Osteoarthritis (OA), the most prevalent form of arthritis, affects a staggering 240 million individuals globally, with 32.5 million adults in the U.S. alone. This degenerative joint disease primarily afflicts older adults, with most cases found in patients aged 45 years and above.
OA occurs when bone and cartilage gradually degrade over time. Unlike other systemic variants of arthritis, OA is restricted to the joints. Experts commonly associate it with “wear and tear” on the joints. This suggests that individuals with careers or lifestyles involving heightened physical activity could be at a higher risk.
Moreover, inflammatory responses can exacerbate the damage, intensifying symptoms. Risk factors such as obesity, diabetes, and high cholesterol also play a role.
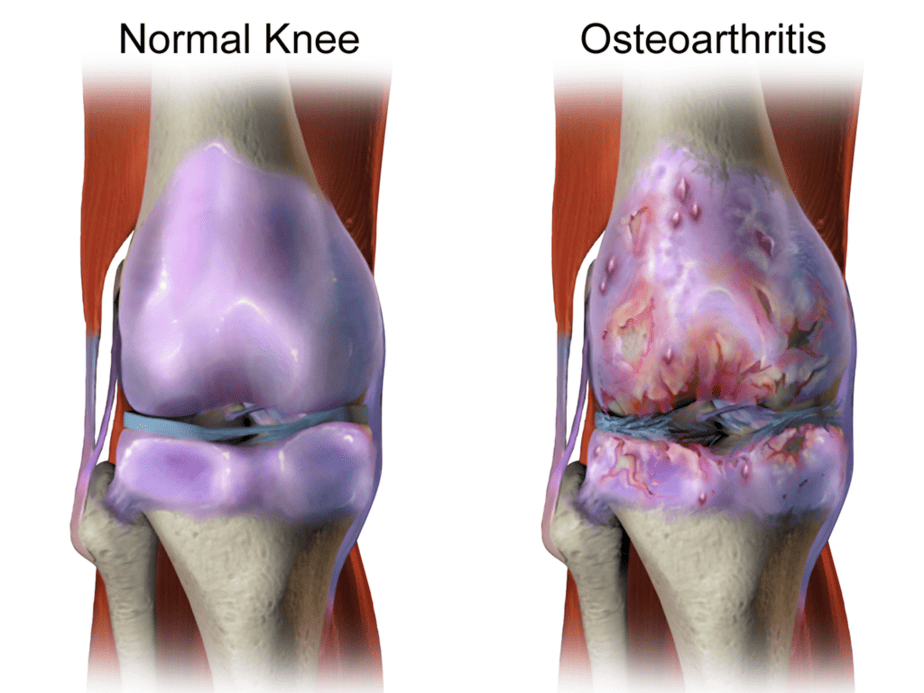
Patients typically notice OA in the knees, hips, and small joints of the hands, but it can progress to other areas over time. Initial symptoms include joint pain and stiffness. Later, it can also lead to joint swelling, reduced mobility, and muscle weakness.
| This post may interest those with a higher polygenic risk score for osteoarthritis. |
Since there’s no way to cure or slow OA’s progression, treatment focuses primarily on symptom management.
One potential contributor to the worsening of OA is systemic inflammation, which includes allergic reactions. A recently published paper in the Annals of Rheumatic Diseases delved into the possible association between OA and allergic conditions such as asthma and atopic dermatitis (eczema). In short, the researchers discovered that individuals with allergic diseases have a greater chance of developing OA. Their work lays the groundwork for potential OA treatments targeting the same biological pathways as allergy medication.
The Study
The researchers reviewed insurance claims data (2003-2019) and electronic health records (2010-2020). The substantial datasets contained over 1 million and 100,000 people, respectively.
The study identified the “exposed” group as patients diagnosed with either asthma or eczema and the “non-exposed” group as those with no such diagnosis. Both groups had a mean age of around 50, with the exposed group comprising 60% females, compared to 48% in the non-exposed group.
The analysis assessed which group had a higher risk of developing OA, gauged by a physician’s appointment coding.
Results
The data showed a 58% elevated risk of developing OA in the exposed group within the insurance claims dataset and a 42% increase within the electronic health records dataset.
Additionally, when the team conducted a statistical analysis to control for multiple variables such as age, gender, education level, etc., they found a 115% elevated risk of developing OA in those with asthma and eczema in the insurance claims dataset. Despite being less pronounced in electronic health records, the trend was consistent. The researchers suggest that this correlation supports the hypothesis that allergic pathways contribute to OA’s onset.

The study’s main limitation lies in its retrospective design, relying on previously collected data. Although the authors used statistical tools to minimize confounding variables, the authors concede that there might still be overlooked factors. Furthermore, the data could be skewed as other diseases might influence a patient’s frequency and reasons for doctor visits.
The team also highlighted the absence of information on BMI, joint trauma, or physical activity, potential variables, in the insurance claims dataset. Although the smaller electronic health records dataset attempted to account for these factors, the association became weaker when they included BMI.
Summary
In summary, the authors demonstrate that patients with atopic disease seem to have a greater risk of developing osteoarthritis than the general population. These results suggest that non-allergy patients may benefit from the same medication if the same biological pathways are responsible for both diseases. This result could impact OA treatment since current therapies only treat the symptoms, not the biological cause.
Citation
Baker MC, Sheth K, Lu R, Lu D, von Kaeppler EP, Bhat A, Felson DT, Robinson WH. Increased risk of osteoarthritis in patients with atopic disease. Ann Rheum Dis. 2023 Jun;82(6):866-872. doi: 10.1136/ard-2022-223640. Epub 2023 Mar 27. PMID: 36987654.
