Table of contents
Nebula Genomics DNA Report for Congestive Heart Failure
Is congestive heart failure genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of May 2021. |
What is Congestive Heart Failure?
Congestive heart failure (CHF), or simply heart failure, is the inability of the heart to pump enough blood to meet the body’s need for blood and oxygen. The “pump weakness” manifests itself in reduced physical and mental performance. Additionally, when the left side of the heart is weak, water accumulates in the lungs, which manifests itself as shortness of breath, especially when the patient is lying down. In severe cases, it limits oxygen uptake in a life-threatening manner.
Congestive heart failure is the common result of many cardiac diseases, with long-standing high blood pressure and atherosclerotic narrowing of the vessels supplying the heart (i.e., coronary heart disease and expired heart attacks) the most common causes. In therapy, in addition to the treatment and elimination of underlying conditions and risk factors, certain antihypertensive drugs play a significant role, as they have been shown to prolong survival.
Advanced heart failure often shows a relapsing course with recurrent decompensations, in which the affected person stores too much water and thus “overloads” their heart. Cardiac decompensation is a common reason for hospitalization. It can often be managed with diuretic medications and intensive care if necessary, but it can also lead to death from relative health. Heart failure is a common disease with high mortality and is one of the leading causes of death.
Is Congestive Heart Failure Genetic?
While congestive heart failure itself doesn’t appear to be genetic, the chances of developing risk factors such as high cholesterol and hypertension tend to run in families. There are also a number of other heart diseases related to congestive heart failure that have a genetic component. Three of the most commonly inherited heart diseases are familial hypertrophic cardiomyopathy, familial dilated cardiomyopathy, and familial hypercholesterolemia.
All of these diseases may lead to heart failure. Other factors that contribute to the risk of developing heart failure are hypertension, diabetes, high cholesterol, and coronary artery disease.
Is congestive heart failure hereditary? Most of the cases documented are not, but some inherited heart conditions are considered a risk factor and can run in families.
Did you know you can test for heart health at home? Learn more about home heart health tests and home cholesterol tests on our blog.
Current Research on Genetic Congestive Heart Failure
There are a number of heart conditions affecting an increasing number of patients every year. Undoubtedly, advanced research has helped with treatment. In 2019, the University of Southern California published a study on Innovation in Heart Failure Treatment: Life Expectancy, Disability, and Health Disparities.
Only around three years ago, the studies on heart failure were poorly understood. To better understand the molecular and cellular mechanisms in heart failure, scientists from two universities in Aurora, CO, and the University of Trieste, Italy, published positive insights to understand the disease in 2018 better. In February, several universities from the UK published a population-based study of 4 million individuals to observe and document temporal trends and patterns in heart failure incidence.
If you are interested in knowing more about how our knowledge and understanding of heart failure has changed through history, we recommend “The history of the evolution of knowledge about the diagnosis and the pathogenetic aspects of heart failure: From the Egyptians to James Mackenzie.” This article was published in the International Journal of Cardiology in 2020. You can also read about the natural history of the disease through The Framingham Study.
From the Framingham study, you can also check out this interesting article about the Role of diabetes in congestive heart failure.
The year 2021 brought us this exciting study on the impact of congestive heart failure and role of cardiac biomarkers in COVID-19 patients.
Classification
The types of heart failure are subdivided according to its course (acute or chronic), to the affected half of the heart (right or left, otherwise global), and to the mechanism.
Course
The two types of congestive heart failure based on course are acute heart failure and chronic heart failure.
Acute heart failure develops over the course of hours to days. Causes include:
- Tachycardia (heart rate too high) or bradycardia (heart rate too low)
- Sudden loss of pumping function due to a heart attack
- Pulmonary embolism
- Acute and severe inflammation of the heart muscle (Did you know you can test inflammation markers at home? Learn more in our article about at home inflammation tests).
- Mechanical obstruction of ventricular filling, e.g., due to pericardial tamponade
- Sudden valve insufficiency due to rupture of a pre-damaged heart valve
On the other hand, chronic heart failure develops over the course of months to years.
It is characterized by a faster irregular heartbeat, thickening of the heart muscle, constriction of blood vessels, increased blood volume, etc., which can compensate for the reduced pumping capacity of the heart. Compensated heart failure may show no symptoms or show symptoms only with physical exertion. In the decompensated stage, pathological water retention (edema) and shortness of breath (dyspnea) occur. This already happens at rest or under low exertion.
Affected half of heart
Heart failure often does not affect both halves of the heart equally. Left-side heart failure is characterized by blood backing up into the pulmonary vessels (often resulting in pulmonary hypertension) with coughing and shortness of breath, and even pulmonary edema. The impaired pumping capacity of the left ventricle also leads to decreased exercise capacity and eventually low blood pressure.
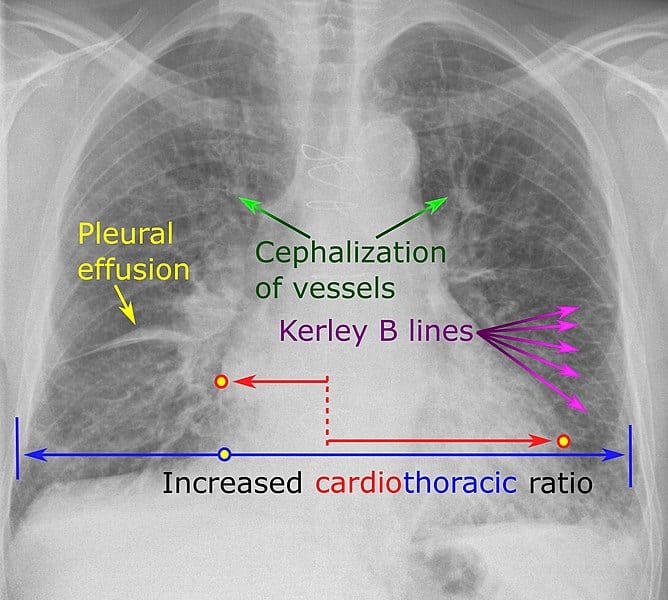
In right heart failure, the contraction failure of the right ventricle and right atrium, blood backs up into the body’s veins. The increased venous pressure can cause water retention in the tissues with edema, especially of the lower parts of the body (legs), as well as in the abdomen (ascites) and pleural cavity (pleural effusion).
Global heart failure with contraction insufficiency of the right and left ventricles shows both left and right heart failure symptoms.
Mechanism
Functionally, a distinction can be made between forward and reverse heart failure. In forward failure, adequate pressure cannot be built up in the arteries, whereas blood backs up in the body and pulmonary veins in reverse failure.
The symptoms of heart failure can also occur when an increased demand for blood flow to the organs can no longer be met:
- Anemia – because of inadequate oxygen-carrying capacity, cardiac output must increase to ensure adequate oxygen delivery to tissues.
- Hyperthyroidism – the heart’s pumping capacity is strongly stimulated, but so is the metabolism and blood flow to the tissues. Tachycardia, among other things, can lead to (relative) heart failure.
- Arteriovenous fistula – due to a short-circuit connection between arteries and veins, part of the cardiac output is consumed without benefit.
- Sepsis/SIRS – the dilatation of small vessels and endothelial barrier dysfunction associated with the release of inflammatory mediators requires a greatly increased ejection output of the heart to maintain arterial blood pressure.
The American Heart Association distinguishes four classes of congestive heart failure based on symptoms and four objectives based on pathological evidence. This system is called the New York Heart Association (NYHA) Functional Classification.
| Class | Patient Symptoms | Class | Objective Assessment |
| I | No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea (shortness of breath) | A | No objective evidence of cardiovascular disease. No symptoms and no limitation in ordinary physical activity |
| II | Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea (shortness of breath) | B | Objective evidence of minimal cardiovascular disease. Mild symptoms and slight limitation during ordinary activity. Comfortable at rest |
| III | Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes fatigue, palpitation, or dyspnea | C | Objective evidence of moderately severe cardiovascular disease. Marked limitation in activity due to symptoms, even during less-than-ordinary activity. Comfortable only at rest |
| IV | Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases | D | Objective evidence of severe cardiovascular disease. Severe limitations. Experiences symptoms even while at rest |
Epidemiology
According to the CDC, in 2020, about 6.2 million adults in the United States and 64.3 million people worldwide have heart failure. In 2018, cardiac disease was mentioned on 379,800 death certificates (13.4%).
Heart failure is more common in some areas of the United States than in others, with particular prevalence in the south-central and southeastern states.
Although heart conditions primarily affect the elderly, there has been an increase in the heart disease burden in younger populations.
Symptoms
The CDC lists several common symptoms of familial heart disease and non-familial congestive heart failure:
- Breath shortness during daily activities
- Trouble breathing when lying down
- Weight gain and swelling in the feet, ankles, legs, or stomach (from water retention)
- Generally feeling tired or weak
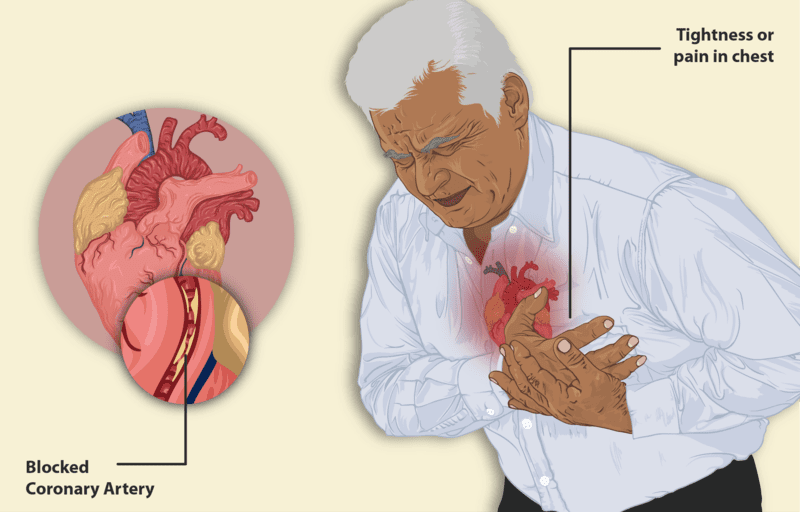
Chest pain can also be common if the symptoms are caused by a heart attack, when blood to the heart is blocked, or by sudden cardiac arrest when the heart has stopped unexpectedly. The latter is often a cause of sudden cardiac death.
The most severe form of heart failure is cardiogenic shock, which usually presents severe shortness of breath, clouding of consciousness, cold sweat, weak and rapid pulse, and cool hands and feet.
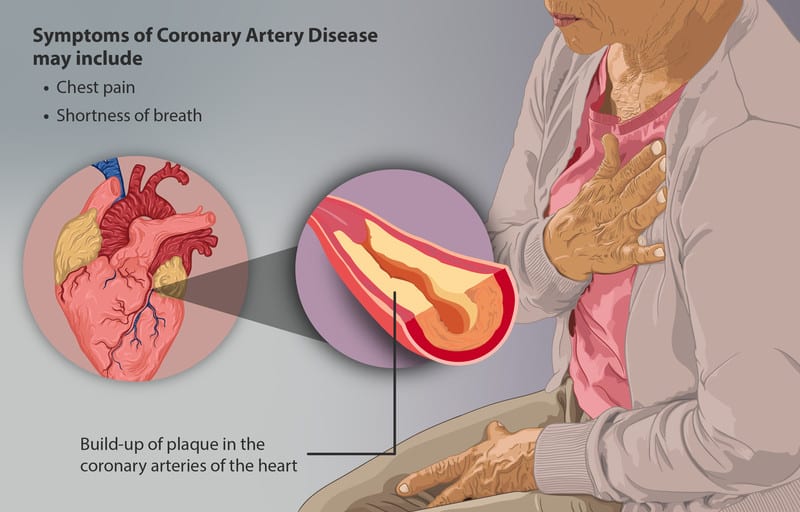
Congestive heart failure rarely occurs alone. Instead, it is often associated with concomitant diseases, which, depending on the cause of the heart failure, may include congenital heart disease, coronary artery disease, hypertension, dyslipidemia, or obesity. Atrial fibrillation can be both a consequence and a cause of heart failure. The frequency of concomitant diseases is related to the patient’s age, personal risk factors (e.g., smoking), and the heart failure’s severity.
Causes
Some physical causes of congestive heart failure include:
- Impaired contractility or filling of the heart due to direct damage to the heart muscle, e.g., in coronary heart disease, after myocardial infarction, or due to myocarditis
- Increased pumping resistance, e.g., in the case of high blood pressure in the systemic circulation (arterial hypertension) or the pulmonary circulation (pulmonary hypertension) or narrowed aortic valve
- Increased stroke volume in the case of heart defects, e.g., leaking aortic valve
- Too low a heart rate in bradycardia or too low a stroke volume in tachycardia, resulting in a decrease in cardiac output
- Constriction of the heart due to fluid in the pericardium
- Increased blood demand of the body in case of severe general disease
- anemia
- Obstructive sleep apnea syndrome (OSAS), especially in the case of right heart failure
- Side effects of numerous medications
- Excessive viscosity (viscosity, hemoconcentration) of the blood can decrease cardiac output
Congestive heart failure itself does not appear genetic. However, conditions contributing to congestive heart failure may have a genetic component.
Diagnosis
Diagnosis is made based on a physical examination, family history of heart disease, and various other diagnostic tests. Having family members with heart disease increases your risk of having a similar heart condition. Your doctor will also check for personal risk factors, such as high blood pressure, coronary artery disease, or diabetes.
Some of the additional tests are noted on Mayo Clinic and may include:
- Blood tests that look for signs of diseases that can affect the heart
- Chest X-ray to assess the condition of your lungs and heart. Your doctor can also use an X-ray to diagnose conditions other than heart failure that may explain your signs and symptoms
- Electrocardiogram (ECG) to help diagnose abnormal heart rhythms and damage to your heart
- Echocardiogram to help visualize the size and shape of your heart along with any abnormalities. Ejection fraction can also be measured with this test
- Stress test to measure the health of your heart by how it responds to exertion
- Cardiac computerized tomography (CT) scan to collect images of your heart and chest.
- Magnetic resonance imaging (MRI) to also obtain images of your heart
- Coronary angiogram to help identify spot blockages
- Myocardial biopsy to diagnose certain types of heart muscle diseases that cause heart failure
Treatment
Although congestive heart failure is often a chronic disease, there are approaches to help mitigate symptoms and help patients live longer and healthier lives. The three most common ways to treat heart failure are lifestyle changes, medications, and surgical procedures.
Lifestyle changes
To treat congestive heart failure, it’s often recommended that, if necessary, patients:
- Quit smoking
- Maintain or lose weight
- Track daily fluid intake
- Avoid or limit alcohol and caffeine
- Eat a healthy diet
- Be physically active
- Manage stress
- Keep track of symptoms
- Monitor blood pressure
- Get adequate rest
- Seek support
- Get vaccinated against the flu
- Follow heart patient guidelines for sexual activity
- Select clothing that does not restrict circulation
Medication
Congestive heart disease is a complicated disease, and patients are almost always prescribed multiple medications to treat different symptoms or contributing factors. The combinations of these drugs prolong life, improve the heart’s function, and heighten the quality of life. Some typical medications are:
- Angiotensin-converting enzyme (ACE) inhibitors: vasodilators that widen blood vessels to lower blood pressure, improve blood flow, and decrease the workload on the heart
- Angiotensin II receptor blockers: an alternative to ACE inhibitors that perform similar functions
- Beta-blockers: slows heart rate, reduces blood pressure, and limits or reverses some of the damage to your heart if you have systolic heart failure
- Diuretics: make you urinate more frequently and keep fluid from collecting in your body
- Aldosterone antagonists: diuretics that also raise the level of potassium in the blood
- Inotropes: intravenous medications that improve weakened heart pumping function and maintain blood pressure
- Digoxin (Lanoxin): increases the strength with which your heart contracts. It also tends to slow the heartbeat
Surgical procedures
When congestive heart failure is severe or a condition will benefit from correction, devices, and surgical procedures may be recommended.
- Implantable cardioverter defibrillator (ICD)
- Cardiac Resynchronization Therapy (CRT)
- Left ventricular assist device (LVAD) to help your heart pump blood to the body
- Heart transplantation
- Percutaneous coronary intervention (PCI, also referred to as angioplasty)
- Coronary artery bypass
- Valve replacement
If you liked this article, you should check out our other posts in the Nebula Research Library!
July 5, 2022
