African heritage than do ACE inhibitors alone. It’s important not to consume grapefruit while on these drugs as it can raise levels of certain calcium channel blockers to a dangerous level.

If a combination of the treatments above isn’t effective, additional medications may be added, including alpha-blockers, beta-blockers, alpha-beta blockers, aldosterone antagonists, renin inhibitors, vasodilators, and central-acting agents.
A doctor may also recommend that a patient monitors their blood pressure level regularly at home. Home monitors are widely available and inexpensive, and you don’t need a prescription to buy one. It’s important to note that monitoring your blood pressure at home isn’t a substitute for visits to your health care professional.
To learn more about risk factors, diagnosis, and treating hypertension, you should look at the resources provided by the National Heart, Lung, and Blood Institute (a member of the National Institutes of Health, NIH) on their website.
In October 2020, former United States Surgeon General Jerome M. Adams, M.D., M.P.H issued a call to action on hypertension control, including a document that provides strategies for medical providers on how to address this issue. The resource and video can be found on the website of the U.S. Department of Health and Human Services.
This report is based on the results of a genome-wide association study conducted by a large group of international researchers in 2018. The research group published their results in Nature Genetics. If you liked this article, you should check out our other posts in the Nebula Research Library!
July 12, 2022
