Nebula Genomics DNA Report for Restless Leg Syndrome
Is restless leg syndrome genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

Table of contents
What is Restless Leg Syndrome?
Restless leg syndrome (RLS), also called Willis-Ekbom Disease, is a long term neurological condition experts associate with the constant need to move one’s legs. At times, it affects the arms as well. Patients describe symptoms as aching, tingling, crawling, or other unpleasant sensations in the legs.
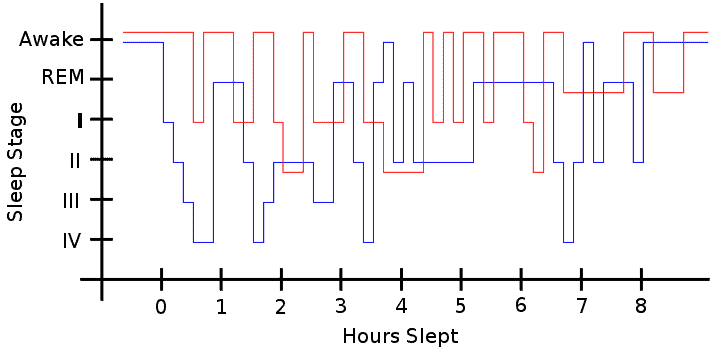
As these experiences are most common at rest, including while trying to sleep, the CDC classifies the condition as a sleep disorder. Notably, this factor can cause daytime sleepiness and insomnia. Limb twitching during sleep, a condition called periodic limb movement disorder, is also common.
Moving the legs will temporarily relieve the discomfort.

There are two types, mainly based on the onset of the condition. If it occurs before the middle age of 45, doctors call it early onset RLS. This form runs in families and can worsen over time.
When it occurs after the age of 45, it is known as late onset RLS. The latter form comes on suddenly and does not worsen.
Doctors diagnose restless leg syndrome by observing symptoms and ruling out other causes. They tend to associate it with other conditions and medications. Sometimes, the condition resolves on its own.
If there is an underlying problem, treatment of the cause will alleviate the RLS as well. Lifestyle changes and certain medications can also help with the condition.
Is Restless Leg Syndrome Genetic?
Restless leg syndrome is most likely a combination of genetic and environmental factors. Several genes have been associated with developing RLS. Most are thought to be involved in the development of nerve cells (neurons) before birth. Although not identified, genes associated with iron levels or dopamine signaling may also play a role.
Early onset RLS is more likely than the late onset form of restless leg syndrome to be genetic. Additionally, those with a family history of the condition are also at higher risk.
Epidemiology
The prevalence of RLS varies widely based on geographical location. There has historically been difficulty in obtaining accurate numbers due to the fact that many symptomatic patients do not seek treatment. Thus, researchers must carry out studies through one-on-one interviews or surveys.
In 2006, experts showed that RLS was a common disorder with prevalence rates ranging between 2.5 and 10% of the population. North American and European populations accounted for higher rates while Asian population values were lower. For example, a 2000 RLS study in the United States found a prevalence as high as 20% in adults.
In 2017, a collection of studies suggested that the prevalence rose to 3.9-15% of the general population. This includes 7-10% in Caucasians and 0.1 to 12% among Asian population. Higher rates appear in Western countries. In the United States, experts estimate the current rate at 5-10%.
Although it can occur at any point in life, risk and severity of the condition increases with age. Additionally, incidence is twice as common in women as men.
Symptoms
Symptoms of restless leg syndrome usually focus on physical sensations of the legs and behavioral changes. Patients often describe leg discomfort as creeping, itching, pulling, crawling, tugging, throbbing, burning, or gnawing.
Sitting, lying down, and overall little leg movement exacerbates these symptoms. Because of this discomfort, patients describe an uncontrollable need to move their legs. The effects of RLS include:
- Sleep disruption, including difficulty falling asleep and staying asleep
- Daytime sleepiness
- Struggles with behavior and work performance (irritability, moodiness, difficulty concentrating, hyperactivity, etc.)
Symptoms can be mild or severe. On the mild end, a person may experience symptoms only a few times a month. For others, they may be as persistent as every night. In the most severe cases, the symptoms can affect the arms or other parts of the body.
Causes
In most cases, the cause of restless leg syndrome is unknown. In most cases diagnosed before the age of 40, there appears to be a hereditary component.
Overall, doctors associate the symptoms with the the central nervous system, especially the basal ganglia, the part of the brain that controls movement. Low iron levels may be the main cause through disruption of the chemical dopamine, which can result in involuntary movement, such as that seen with this condition. Other movement disorders, such as diabetes, rheumatoid arthritis, and Parkinson’s disease, also increase the risk of developing restless leg syndrome.
A case control study published in 2023 discovered that the prevalence of RLS among multiple sclerosis (MS) patients was significantly higher than those without MS, suggesting a close association between the two conditions.
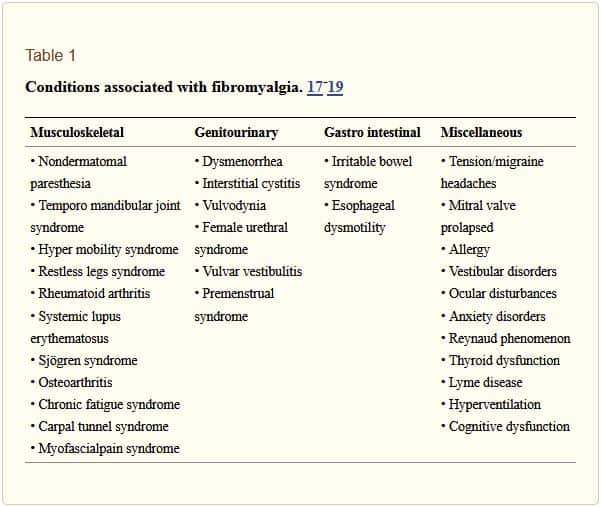
The National Institute of Neurological Disorders and Strokes lists the other conditions and medications that may contribute to developing the restless leg syndrome symptoms:
- Kidney failure and hemodialysis
- Iron deficiency (anemia)
- Use of alcohol, nicotine, and caffeine
- Pregnancy, especially in the last trimester
- Neuropathy (nerve damage)
- Anti nausea drugs
- Antipsychotic drugs
- Antidepressants that increase serotonin
- Some cold and allergy medications that contain older antihistamines (e.g., diphenhydramine)
Diagnosis
The diagnosis of restless leg syndrome is based on a patient’s medical history and expression of symptoms. The International Restless Legs Syndrome Study Group has a list of diagnostic criteria for clinical practice:
- A strong, often irresistible urge to move your legs, usually accompanied by uncomfortable sensations.
- Symptoms start or get worse when you’re resting, such as sitting or lying down.
- Symptoms are partially or temporarily relieved by activity, such as walking or stretching.
- Symptoms are worse at night.
- Symptoms can’t be explained solely by another medical or behavioral condition.
If your doctor suspects that an underlying medical condition is causing the symptoms, they may order a physical or neurological exam or blood tests for conditions such as anemia.
Depending on how severely the condition is affecting your sleep, the doctor may recommend you see a sleep specialist. This specialist can also use sleep studies to test for conditions such as sleep apnea.
Treatment
If an underlying condition causes RLS, treatment of that ailment will normally improve the symptoms. For example, if iron deficiency is detected, iron supplementation via oral or intravenous means may be recommended.
When a doctor detects no underlying condition, they may prescribe lifestyle changes and medications to improve sleep and quality of life. Mayo Clinic describes some of these approaches.
Lifestyle changes
Simple lifestyle changes can help alleviate the symptoms although they do not address the underlying cause of RLS itself.
- Warm baths and leg messages can help relax nervous muscles
- Warm and/or cold packs help relax muscle sensations
- Good sleep hygiene that includes a cool, quiet, comfortable sleeping environment; a consistent sleep schedule; and at least seven hours of sleep nightly
- Moderate, regular exercise
- Avoiding caffeine
- A foot wrap specifically for RLS that creates certain pressure points
Medications
Prescription medications may be recommended if the symptoms persist or are severe.
Medications that increase dopamine in the brain: These medications alter the levels of dopamine in the brain, which may biologically cause the symptoms. Several options are approved by the Food and Drug Administration (FDA) for RLS. Mild side effects include nausea, lightheadedness, and fatigue. Some people with RLS may also experience impulse control issues due to the change in brain chemistry associated with this medication.
Medications that affect calcium channels: These medications can also alter brain chemistry which affects symptoms.
Opioids: These narcotics are often effective to treat RLS symptoms ranging from mild to severe. They should be prescribed carefully as they can be addicting.
Muscle relaxants and sleep medications: These medications are used to help patients sleep better at night. They do not relieve the symptoms of RLS and can cause daytime drowsiness. Therefore, they are usually only recommended after other treatment options have failed.
Some medications, including some antidepressants, some antipsychotic medications, some anti-nausea drugs, and some cold and allergy medications, may make symptoms worse.
For more information, you may want to visit the website of the American Academy of Sleep Medicine.
Did you like this article? Be sure to check out the other posts in the Nebula Research Library!
July 5, 2023
