Table of contents
Nebula Genomics DNA Report for Asthma
Is asthma genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of May 2021. |
What is Asthma?
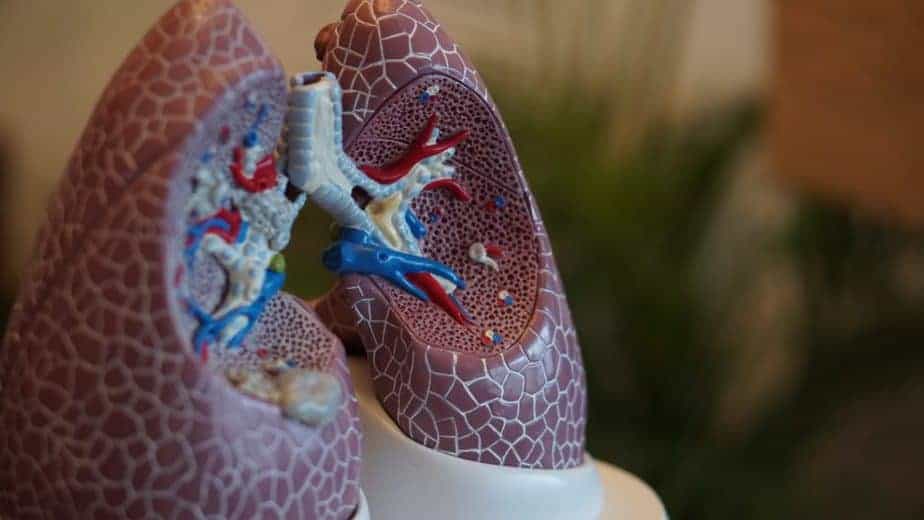
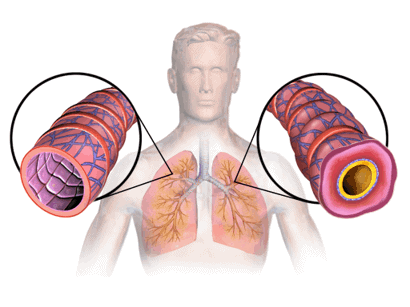
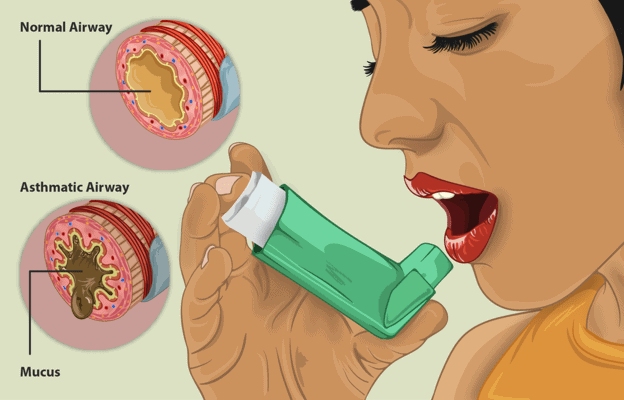
Asthma is a chronic, inflammatory disease of the airways with permanent hypersensitivity. In certain individuals, the inflammation may lead to the acute airway narrowing of bronchial obstruction. This airway narrowing is caused by increased secretion of mucus, spasm of the bronchial muscles, and formation of edema of the bronchial mucosa. A variety of stimuli causes an increase in airway sensitivity and associated inflammation, but the condition is reversible with treatment.
Did you know you can test inflammation markers at home? Learn more in our article about at home inflammation tests.
A distinction is made between allergic asthma (extrinsic) and non-allergic asthma (intrinsic). In pure form, however, these occur in only about ten percent of patients; mixed forms are observed in the majority. While the allergic form is more common in children, the non-allergic form is more frequent in old age.
Prenatal cigarette smoke exposure seems to promote it. There is also evidence that cultural and civilizational circumstances, as well as certain drug applications in early childhood, promote the condition.
Allergic
Allergies and asthma are often seen together. Allergic exogenous asthma is triggered by external stimuli (allergenic substances in the environment, so-called allergens) if there is a corresponding genetic predisposition to atopy (the genetic tendency to develop allergic diseases).
Type E immunoglobulins (IgE) are formed, which, in interaction with specific allergens, cause the release of allergy-triggering messenger substances such as histamine, leukotrienes, and bradykinins from mast cells. These substances then trigger airway constriction. A delayed reaction can occur after 6 to 12 hours, started by type G immunoglobulins (IgG). Often both reactions occur.
Non-allergic
Other stimuli can cause the non-allergic form: Infections, usually of the respiratory tract, drug intolerances, usually towards nonsteroidal anti-inflammatory drugs such as acetylsalicylic acid), drug side effects (e.g. of beta-receptor blockers and cholinesterase inhibitors), exposure to toxic or irritating substances, special physical exertion, and reflux disease are possible causes of this form. Some correlations and other causes are not yet clear.
Three characteristics of all cases include:
- Inflammation of the bronchial tubes: Allergens or other stimuli trigger an inflammatory reaction of the bronchial mucosa.
- Bronchial hyperreactivity: Hyperreactivity can often be felt when inhalation of irritant substances occurs, during exercise, or by cold air provocation. Substance P, a neuropeptide detected in the respiratory tract, is thought to be involved in the pathogenesis of bronchial hyperreactivity.
- Lack of bronchial clearing: Obstruction is the narrowing of the airway due to mucosal edema (fluid retention in the mucosa), increased or impaired mucus secretion, and bronchospasm. As a result, self-cleaning of the lungs is reduced. Secretions cannot drain and, in turn, increase damage to the point of obstruction, known as bronchial effusions.
Is Asthma Genetic?
In allergic asthma, it was observed that children of parents who both suffer from this condition have a 60-80% risk of developing the disease. According to a CDC report, if a person has a parent affected, they are three to six times more likely to develop the condition than someone who does not have a parent with asthma. This condition is a complex heritable disease, and it is believed that a combination of gene mutations contributes to the chances a person will develop it.
Current Research on Genetic Asthma
Is asthma a genetic disease? Scientists have conducted many studies to determine this. In 2018, the American Academy of Allergy Asthma and Immunology published a study that diversified studies into populations other than Europeans to help understand genetic discoveries across multiple groups.
A year before this, the same Academy published research on the extent of genetic causes of asthma, specifically the genetic variants that make patients susceptible to dust mite exposure.
The Frontiers in Pediatrics magazine published the Genomic Predictors of Asthma Phenotypes and Treatment Response in February 2019. This paper presents that even though the question “can asthma be genetic?” has been researched for over 40 years, questions remain as if we have discovered all the genetic markers for asthma.
The European Journal of Allergy and Clinical Immunology published a review of recent publications and studies related to diagnostic and treatment.
Atopic dermatitis is a skin condition that, when severe, 50% of patients develop the condition, as expressed in this study of the prevalence of the condition in patients with atopic dermatitis.
An interesting study revealed COVID-19-related genes in sputum cells in the condition. The objective of this research was “to determine demographic features and sputum ACE2 and TMPRSS2 gene expression.”
The pandemic triggered concerns about how the novel coronavirus (SAAR-CoV-2) would negatively affect asthma patients. The Asian Pacific Journal of Allergy and Immunology began research in May 2020 and concluded in July that same year. After extensive studies, they concluded that asthma does not increase COVID-19 mortality and poor outcomes.
Epidemiology
Many people with have some form of asthma at some point of their lives. According to the Centers for Disease Control and Prevention (CDC), 7.8% of all U.S. adults and 8% of U.S. children younger than 18 years had some form of the condition as of 2019. The condition is more common in boys under 18 than girls (8.4% and 5.5%) but more common in adult women (8.9%) than adult men (6.6%).
The condition is slightly more prevalent in Black and Hispanic than in other populations.
Symptoms of Asthma
Asthma symptoms vary in both frequency and severity among individuals:
- coughing or wheezing (whistling sound)
- chest tightness
- difficulty breathing
- shortness of breath
These symptoms are often similar to seasonal allergies (allergic rhinitis).
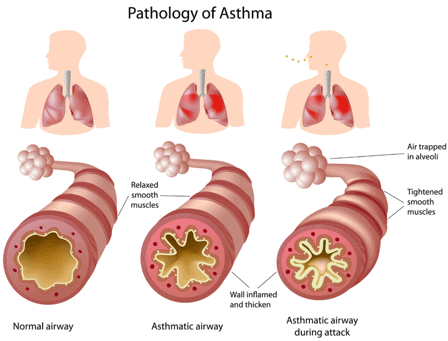
People with asthma may experience a short period of worsening symptoms called an asthma attack. In an attack, there is acute shortness of breath and constriction of the bronchial tubes. Exhalation, in particular, is difficult and is often accompanied by whistling breath sounds.
In some cases of asthma, coughing occurs in the form of coughing fits. Cough is usually the leading symptom in children. Difficulty breathing and shortness of breath can lead to anxiety, restlessness, difficulty speaking, and nausea.
Asthma Causes
Perhaps one of the first questions that come to mind is, “is asthma hereditary?”
Both genetic and environmental factors contribute. It tends to occur in individuals with a family history, proving that genetics play a role in causing the condition. But environmental factors may also play a key role.
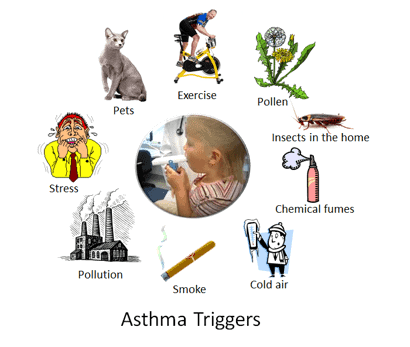
Environmental factors
Development of allergies (which also run in families) or respiratory infections tend to increase a person’s risk of developing asthma or making asthma worse. Additional risk factors for asthma include exposure to certain allergens or chemicals in the environment that may trigger the condition, including occupational asthma acquired through the workplace.
Environmental and health triggers that increase the risk of asthma include:
- Respiratory infections, including the cold or flu
- Irritants in the air
- Air pollution
- Tobacco smoke
- Exercise-induced asthma
- Cold air
- Medications, including beta-blockers and nonsteroidal anti-inflammatory drugs
- Stress
- Food and drink preservatives
- Allergic reactions, including dust mites, pet dander, and pollen
- Acid reflux
- Hay fever
Other diseases, such as Eosinophilic granulomatosis with polyangiitis, are associated with the immune system and play a role as precursors of the condition.
Diagnosis
Diagnosis is often easy to make with a history of the main symptoms.
According to Mayo Clinic, diagnosis is aided by lung function testing to test how much air moves in and out as you breathe.
A spirometry test measures the total volume of air inhaled and exhaled and the volume exhaled in one second during forced exhalation (a measurement of how fast you can exhale). The ratio of these two measurements is used to indicate airway constriction.
The PEF value (peak expiratory flow) is also used for diagnosis and therapy monitoring and is a measure of how hard you can breathe out. This value usually decreases even before an attack. It is measured with a “peak flow meter,” available in a variety of age-adapted designs.
These tests are often done before and after taking a medicament to open your airways called a bronchodilator. If your lung function improves with the use of a bronchodilator, you likely have the condition.
Other tests that help diagnose the condition are:
- Methacholine challenge: Methacholine is a well-known asthma trigger. When inhaled, it will cause your airways to narrow slightly. If you react to the methacholine, you likely have the condition.
- Imaging tests: A chest X-ray can help identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems.
- Allergy testing: Allergy tests can be in the form of a skin test or blood test.
- Nitric oxide test: When your airways are inflamed, your nitric oxide levels may have higher than normal. This test isn’t widely available.
- Sputum eosinophils: This test looks for specific white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing.
- Provocative testing for exercise and cold-induced asthma: In these tests, you perform vigorous physical activity or take several breaths of cold air. The doctor measures your airway obstruction before and after.
Determining the severity of a patient’s condition helps medical professionals recommend treatment. Severity is classified based on symptoms as mild intermittent (mild signs for up to two days a week and two nights a month), mild persistent (symptoms more than twice a week, but no more than once in a single day), moderate persistent (symptoms once a day and more than one night a week), or severe persistent (symptoms throughout the day on most days and frequently at night).
Asthma Treatment
In most cases, treating asthma usually comes as medicine in the form of either an asthma inhaler or a nebulizer, which delivers asthma medicine directly to the lungs. Other treatments are in pill form. The Asthma and Allergy Foundation of America provides health information and asthma action plans on their website.
Please note that this article is not intended to provide medical advice. You should speak to a medical profession to discuss your condition and treatment.
There are two types of inhalers for asthma management: metered-dose inhaler (MDI) and dry powder inhaler (DPI). MDIs deliver an aerosol while DPIs deliver dry powder.
A nebulizer converts liquid into a mist that you inhale through a tube. It is most often recommended for patients who have difficulty using inhalers.
Options for a long term treatment plan include:
- Inhaled corticosteroids to prevent and reduce airway swelling and reduce mucus in the lungs. They are the most effective long-term control medicines available.
- Inhaled long-acting beta-agonists open the airways by relaxing the smooth muscles around the airways.
- A combination of inhaled corticosteroids and inhaled long-acting beta-agonists
- Biologics (shots or infusions given every few weeks) target a cell or protein in your body to prevent airway inflammation. They can be costly treatments and are usually only prescribed when other treatments fail.
- Leukotriene modifiers are taken in liquid or as a pill to help relax the smooth muscle and reduce swelling.
- Cromolyn sodium is an inhaled non-steroid medicine. It keeps airways from swelling when coming into contact with a trigger.
- Theophylline comes as a syrup, capsule, tablet, and solution. This medicine helps relax the smooth muscle to open the airways.
- Oral corticosteroids are taken in pill or liquid form.
Quick-relief medicine is available when immediate relief is needed. These medicines act fast to relax tight muscles around your airways and allow the airways to open up.
- Short-acting beta agonists are inhaled and are the first choice for quick relief of symptoms.
- Long-acting muscarinic antagonists (LAMA) or anticholinergics are inhaled but have a slower action than the short-acting beta agonist medicines.
- A combination of short-acting beta agonists and long-acting muscarinic antagonists (LAMA).
This condition is chronic and thus it can be controllable but not curable. Treatment depends on the frequency and severity of the symptoms. Additionally, treatment may change if symptoms change. While medicine helps reduce symptoms, patients tend to get the best treatment when they both take medicine and avoid triggers.
If you liked this article, you should check out our other posts in the Nebula Research Library!
July 1, 2022