The Novel Coronavirus Disease (COVID-19)
For the past few months, the novel coronavirus (SARS-CoV-2 that causes the disease COVID-19), which emerged in December 2019 in Wuhan, China, has been making headlines as a rapidly evolving public health threat. To date, over 95,000 cases and 3,200 deaths have been reported in 85 countries and territories. Moreover, because of the growth of social media platforms, information about COVID-19, including travel restrictions and economic impacts, is spreading rapidly, perhaps even faster than the virus itself.
But how can a virus, which is not even alive, wreck so much havoc?
A Primer on Viruses
Viruses are microscopic organisms made up of proteins, fats, sugars, and genetic material that exist almost everywhere on the planet. However, on their own, viruses are not able to do anything. In order to survive, viruses need to infect living cells within hosts, such as bacteria, fungi, plants, or animals. Viral genetic material – DNA or RNA – contains information about how the virus can replicate, or make copies of itself. Once a virus infects a living cell, it hijacks the cell’s machinery to create a “virus factory.”
Human Immunodeficiency Virus (HIV)
In 1984, scientists at the Pasteur Institute of Paris the National Cancer Institute announced the discovery of HIV, a virus that infects the human immune system and can result in acquired immunodeficiency syndrome (AIDS). AIDS interferes with the body’s ability to fight infection and disease. HIV is transmitted through bodily fluids, and often, has been spread through unprotected sex, the sharing of needles, and through birth. Researchers suspect that HIV crossed over from chimpanzees to humans. This was likely due to butchering and consumption of monkey meat in the early 1900s.
Unfortunately, people living with HIV have faced a tremendous amount of discrimination. For example, early on, AIDS was mislabeled the “gay plague,” suggesting that it was spread exclusively among men who had sex with other men. However, American icons like basketball legend Magic Johnson and rockstar Freddie Mercury, both of whom announced that they were HIV-positive in the 1980s and 1990s, serve as reminders that viruses do not discriminate. Almost anyone can become infected.
Interestingly, in the case of HIV, there are some individuals who are resistant or immune to infection. These individuals harbor genetic mutations in the gene CCR5 that prevent their immune cells from displaying a receptor that allows HIV to enter cells and create “HIV factories.”
Coronaviruses
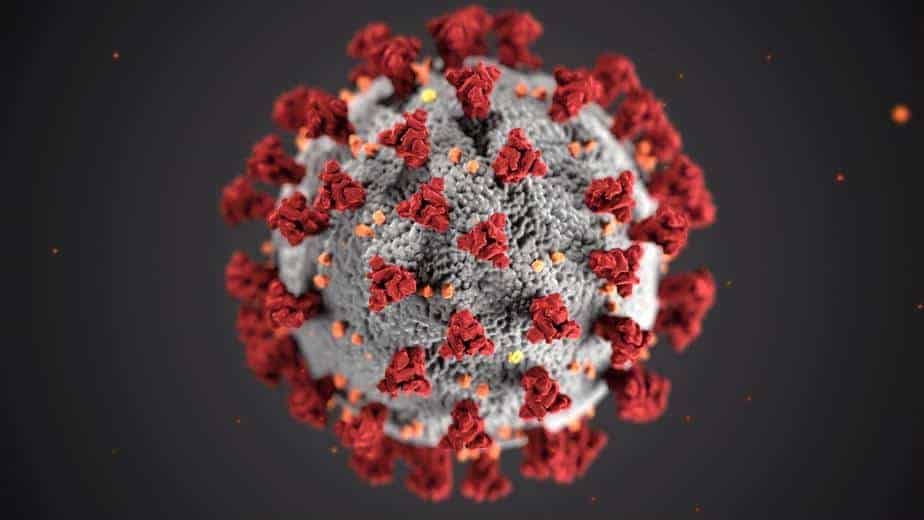
According to the World Health Organization, coronaviruses make up a large family of viruses named for the crown-like spikes found on their surfaces (Figure 1). They carry their genetic material in single strands of RNA and cause respiratory problems and fever. Like HIV, coronaviruses can be transmitted between animals and humans. Coronaviruses have been responsible for the Severe Acute Respiratory Syndrome (SARS) pandemic in the early 2000s and the Middle East Respiratory Syndrome (MERS) outbreak in South Korea in 2015. While the most recent coronavirus, SARS-CoV-2, has caused international concern, accessible and inexpensive sequencing is helping us understand the disease it causes, COVID-19, and respond to the outbreak quickly.
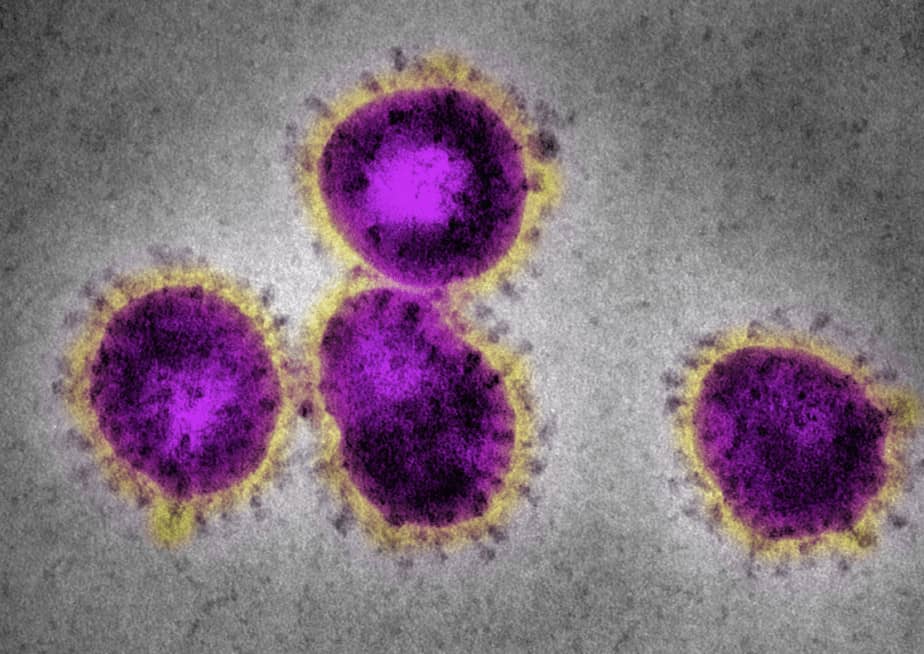
Figure 1. Coronaviruses with the characteristic spikes as seen under a microscope.
First studies that explore genetic susceptibility to COVID-19 are now being published. The first results indicate that SARS-CoV-2 infects cells using the ACE2 cell-surface receptor. Genetic variants in the ACE2 receptor gene are thus likely to influence how effectively SARS-CoV-2 can enter the cells in our bodies. Researchers hope to discover genetic variants that confer resistance to a SARS-CoV-2 infection, similar to how some variants in the CCR5 receptor gene make people immune to HIV. At Nebula Genomics, we are monitoring the latest COVID-19 research and will add any relevant discoveries to the Nebula Research Library in a timely manner.
The Role of Genomics in Responding to COVID-19
Scientists in China sequenced the genome of SARS-CoV-2 just a few weeks after the first case was reported in Wuhan. This stands in contrast to SARS, which was discovered in late 2002 but was not sequenced until April of 2003. It is through inexpensive genome-sequencing that many scientists across the globe are learning and sharing information about COVID-19, allowing us to track the evolution of the virus in real-time. Ultimately, sequencing can help remove the fear of the unknown and allow scientists and health professionals to prepare to combat the spread of COVID-19.
Next-generation DNA sequencing technology has enabled us to understand SARS-CoV-2 is ~30,000 bases long. Moreover, researchers in China determined that SARS-CoV-2 is also almost identical to a coronavirus found in bats and is very similar to SARS. These insights have been critical in aiding in the development of diagnostics and vaccines. For example, the Centers for Disease Control and Prevention developed a diagnostic test to detect SARS-CoV-2 RNA from nose or mouth swabs.
Moreover, a number of different government agencies and pharmaceutical companies are in the process of developing COVID-19 vaccines to stop the virus from infecting more people. To protect humans from infection inactivated virus particles or parts of the virus (e.g. viral proteins) can be injected into humans. The immune system will recognize the inactivated virus as foreign, priming the body to build immunity against possible future infection. Of note, Moderna, the National Institute of Allergy and Infectious Diseases, and the Coalition for Epidemic Preparedness Innovations identified a COVID-19 vaccine candidate in a record 42 days. This vaccine will be tested in human clinical trials starting in April.
For more information about COVID-19, please refer to the World Health Organization website. You can also find COVID-19 GWAS summary statistics here.
Interested in COVID-19 travel tests? Kurix Health offers special testing meeting requirements for departing and arriving in the UK.
You can also learn more about coronavirus tests in this blog post.