Table of contents
Nebula Genomics DNA Report for Snoring
Is snoring genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Introduction
From a biological standpoint, snoring is the vibration of the respiratory structures due to obstructed air movement when a person breaths through their nose and throat during sleep. The result that most people recognize is the hoarse or harsh sound made during a person’s sleep. For some people, snoring is soft and infrequent. For others, it can be a chronic nuisance that bothers bed partners during night sleep and may even signal a serious health condition.

Many people experience snoring and sleep apnea. It has also been linked to sleep deprivation. Lifestyle factors can help reduce snoring. Such recommendations to help reduce the condition usually include losing weight, sleeping on your side, and avoiding alcohol before bedtime.
Is Snoring Genetic?
There is no “snoring gene” linked to people who snore. However, there have been several studies over the years that have associated over 100 genetic variants with snoring at some level.
A paper published in 1995, “Snoring, family history, and genetic markers in men. The Copenhagen Male Study”, concluded that there was a strong association between the condition and family history of snoring.
Experts observe a similar effect with OSA where snoring is a combination of genetic factors, health, and lifestyle. Many genes appear associated with the condition, each contributing to the disease in a small amount. Most variations have been identified in single studies, and follow up research has not verified them. According to MedLinePlus, genes involved could be those that control communication between nerve cells, breathing regulation, control of inflammatory responses by the immune system, development of tissues in the head and face, the sleep-wake cycle, and appetite control.
There does appear to be some family history and genetic factors as the risk of developing this condition is about 50 percent greater for first-degree relatives (such as siblings or children who snore) of affected individuals as compared to the general public.
Epidemiology
A survey study in Turkey from 2005 found that the habitual snoring prevalence was 8.9% in females and 29.5% in males. This study also found that males over 40 who had issues with obesity and engaged in smoking and drinking alcohol had the greatest risk of developing the condition. Hypertension and coronary heart disease were statistically more common in individuals with habitual snoring.
In the United States, snoring and sleeping disorders may affect up to 40% of children and up to 49% in adults. Habitual snoring is present in 2.4–15% in children and in 10–36% of adults. As with the other study, it was more common in men than in women. Among college students, it was present in 37% of Asians, 31% of Hispanics, 27% of Caucasians, and 24% of African Americans.
Another study of adults over 40 found that Hispanic males and females had a higher rate than other ethnicities.
According to the American Academy of Sleep Medicine, about 40 percent of adult men and 24 percent of adult women are habitual snorers.
Symptoms
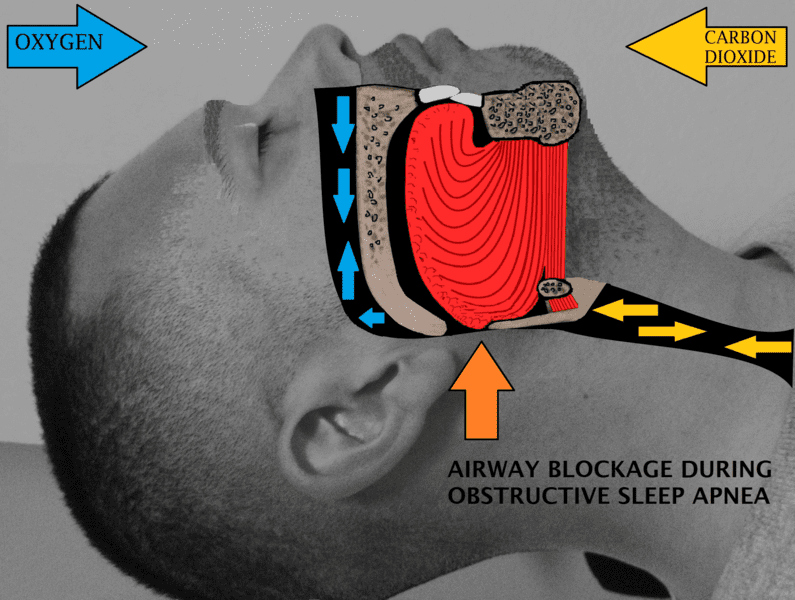
The main symptom of snoring is the harsh noise a person’s airway creates when they sleep. If the condition is occasional, it may be nothing to worry about. However, additional symptoms may indicate a serious sleep disorder called obstructive sleep apnea (OSA).
The condition causes a person to stop breathing repeatedly throughout the night, resulting in loud snoring and daytime tiredness. If left untreated, OSA can cause high blood pressure, stroke, and other heart problems. A major risk factor, 60 to 70 percent of individuals with this condition have high body fat issues.
In most cases, the affected person remains asleep and the affected person’s partner recognizes the symptoms of OSA. These symptoms include:
- Snoring
- Sleep problems that cause daytime sleepiness or fatigue
- Decreased sleep quality or insomnia
- Sudden awakenings with a sensation of gasping or choking
- Dry mouth or sore throat muscles upon awakening
- Cognitive impairment, such as trouble concentrating, forgetfulness or irritability
- Mood disturbances (depression or anxiety)
- Night sweats
- Frequent nighttime urination
- Sexual dysfunction
- Headaches
Causes
Snoring occurs when air is restricted while you sleep. In some cases, the throat and tongue muscles become too relaxed and block the airway. Although it can occur to anyone, including children and adults, it is most common in obese males over 40. The Sleep Foundation notes most of the common causes for the condition.
Not everyone who snores has OSA, but most people with OSA snore. This is a serious sleeping disorder that requires a diagnosis and treatment. Heart complications can occur if left untreated.
Lifestyle
Lifestyle also leads to the condition in many individuals without a serious condition. Alcohol and other sedatives cause the condition by relaxing the muscles that support tissue in the airway. Smoking is also considered a risk factor in snoring due to inflammation impacting the upper respiratory system. Obesity is also one of the most common lifestyle factors that can contribute to your snoring due to excess tissue near the neck which decreases airway size.
Sleeping on your back can increase the condition as the effect of gravity is to narrow the airway by pulling the tissues downward. Some have found sleeping on their side instead reduces the condition.
Biology
Biologically, head, neck, and mouth anatomy may lead to increased snoring. People are more likely to snore if they have a deviated septum (when the wall between the nostrils deviates). Growths in the nasal passages called polyps, having a small jaw, and having an enlarged tongue or tonsils may lead to an increased risk of snoring.
Nasal congestion, caused by allergies, infection or a dry environment, can also increase the risk. These effects can be temporary or can become chronic if the person is exposed to them long enough.
Finally, aging has been associated with increased instances of snoring. Researchers still investigating this correlation but it is most likely the result of weakened muscles around the airways as we age.
Diagnosis
As severe and frequent bouts of the condition may be a sign of a serious health problem, your health care professional will generally ask for a medical history and may ask your partner about snoring patterns. There are also certain tests that can determine if it is being caused by another condition.
Imaging: An x-ray, CT scan, or MRI can assess the structure of your airway to check for problems such as a deviated septum.
Sleep study: For severe cases, patients may be asked to undergo a sleep study in which their breathing is monitored while they sleep. These studies, called polysomnography, are usually performed in a sleep center overnight. During this time, you are connected to various sensors and observed for the following measurements:
- Brain waves
- Blood oxygen level
- Heart rate
- Breathing rate
- Sleep stages
- Eye and leg movements

Patients can perform some sleep studies from home. These modified studies record fewer body functions than at a sleep center but can usually be used to confirm a diagnosis from the comfort of your home. These studies measure airflow, breathing effort, blood oxygen levels and snoring. Doctors do not recommend a home sleep study for those with other sleep disorders such as central sleep apnea, restless legs syndrome, insomnia, or narcolepsy.
Treatment
When not associated with a medical condition, your doctor will most likely recommend lifestyle changes to help you stop snoring. These include options such as losing weight, avoiding alcohol consumption close to bedtime, treating congestion with medications or nasal strips, avoiding sleep deprivation, and changing your sleep position.
For OSA patients, one or more of several options are available as treatments for snoring.
Oral appliances
These are form-fitting dental mouthpieces that adjust the position of your jaw, tongue, and soft palate in a way that keeps the airway open. You will work with a dental specialist and a sleep specialist to ensure that the appliance fits correctly and is working. Patients wearing these devices may experience excessive salivation, dry mouth, jaw pain and facial discomfort.
Continuous positive airway pressure (CPAP) machine
This device is a mask that fits over your nose and mouth while you sleep. The mask directs pressurized air from a small pump into your airway to keep it open during sleep. This is the most common and most effective approach to treat snoring for people with OSA. Some people may have trouble getting used to the discomfort or noise, especially when first using it.

Upper airway surgery
There are several surgical procedures to modify the upper airway to allow breathing to resume normally during sleep. Examples include trimming excess tissue from your throat and moving the upper and lower jaws forward. With these options comes the normal risks for surgeries and the effectiveness is often difficult to predict.
If you liked this article, you should check out our other posts in the Nebula Research Library!
July 18, 2023
