Table of contents
Nebula Genomics DNA Report for Type 2 Diabetes
Is type 2 diabetes genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of May 2021. |
What is Type 2 Diabetes?
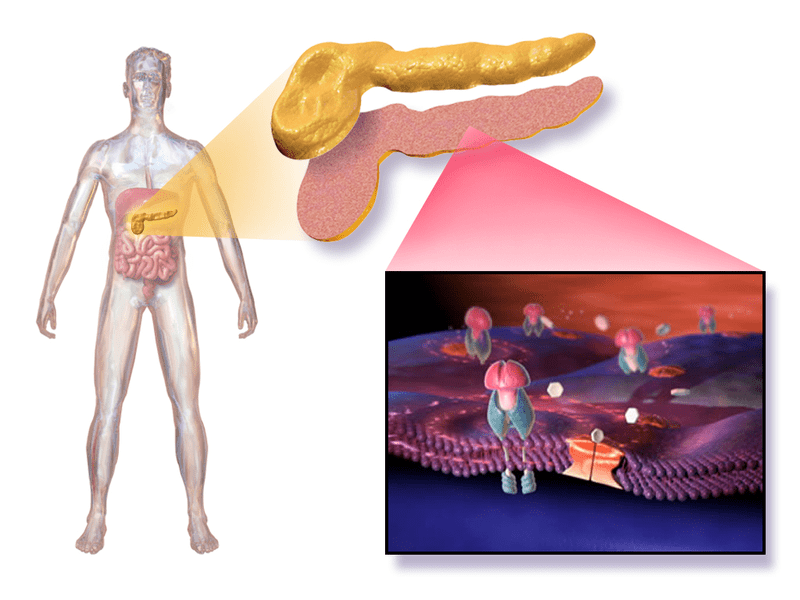
Type 2 diabetes is a disorder in which insulin is present but cannot act appropriately. This is commonly known as insulin resistance. In the early years of the disease, the pancreas can compensate by producing high levels of insulin. At some point, however, the pancreas can no longer maintain excessive insulin production. The amount of insulin produced is no longer sufficient to control blood glucose levels, and type 2 diabetes mellitus manifests.
This common form of diabetes usually develops in adults, although more and more children, teens, and young adults are being diagnosed.
Type 2 diabetes produces much more endogenous insulin than a metabolically healthy person (hyperinsulinism). Due to high insulin resistance, blood glucose still rises; later, via a relative deficiency, absolute insulin deficiency occurs in some cases. The selfish-brain theory provides a possible explanation of the complex regulation of blood glucose and lipid metabolism by the hypothalamus always to provide sufficient glucose to the brain.
Type 2 diabetes is often diagnosed late, not taken seriously, or inadequately treated, and physicians are sometimes uncertain about treatment. Patients, too, often tend to suppress it despite education and training since noticeable health limitations usually do not occur until acute, sometimes irreversible, damage manifests itself.
Is Type 2 Diabetes Genetic?
Children who have a single parent with type 2 diabetes have around a 40 percent chance of also having the disease. In comparison, children who have two parents with the disorder have a higher risk of about 80 percent to also develop the disorder as adults. In total, studies have identified at least 150 DNA variations associated with the genetic risk of developing type 2 diabetes. A combination of these genetic mutations is most likely necessary for a change in risk to be present as opposed to a single variant.
Mutations in any gene associated with mechanisms of controlling glucose levels and insulin processing have the risk of contributing to the risk of having diabetes. These factors include genes related to the development and function of beta cells in the pancreas, the release and processing of insulin, and cells’ sensitivity to the effects of insulin.
Some specific genes identified are:
- TCF7L2, which affects glucose production and insulin secretion
- ABCC8, which helps regulate insulin
- CAPN10, which is associated with type 2 diabetes risk in Mexican-Americans
- GLUT2, which helps transport glucose into the pancreas
- GCGR, a glucagon hormone involved in glucose regulation
Current Research on Type 2 Diabetes
In 2021, a study was published in the Journal of Personalized Medicine, titled “Impact of Genetic Factors on the Age of Onset for Type 2 Diabetes Mellitus in Addition to the Conventional Risk Factors.”
The study aim was to evaluate the joint effect of type 2 diabetes-associated single nucleotide polymorphisms (SNPs) and conventional risk factors for the condition (sex, body mass index (BMI), and TG/HDL-C ratio) with age of onset.
Results showed a considerable genetic factor contributing to the early onset of type 2 diabetes mellitus. According to the study, the results suggest that genetic risk factors can be used as a complementary tool for estimating the risk of the earlier onset of type 2 diabetes and help guide early interventions.
Another study titled “Effects of family history of diabetes on pancreatic β-cell function and diabetic ketoacidosis in newly diagnosed patients with type 2 diabetes: a cross-sectional study in China” was conducted to examine the association between a parental and/or sibling history of diabetes and clinical characteristics.
The result shows that patients with a parental history of diabetes were characterized by early-onset disease, poor glycemic control of fasting blood glucose, and a high prevalence of DKA.
It further revealed that the patients with a sibling history of diabetes had later disease onset and lower body mass index than those without that history. Hence, a family history of diabetes can increase an individual’s chance of having the disease.
Epidemiology
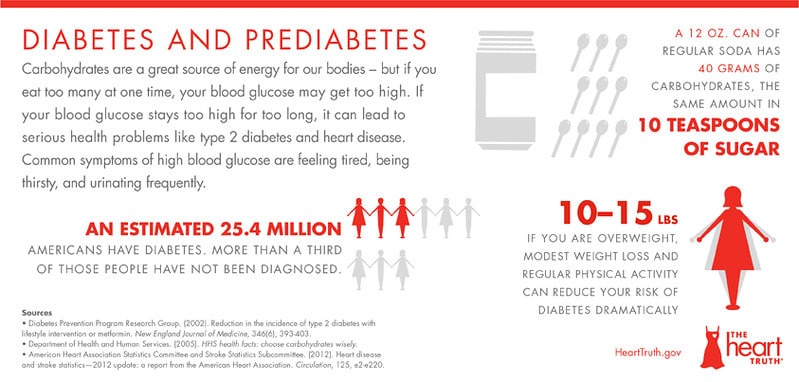
According to the Centers for Disease Control and Prevention (CDC), 34.2 million people (10.5% of the United States population) had diabetes in 2020. 21.4% of those people are undiagnosed. They also estimate that 88 million people aged 18 years or older (34.5% of the adult US population) and 24.2 million people aged 65 years or older have prediabetes.
According to a report in the journal of epidemiology and global health, titled “Epidemiology of type 2 diabetes–global burden of disease and forecasted trends,” In 2017, about 462 million people had type 2 diabetes corresponding to 6.28% of the world’s population (4.4% of those aged 15–49 years, 15% of those aged 50–69, and 22% of those aged 70+).
Symptoms of Type 2 Diabetes
The condition develops slowly. Many people with type 2 diabetes may not realize it for several years as the symptoms occur gradually. Type 1 and type 2 forms of the condition have many symptoms in common. However, in contrast to type 1 diabetes, type 2 is rarely associated with weight loss and only with massively elevated blood glucose levels with increased urination and thirst. Early symptoms may include fatigue, weakness, visual disturbances, and a tendency to infections (bacterial infections and fungal infections) such as frequent bladder infections.
According to Mayo Clinic, there are other symptoms of type 2 diabetes, including:
- Increased thirst
- Frequent urination
- Increased hunger
- Unintended weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
- Frequent infections
- Numbness or tingling in the hands or feet
- Areas of darkened skin, usually in the armpits and neck
Additionally, a rare symptom is hyperosmolar syndrome up to hyperosmolar coma can occur. This symptom appears when an extremely high blood glucose level causes the kidneys to excrete so much water that the loss of fluid can no longer be compensated for by drinking.
Comorbid disease
Potential complications arise in patients with type 2 diabetes, some of them serious. Diabetes is associated with conditions such as stroke, high blood pressure, increased risk of heart disease, and narrowing of blood vessels (atherosclerosis), nerve damage (neuropathy) in limbs, and other nerve damage. Nerve damage in the digestive system can cause health problems with nausea, vomiting, diarrhea, or constipation. For men, nerve damage may cause erectile dysfunction.
People with diabetes may experience kidney disease, eye damage such as cataracts and glaucoma, skin conditions including bacterial and fungal infections, slow healing, hearing impairment, sleep apnea, Alzheimer’s disease, and other disorders that cause dementia.
Causes
Two interrelated problems contribute to the onset of the disorder. Firstly, cells in muscle, fat, and liver become resistant to insulin, and secondly, the pancreas fails to supply enough insulin to control high blood sugar levels. A combination of genetic, environmental factors, and lifestyle factors contributes to an increased risk of developing the disease.
Obesity
Being overweight or obese is considered one of the leading causes of type 2 diabetes. In particular, excessive abdominal fat around internal organs such as the liver or pancreas, caused by fat- and sugar-heavy diet, is considered a risk factor for diabetic patients. In addition to congenital insulin insensitivity, obesity results in the additional insulin resistance of the insulin-dependent cells of the body.
When such a cell is stimulated with insulin in healthy individuals, more type 4 glucose transport proteins (GLUT-4) are inserted into the cell membrane. In type 2 diabetics, this mechanism, among others, is disturbed. In their muscle and adipose tissue, GLUT-4 is downregulated.
There is a correlation between the concentration of the messenger retinol-binding protein 4 (RBP-4) and the extent of insulin resistance. RBP-4 is produced in excessive amounts in the adipose tissue of overweight individuals. This messenger appears to cause muscle and liver cells to respond poorly to the blood glucose-regulating hormone insulin. If insulin resistance improves after physical training, lower RBP-4 plasma levels can also be measured.
Other factors
Correlation studies have suggested that other factors than genetics play a role in increasing the risk of acquiring the disorder:
- Fat distribution. Storing fat mainly in your abdomen — rather than your hips and thighs — indicates a greater risk.
- Inactivity. The less active you are, the greater your risk. Physical activity helps control your weight, uses up glucose as energy, and makes your cells more sensitive to insulin.
- Blood lipid levels. Increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol and high levels of triglycerides (you can get these levels measured at home!)
- People of certain races and ethnicities — including African American, Hispanic, Native American and Asian people, and Pacific Islanders — are more likely to develop diabetes type 2
- Age. The risk of type 2 diabetes increases as you get older, especially after age 45.
- History of prediabetes or gestational diabetes (developed during pregnancy)
- Women with a condition called polycystic ovary syndrome
Diagnosis
Most diabetes testing focuses on A1C measurements. A1C is measured through a blood test and informs doctors and patients of their average blood sugar level over two to three months. This measurement is useful not only in diagnosing the disease but also in monitoring it. A1C levels below 5.7% are considered normal, between 5.7%-6.5% are prediabetic levels, and anything over 6.5% indicates diabetes range.
Other tests used to assess blood sugar levels include the fasting plasma glucose test, which tests the amount of glucose in plasma, or the oral glucose tolerance test, which measures how your body responds to added glucose.
Some at-home testing kits may help diagnose the condition through easy-to-use measurements. Day Two is a gut microbiome test designed to help patients with Type 2 diabetes target their diet. Some lab testing companies like LetsGetChecked and Everlywell offer a finger prick test that measures A1C and other contributing factors, which can be done from your home without going to a doctor’s office. You can also do genetic testing to sequence your entire genome and see your genetic risk of developing the disease. The test will examine whether you have a combination of the genetic predispositions through whole-genome sequencing companies like Nebula Genomics!
Prevention
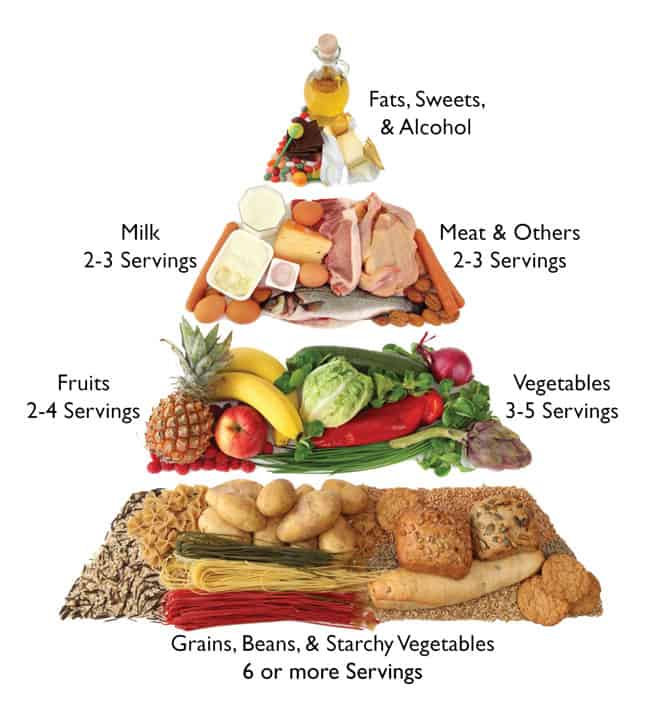
Diet, exercise, and losing weight are the key ways to prevent or delay the disease. You can proactively help to prevent type 2 diabetes, even if you have a family history of the disease. These prevention strategies are based on modified healthy lifestyle factors that help keep weight and blood sugar under control. Eating healthy foods low in fat and calories and high in fiber is one of the most critical factors. Staying active and losing excess body weight are also incredibly effective prevention strategies.
Treatment
In type 2 diabetes, increased insulin resistance can be reduced by healthy eating, weight loss, and increased exercise. The first options for managing diabetes usually include lifestyle changes that help the patient maintain healthy body weight. Many of these diabetes treatments are the same lifestyle factors as prevention, including eating foods high in fiber, increased aerobic activity, and eating regularly.
In most cases, lifestyle changes are enough to treat type 2 diabetes. Regular self-monitoring of blood glucose levels using different types of diabetic monitoring systems is an integral part of most diabetes care.

However, if the pancreas is not making enough insulin, health care teams will instruct patients to take insulin therapy, which involves insulin injections once to several times a day and/or other prescription medications.
Healthline describes some of the most common types of diabetes medicines:
- Metformin helps manage blood glucose levels and improves how your body responds to insulin
- Sulfonylureas (oral medications) help your body make more insulin
- Meglitinides quickly stimulate your pancreas to release more insulin
- Thiazolidinediones make your body more sensitive to insulin
- Dipeptidyl peptidase-4 inhibitors are milder medications that help reduce blood glucose levels
- Glucagon-like peptide-1 (GLP-1) receptor agonists slow digestion and improve blood glucose levels
- Sodium-glucose cotransporter-2 (SGLT2) inhibitors aid to prevent the kidneys from reabsorbing glucose into the blood and sending it out in urine
Since the condition is often associated with high blood pressure as part of the metabolic syndrome, and high blood pressure further accelerates late complications of diabetes, especially in the eyes, kidneys, and large blood vessels, high blood pressure must be detected and treated early.
Especially concerning macrovascular risks such as myocardial infarction or stroke, optimal blood pressure control is even more important than optimizing sugar metabolism. However, for the microvascular risks of the eyes and nerves, optimization of blood glucose is considered more important.
More resources and support are available from the American Diabetes Association or the National Institute of Diabetes and Digestive and Kidney Diseases, a part of the National Institutes of Health. These websites help you learn about your risk of diabetes and digestive and kidney diseases and provide resources.
You can find more diabetes reports on our website. If you liked this article, you should check out our other posts in the Nebula Research Library!
July 9, 2022
