Table of contents
Nebula Genomics DNA Report for Eating Disorders
Are eating disorders genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What are Eating Disorders?
Eating disorders are a group of serious conditions in which a person has abnormal eating patterns that negatively affect their physical and/or mental wellbeing. The Diagnostic and Statistical Manual of Mental Disorders defines these conditions as mental illnesses. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge eating large amounts of food in a short amount of time.
People with these conditions tend to obsess over food or body weight. They can occur at any age, but women in young adulthood or adolescence report them most often. The main result of any of these ailments is the inability to obtain proper nutrition. This malnutrition leads to difficulty in performing daily functions.
The most well known type is anorexia nervosa, which is the focus of this genetic report. In this article, we will cover information about anorexia, as well as some other similar illnesses.
Types
- Anorexia nervosa
- Bulimia nervosa
- Binge eating disorder
- Pica
- Rumination disorder
- Avoidant/restrictive food intake disorder (ARFID)
Individuals will have different symptoms depending on the type. Anxiety, depression, obsessive compulsive disorders, and addiction disorders are common complications. Anorexia and bulimia can lead to life-threatening malnutrition if severe. These conditions can also harm the heart, digestive system, bones, and teeth and mouth, and lead to other diseases.
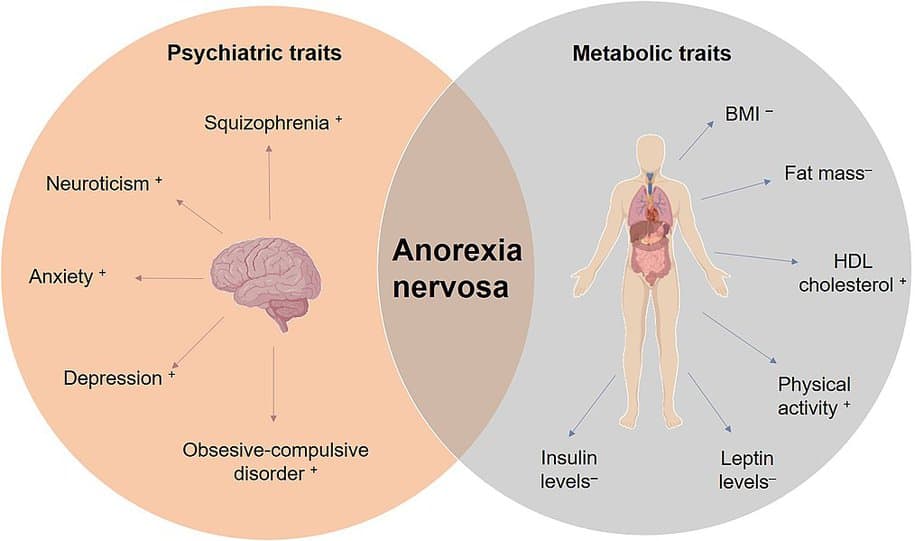
While the exact cause of these conditions is unknown, experts largely believe them to be a combination of genetic and environmental factors. Societal pressures to look thin and have a certain body type are also contributors to the condition.
Are Eating Disorders Genetic?
Some studies have suggested that having a family member with an eating disorder can increase your risk 7-12 times. Experts believe shared genetic predispositions, as well as environmental and psychological factors, also play a role.
In 1996 a private European foundation, Price Foundation, sought to understand the genetic basis of eating disorders. Specifically, genetic research identified several genes on chromosomes 1 and 10 as likely contributing to anorexia and bulimia.
Later research at the University of Iowa and University of Texas Southwestern Medical Center found that individuals with mutations in the ESRRA and HDAC4 genes had a 90% and 85% chance of developing an eating disorder.
ESRRA: This gene codes for a nuclear receptor closely related to the estrogen receptor. The protein is required for the activation of mitochondrial genes as well as increased mitochondrial biogenesis.
HDAC4: This gene codes for an enzyme that modifies proteins called histones, structural proteins that attach to DNA and give chromosomes their shape.
The research study suggested that both of these genes are involved in a pathway that increases a person’s desire for food when they are hungry. Thus, genetic variants can prevent the natural desire to eat and cause a genetic predisposition.
Researchers at the UNC School of Medicine, led by Cynthia Bulik, Ph.D., are also seeking to identify hundreds of markers responsible for a genetic predisposition to eating disorders through an international study funded by the National Institute of Mental Health.
Current Research on Eating Disorders
There is not enough research about to what extent eating disorders are genetic. In March 2019, Psychiatric Clinics of North America, with the participation of several prestigious universities from the USA, Sweden, and Canada, published a paper on the topic called “Genetics of Eating Disorders: What the Clinician Needs to Know.”
The COVID-19 pandemic has impacted the number of cases, and this study looks at the context that has led to such an increase.
Other investigations, such as The Binge Eating Genetics Initiative (BEGIN), examine the relationships of genetic eating disorders, specifically gut microbiota, and behavior in bulimia nervosa and binge-eating disorder. This particular study took 1000 individuals who provided biological samples during 30 days of research.
The Klarman Family Foundation announced in 2020 their contribution to the research of eating disorders. This initiative, dubbed ANGI – Anorexia Nervosa Genetics Initiative, identified eight genetic variants associated with anorexia nervosa.
The authors in this Psychological Medicine article makes a very detailed case on how this wide-genome era has helped unlock all the biological bases for eating disorders. This article points out that there are five genome-wide association studies on anorexia nervosa alone.
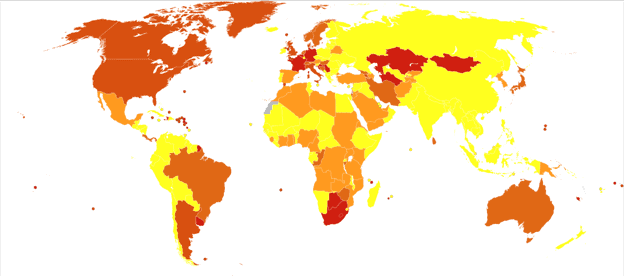
Epidemiology
Overall, 9% of the U.S. population will experience an eating disorder in their lifetime. The lifetime prevalence of anorexia nervosa in the U.S. is estimated to be between 0.3-1%. Although, some studies have estimated it as high as 4%.
These psychological and physical conditions are more common in women than in men, with some estimates suggesting that anorexia and bulimia occur ten times more often in females.
In 2020, it was believed that 10,200 deaths each year are the direct result of an eating disorder.
Symptoms
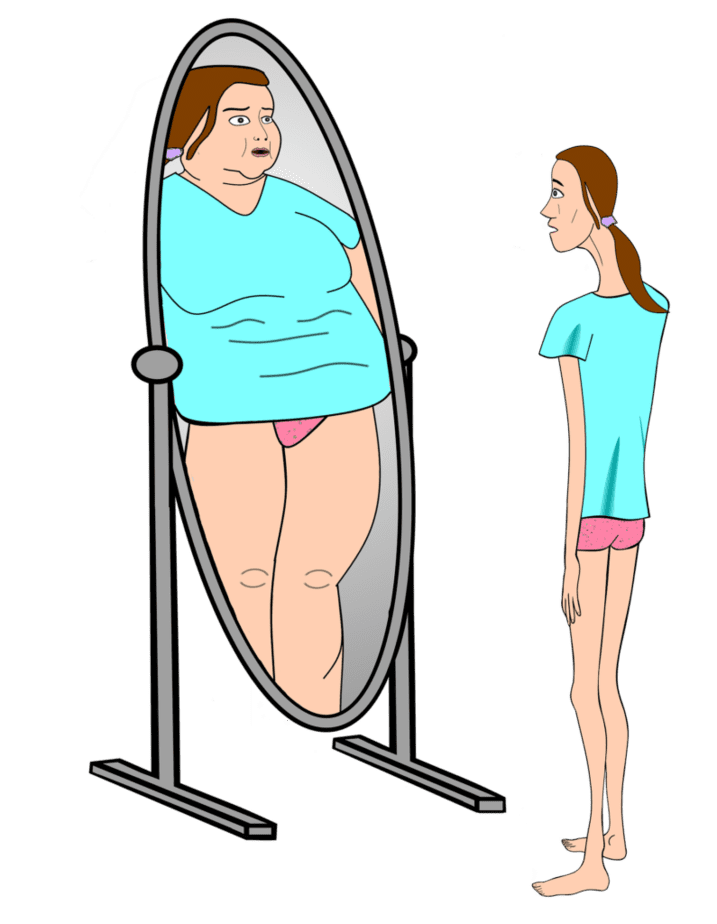
The symptoms of the condition depend primarily on the type of eating disorder present. There are some general signs of developing anorexia or another eating disorder that mainly focus around behavior around food, such as frequent dieting and skipping meals. Patients may also have an obsessive personality trait about worrying about body appearance. Typically they experience feeling a lack of control over eating.
Physical symptoms include dizziness, muscle weakness, feeling cold, poor wound healing, and dental problems associated with vomiting. A more comprehensive list of symptoms can be found on the National Eating Disorders Association (NEDA) website.
If you are concerned about a friend, relative, or yourself, the NEDA helpline is available for access to professional help.
Generally, an individual won’t have all the behavioral and physical symptoms at once. The exact signs are usually unique to each individual. People with anorexia will have symptoms unique from people with binge eating disorder and so on.
Types
Each type of the condition has a more specific range of symptoms:
Anorexia nervosa
- Dramatic weight loss
- Intense fear of gaining weight
- Preoccupation with losing weight, food, calories, fat grams, and dieting
- Resists or is unable to maintain a body weight appropriate for their age, height, and build
- Excessive exercise despite inappropriate need
Bulimia nervosa
- Binge eating, which means to eat large amounts of food until uncomfortably full
- Evidence of purging behaviors, or vomiting
- Dental problems, such as enamel erosion, cavities, discoloration of teeth from vomiting, and tooth sensitivity

Binge eating disorder
- Secret recurring episodes of binge eating (eating an inappropriate amount of food in a short period of time)
- Feelings of disgust, depression, or guilt after overeating, and/or feelings of low self-esteem
Pica
- The persistent eating of substances that are not food and do not provide nutritional value such as paper, soap, chalk, paint, pebbles, etc.
Rumination disorder
- Repeated regurgitation of food
Avoidant/restrictive food intake disorder
- Dramatic weight loss
- Limited range of preferred foods that becomes narrower over time
- Fears of choking or vomiting
- No body image disturbance or fear of weight gain
Causes
Eating disorders are mental disorders, which tend to have unknown or unclear causes. Like most mental disorders, both genetic factors and environmental factors most likely play a role. Physiological and emotional problems may also contribute to the disorders.
Adolescent and young female adults are more likely than adult males to have an eating disorder. There are several risk factors that may contribute to an increased risk of developing an eating disorder.
Family history, including having a parent or sibling with an eating disorder, increases your chances of developing one as well. Other mental health issues, such as anxiety and depression, also put you at higher risk. Strict dieting or starvation can change the way the brain works. This change can lead to an eating disorder and make returning to a regular diet routine more challenging.
Stress in any part of life is another factor that can lead to many mental disorders, including eating disorders.
Diagnosis
These conditions are typically diagnosed based on signs, symptoms, and eating habits. Either a primary care doctor or a mental health professional can diagnose an eating disorder.
Doctors use a physical exam to rule out other medical conditions that might be affecting your digestive system. If other conditions are ruled out, a psychological evaluation can be used to diagnose the state positively.
A doctor or mental health professional will focus on thoughts, feelings and dietary habits. These questions may be presented as a questionnaire. In addition, other biological tests may be performed to check for medical complications.
Treatment
To treat an eating disorder, a team of health professionals normally need to address both the psychological and physical symptoms. Generally, people with eating disorders will be recommended towards nutrition education, treatment of the psychiatric disorder, and medication. If severe, some cases may require hospitalization.
Psychotherapy
The condition is a psychiatric illness. Also called talk therapy, this treatment can help patients address their eating problems by replacing bad habits with healthy ones. Family based therapy is most commonly recommended for teens and young adults.
Cognitive behavioral therapy is another common strategy, especially for people with bulimia and binge eating and purging disorder. This therapy focuses on improving mood and dealing with stress.
Medications
Medications cannot cure or treat eating disorders directly. They are sometimes prescribed to help treat the symptoms and underlying causes. Typical prescriptions may include antidepressants and anti-anxiety medications.
Hospitalization
Eating disorders, but especially anorexia and bulimia, can be life threatening and require hospitalization. In these cases, the patients are usually suffering from extreme malnutrition. Day programs or outpatient care is also available in some cases. Full hospitalization is usually required when the patient needs long term, intensive care.
More treatments and resources can be found from the National Institute of Mental Health.
If you liked this article, you should check out our other posts in the Nebula Research Library!
February 10, 2023
