Table of contents
Nebula Genomics DNA Report for Osteoarthritis
Is osteoarthritis genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!
What is Osteoarthritis?
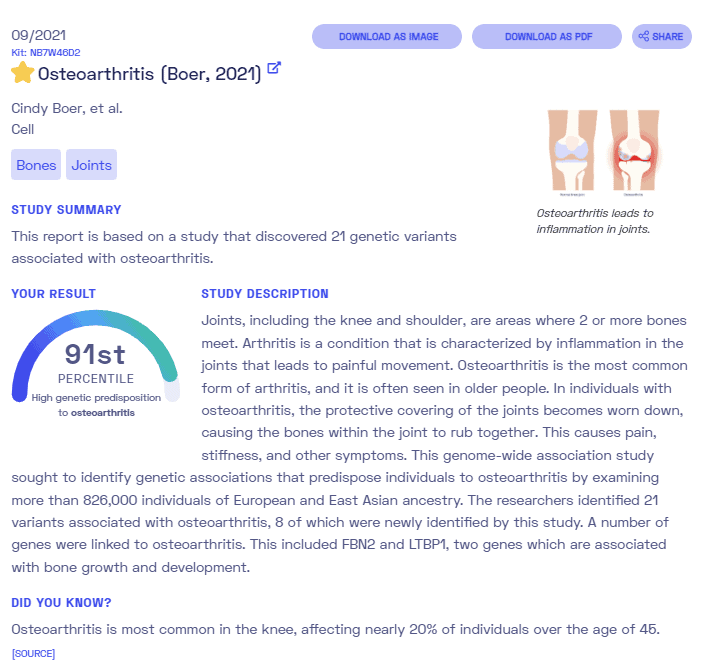
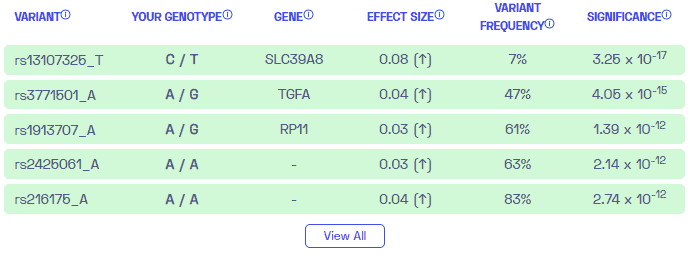
Osteoarthritis (OA) is a degenerative joint disease resulting from the breakdown of bone and cartilage as well as other connective tissue in those areas. Cartilage is the tough and flexible tissue that covers the ends of bones at the joints and allows for smooth movement. It is the most common type of arthritis and tends to occur as people age.
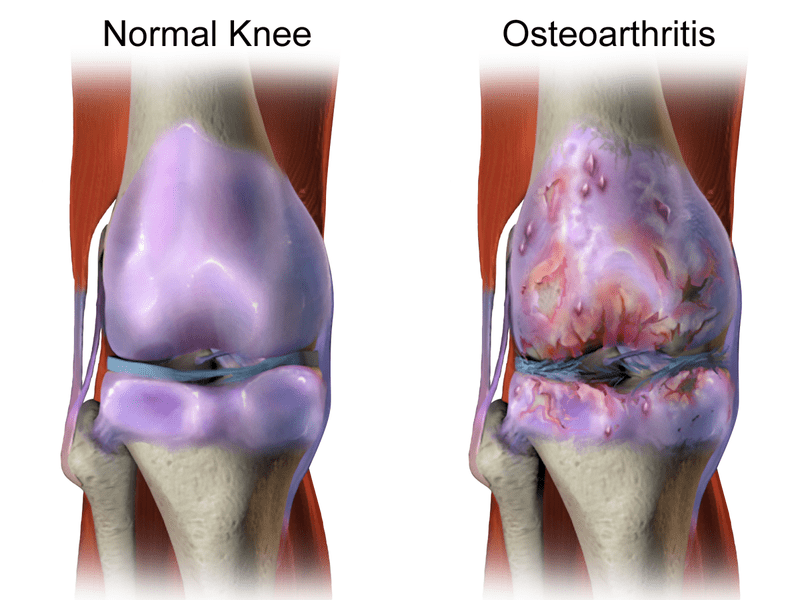
The first signs of the condition are joint pain and stiffness, which tend to occur gradually over time. Other symptoms affect the joints including swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. Joints involved are usually those in the fingers and thumbs, as well as weight bearing joints such as the hips, knees, neck, and lower back.
Unlike other types of arthritis, only the condition only affects the joints and not other parts of the body like systemic immune disease.
Forms
There are two types of osteoarthritis:
Primary osteoarthritis- generalized occurrence, usually in the fingers, thumbs, spine, hip joints, knees, and the great (big) toes.
Secondary osteoarthritis – Occurs with a pre-existing joint abnormality, including joint injury or trauma, such as repetitive or sports-related; inflammatory arthritis, such as rheumatoid, psoriatic, or gout; infectious arthritis; genetic joint disorders; congenital joint disorders; or metabolic joint disorders.
The cause of the condition tends to be injury, development, or genetic factors. It is also known as “wear and tear” arthritis since it tends to correspond to the amount of use in the joints. Abnormal stress on the joints is one of the main contributing factors. Thus, those with physically-demanding jobs tend to have a higher risk of developing the condition.
Doctors make a diagnosis based on signs and symptoms as well as medical imaging. Unlike rheumatoid arthritis, osteoarthritis patients do not experience hot or red joints, making this condition more difficult to diagnose.
To treat osteoarthritis, lifestyle factors such as exercise and using a support such as a cane are often recommended. Weight loss for those who are obese may also help alleviate symptoms. A healthcare professional may also prescribe pain medications if the condition is severe. In the worst cases, joint replacement surgery may be an option if other treatments are not successful.
Is Osteoarthritis Genetic?
People inherit an increased risk of developing osteoarthritis, not the condition itself. Most of the genetic components that increase osteoarthritis susceptibility are those that affect cartilage and bone. It is most likely the combination of many genes.
These gene variants include VDR, AGC1, IGF-1, ER alpha, TGF beta, CRTM (cartilage matrix protein), CRTL (cartilage link protein), and collagen II, IX, and XI. Most of these identified genetic variants for osteoarthritis are the result of genome wide association studies.
Individuals who are born with other bone diseases or genetic traits may be at higher risk to develop the disease. Ehlers-Danlos, which is characterized by joint laxity or hypermobility, can contribute to OA.

Epidemiology
Osteoarthritis is the most common form of arthritis, with 240 million cases worldwide. According to the Centers for Disease Control and Prevention (CDC), the condition affects 32.5 million US adults. Because it results from the amount of use on joints, it tends to affect people who are older, with 43% of patients aged 65 or older and 88% of patients aged 45 and older. Non-Hispanic white women are more likely than males or any other ethnic group to develop the condition.
Symptoms
The symptoms of osteoarthritis usually develop slowly and get worse the course of multiple years. During progression, the extracellular matrix around cartilage is actively remodeled.
At first, it may only affect a few joints. The most common areas to experience the condition are the knees, hips and small joints in the hands. The common symptoms of osteoarthritis include:
- Localized pain when using the joint, which may get better with rest. For some people with osteoarthritis, in the later stages of the disease, the pain may be worse in the evening after movement throughout the day
- Increased pain or stiffness, usually lasting less than 30 minutes, in the morning or after sitting for a period of time
- Swelling in and around the joint, especially after you use the area a lot
- Abnormal growth of the bone, visible as enlarged joints
- Limited range of motion in the joints
- Feeling that the joint is loose or unstable
- Weakness or muscle wasting
OA symptoms can range from mild to severe. Over time, the symptoms may get worse and interfere with work or daily tasks, affecting quality of life. Activities such as stepping up, getting up from the sitting position, and walking can become more difficult or even impossible.
Some patients experience episodes, when the symptoms get worse after certain activity or during certain weather patterns.
Causes
Age is the most important risk factor for osteoarthritis as the cartilage wears and tends to thin naturally with age. It occurs when use of joint tissues or injury causes the breakdown of cartilage and bone and deterioration of tendons and ligaments, which results in the pain and swelling associated with the condition.
Further damage in the form of inflammation is caused as the immune system responds to the injury and attempts to repair the damage. However, not all older people develop osteoarthritis and for those who do, not everyone experiences symptoms.
According to the UT Southwestern Medical Center, several risk factors put patients at greater risk. Inflammatory arthritis and injury/trauma are two of the most common risk factors, especially in those who are diagnosed at a younger age. Environmental factors that encourage obesity (especially associated with arthritis in the knee), diabetes, and high cholesterol also play a role.
Women may be particularly at risk due to the drop of estrogen that occurs after menopause.
Diagnosis
A health care professional will normally start by taking a medical history and gathering health information to assess if there is potential injury or trauma to the area. While there is no test for osteoarthritis, a physical exam can help doctors check for tenderness, swelling, redness and flexibility in the suspected joints. They may also recommend imaging or lab tests that can diagnose or rule out other conditions.
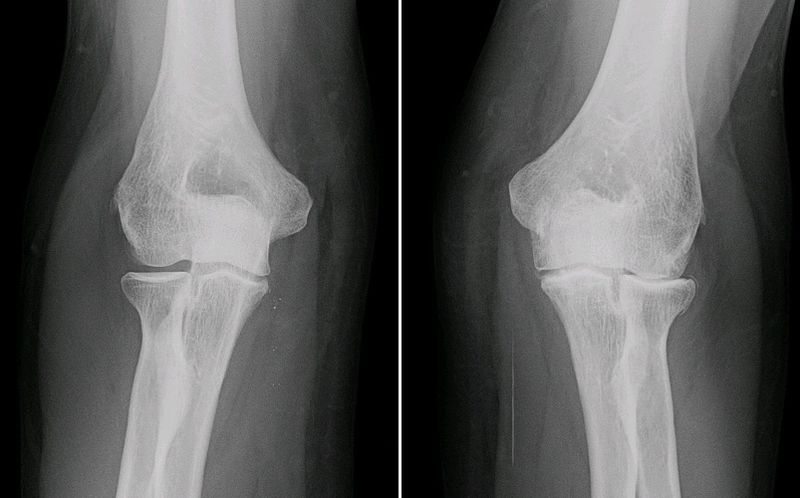
Imaging
X-rays and MRIs can capture pictures of the affected joints. If cartilage is missing, it will show up as narrowed space between the bone and joint. X-rays can also show bone spurs. MRIs are less common in diagnosing osteoarthritis but can help get a bigger picture in complex cases.
Lab tests
Blood tests can help rule out other conditions that may be causing the symptoms, including rheumatoid arthritis. Doctors may perform a joint fluid analysis by using a needle to draw fluid from the affected joint. They can test the fluid for inflammation, which can suggest other conditions such as gout or an infection.
Treatment
There is no cure for osteoarthritis. However, treatment can help reduce pain and disability, which can help patients improve their quality of life. Lifestyle factors, such as losing weight and moderate physical activity, can greatly improve symptoms. The Mayo Foundation for Medical Education and Research describes some of the treatments.
Medications
Most medications used to treat the condition are over the counter pain relievers although your doctor may recommend certain prescriptions.
Acetaminophen: These include oral medications such as Tylenol and are recommended for patients with mild to moderate pain. Taking more than the recommended dose of acetaminophen can cause liver damage.
Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). They are normally effective for all levels of severity although stronger NSAIDs are available by prescription. Some side effects include stomach upset, cardiovascular problems, bleeding problems, and liver and kidney damage.
Another option is gel-based NSAIDS, which patients apply to the skin over the affected joint. These tend to have fewer side effects and are just as effective.
Duloxetine (Cymbalta): Normally used as an antidepressant, this medication is also approved to treat chronic pain.
Therapy
There are several types of therapy available to treat pain. Physical therapy takes advantage of exercises that strengthen the muscles around affected joints, increase flexibility, and reduce pain.
Mild exercises like swimming or walking may also be effective. Occupational therapy can provide patients with alternative ways to engage with everyday activities to reduce the stress on their joints. Finally, transcutaneous electrical nerve stimulation (TENS) is a type of low-voltage electrical current treatment that temporarily relieves severe pain.
Surgery and other procedures
When other treatments are not effective, a doctor may recommend surgery to repair the joints and bones.
Cortisone injections: This procedure involves injecting cortisone directly into the affected joint. It helps reduce pain for a few weeks. Doctors usually limit the injections to three to four a year as too much of the medication can make joint damage worse.
Lubrication injections: Doctors normally make these injections in the knee, with the intention to create additional cushioning in that area.
Bone realignment: This procedure is usually performed on the knee in extreme cases. A surgeon will cut above or below the knee and either remove or add a wedge of bone. This procedure will shift body weight to a less affected area of the knee.
Joint replacement: In this procedure, an orthopedic surgeon will remove damaged joint surfaces and replace them with plastic or metal substitutes. As with any surgery, infections and blood clots may occur. A risk of joint surgery is that artificial joints can wear out or come loose and might eventually need to be replaced.
If you liked this article, you should check out our other posts in the Nebula Research Library!
May 3, 2023
