Table of contents
- Nebula Genomics DNA Report for Vitamin D Deficiency
- What is Vitamin D Deficiency? (Part 1 of Is Vitamin D Deficiency Genetic?)
- Is Vitamin D Deficiency Genetic?
- Current Research On Vitamin D Deficiency [Updated June 2021]
- Epidemiology (Part 4 of Is vitamin D deficiency genetic?)
- Symptoms (Part 5 of Is vitamin D deficiency genetic?)
- Causes (Part 6 of Is vitamin D deficiency genetic?)
- Diagnosis (Part 7 of Is vitamin D deficiency genetic?)
- Treatment (Part 8 of Is vitamin D deficiency genetic?)
Nebula Genomics DNA Report for Vitamin D Deficiency
Is vitamin D deficiency genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of June 2021. |
What is Vitamin D Deficiency? (Part 1 of Is Vitamin D Deficiency Genetic?)
Vitamin D is a group of fat-soluble vitamins that are known primarily for their role in calcium metabolism. The most important form, vitamin D3, can be found in the skin from cholesterol when exposed to UV rays in sunlight. The rays act as a catalyst to trigger vitamin D synthesis. In food, it is found mainly in fatty fish, egg yolks, or is added to your diet as a dietary supplement.

Vitamin D plays an essential role in regulating mineral levels in the blood, like calcium and phosphate. These minerals are important in bone health and tooth formation. The associated disorder, vitamin D deficiency, leads to rickets in children and osteomalacia in adults. Further health consequences of vitamin D deficiency include osteoporosis and brittle bones in older adults.
Sufficient amounts of vitamin D are also important to reduce inflammation, promote cell growth, maintain neuromuscular and immune function, and for glucose metabolism. In fact, one of the hallmark biomarkers of home inflammation tests is vitamin D deficiency. You may choose to take a full inflammation panel (which also includes other biomarkers such as CPR), or a vitamin D test can be sold separately, often for a lower price.
For an adequate supply of vitamin D, sufficient exposure to sunlight or UV-B or, otherwise, additional intake (supplementation) is necessary. In some countries, certain foods are fortified with vitamin D for this purpose.
How is vitamin D formed?
Vitamin D is obtained from sunlight exposure, certain food, and through dietary supplements as either D2 or D3. However, these forms must go through two chemical reactions in the body in order to be used.
The first reaction occurs in the liver and converts vitamin D to 25-hydroxyvitamin D. The second reaction occurs primarily in the kidney and forms the active form, 1,25-dihydroxyvitamin D, also known as calcitriol. 25-hydroxyvitamin D is the most commonly measured form to assess levels through at-home tests. It has a half life in the bloodstream of 15 days and reflects both the natural and supplemental vitamin D in the body.
In contrast, circulating 1,25-dihydroxyvitamin D is generally not a good indicator of vitamin D levels because it has a much shorter half life and can be affected by hormones and other substances. Unless vitamin D deficiency is severe, the level of this form does not fluctuate.
Is Vitamin D Deficiency Genetic?
While vitamin D deficiency in adults is most often attributed to environmental factors, like sunlight, there is an association between childhood rickets and gene variants in the VDR gene. Thus, genetic factors are thought to play a small role in the condition.
The VDR gene encodes instructions for the vitamin D receptors, proteins that allow the body to respond to vitamin D obtained through sunlight induced synthesis or supplemented through diet. When vitamin D responsive genetic variants are turned on or off, the amounts of calcium and phosphate absorbed are controlled.
Genetic variations in the VDR gene cause vitamin D-dependent rickets type 2A (VDDR2A), also known as hereditary vitamin D-resistant rickets (HVDRR). It is a developmental bone disease characterized by low calcium and phosphate levels in the blood. Without sufficient quantities of these important minerals, bones develop as soft and weak and are prone to fracture. A common feature of this condition is abnormally curved (bowed) legs.
When the gene is mutated, the VDR protein cannot function properly. This does not mean that vitamin D is not produced but that it can’t be used for mineral absorption. The lack of calcium and phosphate absorption in the intestines slows deposition of these minerals into developing bone (bone mineralization), which leads to the features of VDDR2A.
Low calcium levels also cause muscle weakness and seizures. Most VDR gene mutations also impair hair growth, leading to hair loss.
Genome wide association studies are being conducted in order to analyze additional connections between the condition and genes.
Current Research On Vitamin D Deficiency [Updated June 2021]
Vitamin D deficiency has been a common condition around the world. This is primarily due to the disadvantageous effects it has on the health of humans. The result of the deficiency of vitamin D has effects on a wide range of health complications.
This study from 2019 explained how vitamin D production is connected to genes. There are various types of vitamin D-associated genes that harness the level of vitamin D production. They include Vitamin D Binding Protein (VDBP) and Vitamin D Receptor (VDR).
These types of vitamin D-associated genes, especially VDR, control more than 200 genes. They do this through various pathways that ultimately control the level of vitamin D. Therefore, a malfunction in these vitamin D-associated genes would alter vitamin D metabolism. Hence, causing a deficiency in vitamin D.
A recent literature review, the results of which were also published in 2019, analyzed 35 genes associated with 25-hydroxyvitamin D serum concentrations. The identified genes were related and tested on how they influence the level of vitamin D production.
The list created from this review provides a comprehensive source to help researchers understand genetic determinants of vitamin D serum levels. In total, 75% (27) of the genes identified are not commercially available for research purposes. However, the candidate list may prove vital for patient screening in clinical environments.
Furthermore, one of the more recent reports from 2020 conducted via genome-wide association has evaluated the dependents of vitamin D on genetics. This study identified 143 loci associated with 25-hydroxyvitamin D serum concentrations. Such results suggest that the condition is incredibly complex and that genetic predisposition is based on the interaction of many genes.
Epidemiology (Part 4 of Is vitamin D deficiency genetic?)
Vitamin D deficiency is a very common problem worldwide, especially for those not sufficiently exposed to natural sunlight. There are conflicting opinions as to exactly how low vitamin D levels are expected to be classified as deficient, but the generally agreed-upon level is 20 ng/mL
In the United States, some reports indicate that about 24% of the population has levels below 20 ng/mL. Other reports, such as from the Cleveland Clinic, suggest that the population at least partially deficient is closer to 42%. Prevalence rates of severe vitamin D deficiency, < 12 ng/ml, have been reported as 5.9% in the United States, 7.4% in Canada, and 13% in Europe.
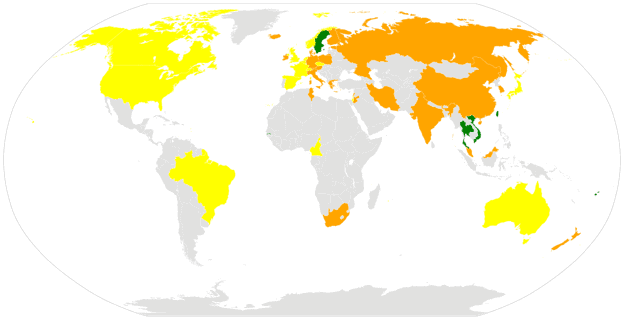
The prevalence of the disorder appears to be higher in non-white populations and also in those individuals who are overweight. In fact, over three quarters of people with darker skin, including African Americans, are vitamin D deficient.
Symptoms (Part 5 of Is vitamin D deficiency genetic?)
The condition is most obvious in children who develop a rare but serious form of bone misgrowth called rickets. Common symptoms include weakness in muscles, pain in bones, and deformities in joints. In less severe cases, children with muscle soreness and/or weakness may also have insufficient levels.
In adults, deficiency is much harder to detect without a diagnostic test. Some signs and symptoms are typical of many conditions, and they include:
- Frequent illnesses or infections
- Fatigue
- Bone pain
- Muscle weakness
- Changes in mood (such as depression)
The condition has also been associated with the onset of other disorders. Keeping your levels at a sufficient level may help prevent or even treat the following health problems:
- Increased risk of cardiovascular disease and high blood pressure
- Diabetes
- Infections and immune system disorders
- Falls in older people
- Some types of cancer, such as colon, prostate, and breast cancer
- Multiple sclerosis
Causes (Part 6 of Is vitamin D deficiency genetic?)
The most common cause of the condition is insufficient exposure to sunlight. It is very common for an individual to have a moderate deficiency because of this factor. It normally does not interfere with daily life. However, there are a number of other disorders, mainly associated with the digestive tract, that may severely reduce vitamin D levels and lead to more severe conditions.

Cystic fibrosis, Crohn’s disease, and celiac disease affect how nutrients are absorbed in the intestines. These disorders also prevent proper absorption of supplements, making it very difficult to get the necessary daily requirements. Any diseases that affect the kidneys or liver affect vitamin D levels since these organs are important for converting dietary vitamin D into a usable form.
Weight loss surgeries also run the risk of contributing to the condition because such procedures often reduce the size of the stomach or intestines. Continuous supplementation and monitoring of vitamin D (as well as other vitamins and minerals) normally keeps levels sufficient in the long term.
Some risk factors that may increase the risk of vitamin D deficiency include:
- Dark skin pigmentation
- Being elderly
- Being overweight or obese
- Lack of fish or dairy in diet
- Lack of exposure to sunlight
Some medications, such laxatives, steroids, and some that control cholesterol, seizures, and weight, also lower levels. It’s important to talk with your doctor to seek medical advice before starting any of these medications, as a vitamin D supplement may also be necessary.
Diagnosis (Part 7 of Is vitamin D deficiency genetic?)
Blood samples are needed to diagnose vitamin D deficiency. These blood tests can be used to measure either 25-hydroxyvitamin D (25-OH vitamin D) or 1,25-dihydroxyvitamin D (1,25(OH)2D).
The former is the most commonly used test as 25-OH vitamin D has a long half life in the blood, and it reflects dietary, supplemental, and sunlight driven forms of the vitamin. The latter can only be measured in the blood for a few hours and is generally not a good measure of total vitamin levels as it can be influenced by parathyroid hormone (PTH), calcium, and phosphorus levels.
Thus, most diagnostic tests only report 25-OH vitamin D. There is a good deal of controversy over how low levels must become to constitute a vitamin D status classified as deficiency. With almost half the U.S. population having at least a mild to moderate deficiency, it is difficult to diagnose what is an actual medical condition. Most experts agree that levels below 20 nmol/L are low.
NutriFit Canada defines the following levels:
- Toxicity possible: > 250 nmol/L
- High levels: 200-250 nmol/L
- Optimal levels: 80-200 nmol/L
- Mild to moderate deficiency: 25-80 nmol/L
- Severe deficiency: <25 nmol/L
Did you know you can get your vitamin D levels checked at home with consumer inflammation and vitamin D tests?
Treatment (Part 8 of Is vitamin D deficiency genetic?)
Dietary supplements are usually the most recommended vitamin D deficiency treatment.
Supplements
These supplements come in either a D2 or a D3 form. D2, the form that comes from plants, must be prescribed by a physician. D3, which comes from animals, is available over the counter. Vitamin D3 is more easily absorbed in the body and lasts longer.
According to the National Institutes of Health’s Office of Dietary Supplements, children over one year and adults should get 600 International Units (IU) of vitamin D per day. Infants younger than one year should get about 400 IUs, and adults over 70 years should get closer to 800 IU.

You should consult with your doctor as to how much supplement you should take. ALthough rare, it is possible to experience vitamin D toxicity from too much supplementation. Common side effects of vitamin D toxicity include nausea, increased thirst and urination, poor appetite, constipation, weakness, and confusion. These symptoms tend to be the result of calcium buildup of calcium in the blood.
Other treatments
Other treatment options include eating more food that contains vitamin D, and getting adequate exposure to sunlight. It’s important to remember that diet is not a large source of vitamin D and the recommended daily amount cannot be obtained through diet alone.
When getting sunlight, 10 to 15 minutes of sun exposure two to three times a week is recommended. Too much exposure to direct sunlight is a serious risk of skin cancer. You should consult your health care provider if you are unsure how much sunlight to expose yourself to. If you are older, have a darker skin color, or live in a darker climate, you may need additional exposure.
If you liked this article, you should check out our other posts in the Nebula Research Library!
July 5, 2021
