Table of contents
Nebula Genomics DNA Report for High Cholesterol
Is high cholesterol genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is High Cholesterol?
Cholesterol is a fat-like natural substance produced in the liver and found in all animal cells. It is an important component of healthy cell membrane formation and contributes to the stabilization of cell membranes, nerve function, vitamin D, the production of sex hormones, and other processes. The two types of lipoproteins, low-density lipoprotein (LDL) or high-density lipoprotein (HDL), carry it through the body.
High cholesterol levels often lead to coronary heart disease, the No. 1 killer of all patients in the United States. Healthy lifestyle factors, such as diet and exercise, and reduction of smoking and alcohol are the most effective ways to reduce or prevent high cholesterol levels.
Did you know you can measure your cholesterol levels at home? Read more about home cholesterol tests on our blog.
LDL
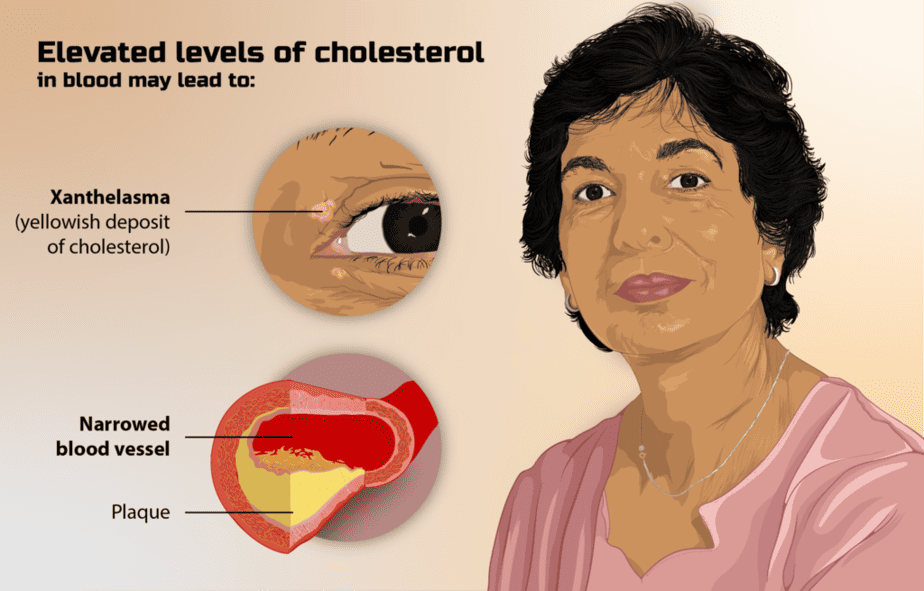
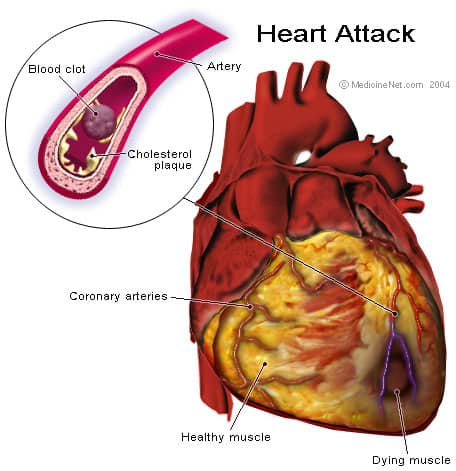
LDL (“bad” cholesterol) causes fatty buildup in the arteries, causing the blood vessels to narrow. This buildup makes it difficult for enough blood to flow through the arteries. Plaques of fat can also break off and form a clot that can cause a heart attack or stroke. High levels of LDL are a risk factor for the risk for many kinds of heart diseases.
Eating foods high in fat increases the level of LDL in the blood.
HDL
Experts widely refer to HDL (high-density lipoprotein) as “good” cholesterol. More of this type of cholesterol can actually help protect against heart attack and stroke. HDL carries LDL away from the arteries and back into the liver, where it is broken down and flushed out of the body.
However, HDL, or good cholesterol, can only do so much and cannot carry all the LDL away, especially if it is high. Therefore, it is important to also reduce LDL by eating more low-fat foods.
Triglycerides
This type of fat stores excess energy from food. A high triglyceride level combined with high LDL or low HDL is linked with fatty buildup in arteries. Cholesterol, triglycerides, heart attack, and stroke often affect the same body systems.
Is High Cholesterol Genetic?
There is a genetic condition that causes high cholesterol called familial hypercholesterolemia (FH). The frequency in the general population is about 1 in 400.
What is hypercholesterolemia? People with FH begin building up cholesterol in their arteries at a young age. Thus, they are at a higher risk of heart attack and stroke at an earlier age. Adults with this condition tend to have levels of 300 mg/dL or higher.
Is high cholesterol hereditary? Experts have found that it is more frequent in those of French Canadian, Ashkenazi Jewish, Lebanese, or Afrikaner (a South African ethnic group) descent. More than 90% of people with familial hypercholesterolemia are not diagnosed. This tends to be because the only clue to inherited high cholesterol is looking at family history to determine if multiple people have experienced heart disease at an early age (under 55 for males and under 65 for females).
Can high cholesterol be genetic? Genetic mutations in one of four genes, LDLR, LDLRAP1, APOB, or PCSK9, cause FH with the most frequent cause due to mutations found on the LDLR gene. Mutations in these genes affect the production of proteins needed for the LDL receptor to function properly. The liver continues to make more, thinking there is not enough from the bloodstream.
If you inherited FH from one parent, there’s a 50% chance you’ll pass it on to your children. If both of your parents passed the FH trait to you, your there is a 100% chance your children will also have it. Genetic testing can help you assess your risk of high cholesterol.
Current Research on High Cholesterol
The studies of genetic high cholesterol mainly focus on familial hypercholesterolemia genetics and its effect on patients from an early age. This 2017 review collected information from many reports to obtain how common heterozygous familial hypercholesterolemia is and how it confers risk for premature cardiovascular disease (CVD).
Last year, the American Heart Association published an article in their journal Circulation about the prevalence of familial hypercholesterolemia and patients with atherosclerotic cardiovascular disease.
For treatment, the FDA recently approved an add-on therapy called Evekeeza (evinacumab-dgnb) to treat patients with homozygous familial hypercholesterolemia (HoFH). Doctors can administer this injection to patients aged 12 and older.
Besides drugs and medication, researchers are also looking to apply nanotechnology to diagnose and treat high cholesterol. Some approaches, reviewed in this 2017 study, have proven safe and effective, while others are still in development.
Epidemiology
Doctors define high cholesterol levels as having a total level above 240 mg/dL. According to the Centers for Disease Control and Prevention (CDC), more than 12% of adults age 20+ had total cholesterol higher than 240 mg/dL, and more than 18% had high-density lipoprotein (HDL, or “good”) levels less than 40 mg/dL. Only 55%, or 43 million, adults in the United States who could benefit from cholesterol medicine are currently taking it.
According to the World Health Organization, about 2.6 million deaths occur worldwide from high cholesterol.
High blood cholesterol levels raise the risk of developing heart disease, the leading cause of death, and stroke, the fifth leading cause of death.
According to the 2015-2016 data, there was no significant difference in the prevalence of high cholesterol between various ethnic groups or between men and women.
Symptoms
Many patients do not realize they have high cholesterol levels since the condition doesn’t cause symptoms. Sometimes, only a major event, such as a heart attack or stroke, provides evidence. Unlike cholesterol levels, symptoms of heart disease and stroke are usually recognizable.
A heart attack occurs when a blood clot blocks the flow of blood to the heart. These clots form around arterial plaque when it breaks off into the bloodstream. Signs of an early heart attack include tightness, squeezing, fullness, pain, or aching in the chest or arms, difficulty breathing, anxiety, dizziness, nausea, indigestion, or heartburn, and excessive fatigue. A heart attack is a medical emergency as damage may be irreversible or fatal within hours.
A stroke is caused when the blood supply to the brain is cut off. Symptoms may only occur on one side of the body and include sudden loss of balance and coordination, sudden dizziness, facial asymmetry, inability to move, confusion, slurring words, numbness in the face, arm, or leg, vision problems, and sudden severe headache.
Like a heart attack, a stroke is a medical emergency that needs immediate medical treatment.
Elevated cholesterol may cause issues like Achilles tendonitis, when the Achilles tendon becomes inflamed and irritated.
Causes
Both lifestyle choices and genetic factors can cause high cholesterol. While the condition normally affects patients with one or more risk factors for heart disease, others may have a family history of high cholesterol that increases their risk.
There are several common risk factors:
- Family history
- Having high blood pressure
- Being overweight or obese
- Smoking
- Lack of exercise
- Age
- Diabetes
Diagnosis
A simple blood test is the only way to diagnose high cholesterol levels. These tests require either a blood draw or a dried blood sample. The most common diagnostic test is a lipid panel that measures total cholesterol, LDL, HDL, and triglycerides. According to the CDC, desirable levels of the testing components are:
- Total cholesterol less than 200 mg/dL
- LDL cholesterol less than 100 mg/dL
- HDL cholesterol 60 mg/dL or higher
- Triglycerides less than 150 mg/dL
Doctors consider total cholesterol between 200 and 239 “borderline” while they classify values over 240 mg/dL as high. Most people start getting cholesterol checks at age 20 and then rechecked every 4 to 6 years.
If you are at risk for heart disease or have a family history of the condition, recommended values might be adjusted to take that risk into effect. For example, it is generally recommended that people with heart disease or diabetes keep their LDL below 70 mg/dL.
Additionally, the values may be different for males and females. For example, having an HDL of 60 mg/dL is best for all patients. However, 40-59 mg/dL is considered borderline for females while 50-59 mg/dL is considered borderline for males.
While traditionally performed in a doctor’s office, at-home cholesterol tests are becoming more widely available. If you are interested in checking your cholesterol entirely from home, you should check out these testing companies:
EverlyWell (wide range of health and wellness tests)
InsideTracker (biomarker health tests and optional DNA test)
LetsGetChecked (wide range of health and wellness tests)
Treatment
Usually, the first treatment option involves lifestyle factors such as exercising regularly, eating a healthy diet, avoiding saturated fat and trans fats, and not smoking. These approaches can also be used to reduce your risk if you have a family history of the condition. When these aspects are not enough, your doctor may recommend medications to help keep levels in the optimal range. The prescribed type and combination of these medications is based on things like age, risk factors, and potential side effects.

Medications
Statins: Statins block a substance the liver uses to make cholesterol. When taking this medication, your liver tends to remove cholesterol from your blood. They can even prompt your body to reabsorb plaques that are already built up on the artery walls and help reverse cardiovascular disease.
Some common statins include atorvastatin (Lipitor), fluvastatin (Lescol XL), lovastatin (Altoprev), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor), and simvastatin (Zocor).
Some patients do not tolerate statins well. Common side effects are muscle pains and muscle damage, reversible memory loss and confusion, and high blood sugar.
Bile-acid-binding resins: The liver uses cholesterol to manufacture bile acids, which are needed for proper digestion. When this medication binds to the acids, the liver must use excess cholesterol to make more bile acids. Thus, less cholesterol is available to make it to the blood.
Some common examples are cholestyramine (Prevalite), colesevelam (Welchol), and colestipol (Colestid).
Cholesterol absorption inhibitors: This medication helps reduce blood cholesterol by limiting the small intestine’s absorption of dietary cholesterol. It can be used in combination with a statin drug.
Other options
Injectable medications: A newer class of drugs, known as PCSK9 inhibitors, can help the liver absorb more LDL. This lowers the amount of total cholesterol circulating in your blood. These medications may be useful for people who have a genetic condition that causes very high LDL cholesterol levels or in people who have an intolerance to statins or other cholesterol medications.
LDL apheresis: This non-surgical procedure removes LDL from a patient’s blood. It is ideal for those who can’t take other cholesterol medications. Although it’s not one of the first treatments, it may be recommended for patients with familial hypercholesterolemia, an LDL level greater than 200 mg/dL with coronary artery disease, or an LDL level greater than 300 mg/dL with or without known heart disease.
For more information on research and resources, you should visit the National Heart Lung and Blood Institute or the American Heart Association.
If you liked this article, you should check out our other posts in the Nebula Research Library!
May 19, 2023
