Table of contents
Nebula Genomics DNA Report for Depression
Is depression genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Depression?
Depression (also called major depressive disorder or clinical depression) is a mood disorder or mental illness. According to the American Psychiatric Association, it causes severe symptoms that affect how individuals feel, think, and handle daily activities.
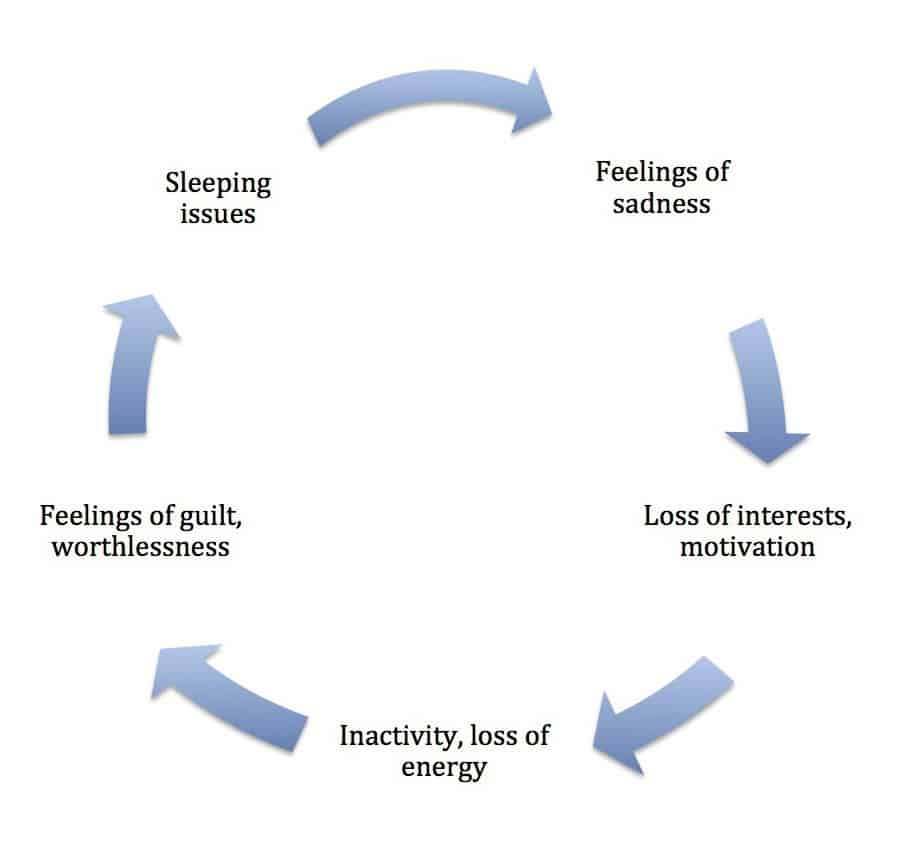
People typically have symptoms of depressed mood, brooding, a feeling of hopelessness, and a diminished drive. Frequently, they lose joy and feelings of pleasure, self-esteem, performance, empathy, and interest in life. Thus, their enjoyment and quality of life are often impaired.
These complaints also occur in healthy people in the context of grief after a loss experience and need not differ in appearance from depression; however, they usually pass by on their own. Illness is present when the symptoms persist for an excessive length of time or when their severity and duration are out of proportion to the factors that trigger the symptoms.
It is one of the most common mental disorders in the United States. For some individuals, the disease can interfere with or limit one’s ability to carry out major life activities.

Is Depression Genetic or Environmental?
The causes of depressive disorders are complex and only partially understood. There are both predispositions and acquired susceptibilities to their development. Biological factors and environmental factors such as social or psychological stress can trigger acquired susceptibilities.
It is most likely that a variety of factors contribute. The condition often runs in families and is more common in individuals who have a family member with depression.
Scientists suspect that a variation in the promoter region of the serotonin transporter single gene 5-HTTLPR is a significant genetic factor for its occurrence. The gene is located on chromosome 17q11.1-q12 and occurs in the population in different forms. This discovery can lead to a more extensive study of the genetics related to the condition.
Carriers of the short version of this allele react more sensitively to psychosocial stress and are said to have up to twice the genetic risk of developing depression than the long allele version carriers. In two meta-analyses in 2011, scientists confirmed the association between the short allele and the development of depression after stress.
These results essentially answers the question “Is there a genetic component to depression?” In a meta-analysis in 2014, researchers found significant data for a total of seven candidate genes: 5HTTP/SLC6A4, APOE, DRD4, GNB3, HTR1A, MTHFR, and SLC6A3.
Depression genes
There is no depression gene. However, experts have associated multiple single genetic variations, making it more likely that an individual will experience the condition. It is most likely that genetic variants affect a small contribution to an individual’s overall risk compared with the general population.
Several extensive genome-wide association studies have proposed potential connections with a unique combination of genes. Many are associated with genomic testing companies, such as 23andMe.
People with genetic depression have physical differences in their brain and brain chemistry. Changes in function and the effect of neurotransmitters involved in maintaining mood stability may play a significant role.
Additionally, changes in the body’s balance of hormones may cause or trigger the condition. Pregnancy, thyroid problems, menopause, or other health conditions can cause these hormone changes. Extreme life stress may also be a trigger, especially if an individual is genetically predisposed.
Current Research on Depression
There have been thorough studies about the condition in the last five years, with more than 11 thousand studies cataloged and detailed in PubMed. The year 2017 was an exciting year for the study of genetics of major depression as genome-wide studies associated genetic variants.
This abstract on Genetic Effects influencing risk for major depressive disorder in China and Europe tries to explain how a certain fraction of SNPs display correlations to major depressive disorder in this demographic. More recently, this study on Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications delves into the social, psychological, and biological aspects of the condition.
You may want to take a look at this abstract about The genetic basis of major depression updated on March 8, 2021.
Epidemiology
According to the National Institute of Mental Health (a part of the National Institutes of Health), an estimated 17.3 million adults in the United States (7.1% of all U.S. adults) had at least one major depressive episode in 2017. Prevalence was higher in women than males. While the condition can occur at any age, it most often begins in the teens, 20s, or 30s. Prevalence is highest in individuals between the ages of 18-25.
According to the World Health Organization, in 2020, more than 264 million people suffer from depression worldwide. While it is a significant contributor to the overall global burden of disease, prevalence is still greater in women than in men worldwide.
Risk Factors and Prevention
According to Mayo Clinic, factors that seem to increase the genetic risk of developing or triggering depression include the following. Many stress situational events.
- Depressive personality traits, such as low self-esteem and high instances of dependence, self-criticism, or pessimism
- Traumatic or stressful events
- Family history of depression, bipolar disorder, alcoholism, or suicidal thoughts, especially having a parent, sibling, or identical twin struggling with depression
- Being lesbian, gay, bisexual, transgender, or non-binary
- History of other common mental health disorders
- Alcohol or substance abuse (drugs)
- Serious or chronic illness
- Certain medications such as high blood pressure medications or sleeping pills
An individual who thinks they may be at higher risk can take some steps to prevent episodes:
- Take steps to control stress
- Reach out to family members and friends
- Get treatment at the earliest signs
- Consider long-term maintenance treatment
Characteristics and Symptoms
There is often an overlap between depressive and anxiety disorder symptoms and symptoms of bipolar disorder. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in the United States defines the condition as:
- A period of at least two weeks when a person experienced a depressed mood or loss of interest or pleasure in daily activities and had a majority of specified symptoms, such as problems with sleep, eating, energy, concentration, or self-worth
- No exclusions were made for major depressive episode symptoms caused by medical illness, substance use disorders, or medication.
The severity, frequency, length, and amount of recurrent depression symptoms vary widely depending on the individual.
Some people may experience depression once in their lives, while others have multiple episodes. For many, symptoms are noticeable enough to interfere with daily life and relationships with others. If you feel depressed, experts recommend you to see a doctor or mental health professional as soon as possible.
If you feel suicidal, you should call 911 or your local emergency number immediately. You can reach the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Children and young adults
Doctors may find it harder to distinguish symptoms in children and young adults since age-typical behavior often overlay the depressive symptoms. This makes the diagnosis more difficult.
In younger children, additional symptoms may include sadness, anger, clinginess, concern, and pains, refusing school, or being underweight. Teens may show these same signs. But symptoms may also include feeling negative and worthless, irritability, underperformance or lack of school attendance, feeling misunderstood and extremely sensitive, resorting to recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in everyday activities, and avoidance of social interaction.
Older adults
The condition often goes undiagnosed and untreated in older adults as they may feel reluctant to seek help. Some less obvious symptoms in older adults include memory problems, personality changes, physical aches or pain, fatigue, loss of appetite, sleep problems, loss of interest in sex, not wanting to socialize, and suicidal feelings.
Forms under Unique Circumstances
Some forms of depression occur in tandem with life or medical events. A doctor may add a specifier to clarify the type of depression present. Some common types are:
- Persistent depressive disorder – a depressed mood that lasts over two years
- Anxious distress – accompanied by unusual restlessness or worry
- Mixed features – depression and mania
- Psychotic features – accompanied by delusions or hallucinations
- Peripartum – occurs during pregnancy or in the weeks or months after delivery (postpartum depression)
- Seasonal affective disorder- related to seasonal changes and reduced sunlight exposure

Diagnosis
A family physician or a psychiatrist in the health care system most often diagnoses this condition. They diagnose the disease when an individual experiences five or more symptoms during two weeks. Additionally, the individual experiences at least one of the symptoms: (1) depressed mood or (2) loss of interest or pleasure.
Possible symptoms:
- Depressed mood most of the day, nearly every day.
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day.
- Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day.
- A decrease in thought ability and a decline in physical movement (not observable by the patient, not like feelings of restlessness or being slowed down).
- Tiredness or loss of energy almost every day.
- Feelings of uselessness or excessive or inappropriate guilt almost daily.
- Reduced ability to process thought or concentration, or faltering, nearly every day.
- Recurrent thoughts of death, random suicidal ideas, or a suicide attempt, or an elaborate plan for committing suicide.
A doctor may recommend a physical exam, lab tests, a psychiatric exam, or use DSM-5 criteria to diagnose an individual. A physical exam can determine if depression is linked to an underlying health problem. Likewise, lab tests can detect problems related to the disease, such as an abnormally functioning thyroid. The psychiatric exam may include a questionnaire that helps a mental health professional analyze symptoms, thoughts, feeling, and behavior patterns.
Treatment
Doctors can successfully treat depression in the majority of individuals. Advice, diagnosis, or treatment should always come from a healthcare professional. Possible treatment options include drug treatment with antidepressants, psychotherapy, or a combination of drug and psychotherapeutic treatment, which is increasingly being supplemented and supported by online therapy programs.
Other therapy methods such as electroconvulsive therapy, light therapy or awake therapy, sports, and exercise therapy complement the treatment options. The success of treatment depends heavily on the individual, and it often takes trial and error to determine the best approach.
Medications
Depression is a medical condition treated with antidepressants. They improve the way the brain uses certain chemicals to control mood or stress. Antidepressants may take 2-4 weeks to work, and going off of them requires consultation with a doctor and medical advice. Stopping them abruptly can cause withdrawal symptoms.
Psychotherapies
Examples of successful psychotherapies include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and problem-solving therapy. Talk therapy has the purpose of helping people with depression identify the root of their condition.
Brain stimulation therapies
If medications do not seem effective, the specialist may recommend electroconvulsive therapy (ECT). ECT can provide relief for people with severe depression for whom traditional medicines did not work or cannot be taken safely. ECT may cause some side effects, including short-term confusion, disorientation, and memory loss.
The treatment is not painful, and patients cannot feel electrical impulses. You should always consult with a doctor before undergoing ECT.
In cases of high suffering and an unsatisfactory response to outpatient therapy and psychotropic drugs, especially in cases of imminent suicide, treatment in a psychiatric clinic should be considered. Such a treatment offers the patient a daily structure and the possibility of more intensive psychotherapeutic and medical measures.
Some smart things to do during treatment involve exercise, setting realistic goals, spending time with others, being prepared for a gradual (not immediate) mood improvement, and continuing to educate yourself about the disease. However, no informal education is a substitute for professional medical advice.
Did you like this article? Check out more reports like this in the Nebula Research Library! Here, you can find more articles on mental health conditions such as Alzheimer’s disease, and other disorder related to Alzheimer’s like dementia.
You can also read about medications such as the antidepressants Lexapro and Zoloft on our blog.
June 10, 2022
