Table of contents
Nebula Genomics DNA Report for Pancreatic Cancer
Is pancreatic cancer genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of June 2021. |
What is Pancreatic Cancer?
Pancreatic cancer, also known as pancreatic carcinoma, is a malignant tumor of the pancreas. It occurs when DNA mutations cause cells to grow uncontrollably and form a tumor. The majority of tumors affect the part of the pancreas that produces digestive enzymes, predominantly affecting the ducts within the organ. These “ductal adenocarcinomas” are among the most common cancers syndromes.
The cancer is divided into two large categories and multiple subcategories:
- Exocrine pancreatic cancer: this type forms in exocrine cells, which make up the exocrine gland and ducts of the pancreas. They make up more than 95% of all pancreatic cancers.
- Adenocarcinoma
- Squamous Cell Carcinoma
- Adenosquamous Carcinoma
- Colloid Carcinoma
- Neuroendocrine Pancreatic Cancer: this type develops from cells in the endocrine gland of the pancreas, which secretes the hormones insulin and glucagon.

Pancreatic carcinomas grow aggressively and form metastases at an early stage. So far, they can only be treated by surgical removal, and many are only detected at such an advanced stage that no cure is possible. Chemotherapy and radiotherapy have a supportive function in the treatment of pancreatic cancer.
During surgery, the pancreas is partially or completely removed (pancreatectomy), and the interrupted bile and pancreatic ducts are reconnected to the intestinal tract. Although it is an aggressive cancer, the cure rate has improved in recent decades.
In addition to malignant tumors of the pancreas, there are also benign tumors, such as serous cystadenoma.
Is Pancreatic Cancer Genetic?
It is largely understood that pancreatic cancer can be caused by either inherited genetic mutations, acquired genetic mutations, or a combination of both.
Familial pancreatic cancer includes inherited mutations, genetic changes passed from parent to child. This includes having a family history of pancreatic cancer or other types in the family. About 10% of patients diagnosed with pancreatic cancer have some form of hereditary component.
Having a family member with other genetic syndromes, including cystic fibrosis, familial adenomatous polyposis (FAP), Lynch syndrome, and familial atypical multiple mole malignant melanoma (FAMMM) syndrome, may also increase the risk of developing pancreatic cancer. Other genes associated with a higher risk of pancreatic cancer include:
PRSS1: Gene mutations in the PRSS1 gene cause most cases of familial pancreatitis. This gene makes instructions for an enzyme in the pancreas that helps with the digestion of food. It is estimated that 65 to 80 percent of people with hereditary cancer of the pancreas have mutations in the PRSS1 gene.
BRCA: Most widely known as the “breast cancer genes,” BRCA1 and BRCA2 work to suppress breast tumors. When germline mutations cause the genes to no longer work properly, breast cancer often results. Certain mutations in these genes are also thought to be linked to pancreatic cancer.
PALB2: This gene works as a partner with the BRCA2 gene to repair DNA and prevent cancer growth. Mutations in this gene are thought to contribute to both breast and pancreatic cancer risk.
Acquired mutations are those that result from exposure to cancer-causing agents, such as tobacco smoke. This is why smoking is so closely related to a high risk of pancreatic cancer. Causes of other acquired mutations are unknown.
Genetic testing and consultation with a genetic counselor may be able to assess your risk. Learn more about diagnostic testing for pancreatic cancer. Sometimes, non-diagnostic testing can be done from home such as through the companies Myriad Genetics, Color, CircleDNA, and Nebula Genomics.
Current Research on Pancreatic Cancer
Some cancer research has linked the risk of developing pancreatic cancer to genetic influences. A 2018 study made a correlation between germline mutations (these are mutations that can be passed on to offspring) and the risk of developing genetic pancreatic cancer. This study showed that mutations in genes associated with pancreatic cancer had a higher occurrence in patients with family history than those without family history of the disease. However, this study did conclude that more research had to be done on other populations to draw further inferences.
A study conducted in 2019 attempted to link the epidemiology of pancreatic cancer with development of preventive measures. The study also identified major risk factors for pancreatic cancer. While there wasn’t much data to make a concrete link between the epidemiology and preventive methods, the study identified various risk factors, dividing them into two groups: modifiable and non-modifiable.
Also, another study conducted in 2019 aimed to exploit new discoveries made on how the body’s immune system attempts to fight pancreatic cancer and how the cancer also combats the immune system. This study aimed to examine these mechanisms to see if more successful immunotherapies can be developed against the disease.
If you’d like to know about the therapy options for pancreatic cancer, this is a publication on the progress that has been made so far in the therapy options for pancreatic cancer.
Epidemiology
The National Cancer Institute, an institute at the National Institutes of Health, regularly surveys and reports instances of cancer cases and deaths in the United States. According to their statistics, there were an estimated 83,777 people living with pancreatic cancer in the United States in 2018. Based on 2016-2018 data, 1.7 percent of men and women will receive a pancreatic cancer diagnosis sometime in their lifetime. This makes it the 11th most common cancer in the United States.
Pancreatic cancer is more common with increasing age and slightly more common in men than women.
Because this cancer is difficult to detect early, it is often only diagnosed at an advanced state, with the 5-year survival rate being 10.8%. This rate is affected by whether the cancer has metastasized or not. Localized cancer survival rates are as high as 41.6%.
Based on statistical forecasting, it is estimated that there will be 60,430 new cases in 2021 (3.2% of all cancer cases).
Symptoms
This cancer is often called a silent disease because it typically goes unnoticed until an advantage stage causes serious symptoms. By the time cancer symptoms become apparent (i.e., the tumor becomes large enough to be noticed) the cancer has often spread throughout the body.
According to the Cancer Treatment Centers of America, most symptoms of pancreatic cancer are not specific to the disease. The earliest symptoms may include jaundice, a yellowing of the skin and the whites of the eyes, which is caused by an excess of bilirubin (a substance made by the liver). Sudden weight loss may also be an early warning sign.
Weight loss may be accompanied by other symptoms affecting the stomach region. Abdominal pain in the upper and middle belly that extends to the lower back may occur if a tumor has grown large enough to press against other organs. Nausea and vomiting occur if tumors have grown near the stomach region. Gallbladder and liver swelling may also occur.
Unlike a pancreatic tumor, a swollen gallbladder can often be discovered through a routine physical exam. Of course, these abdominal issues may be caused by many other conditions other than cancer.
Other symptoms that often occur once the disease is more advanced include:
- Light-colored stools
- Dark-colored urine
- Itchy skin
- Changes in the presence or severity of diabetes and abnormal blood sugar levels
- Blood clots
- Fatigue
- Loss of appetite
Causes
Although the causes of pancreatic cancer are not well known, many environmental and genetic risk factors have been discovered.
Risk factors
Smoking: The largest factor involved with an increased risk of developing pancreatic cancer is smoking. According to the American Cancer Society, the risk is about twice as high among smokers compared to those who have never smoked.
It also works the other way. That is, quitting smoking starts to reduce a person’s risk of developing the disease almost immediately. Cigar smoke and smokeless tobacco products may also carry a risk.

Obesity: People who are obese are 20% more likely to develop pancreatic cancer. This risk may be increased if the weight is carried around the waist.
Diabetes: The condition is more common in people with diabetes, which may be an effect of the correlation between diabetes and obesity. This connection is especially true of those with type 2 diabetes. The connection between pancreatic cancer and type 1 diabetes is less clear.
Chronic pancreatitis: A long-term inflammation of the pancreas is linked with an increased risk of pancreatic cancer.
Heavy alcohol use: Some studies suggest that heavy alcohol use has an effect on increased risk. However, this may be due to an indirect effect in which alcoholism causes chronic pancreatic inflammation.
Peutz-Jeghers syndrome: A Dutch study conducted in 2015 showed that PJS patients have a highly increased risk for developing pancreatico-biliary cancer.
Diagnosis
The tumor is on the pancreas, which is buried deep in the abdomen. Its placement means that early detection is very difficult, which is why it is often not detected until later stages. If the disease is suspected, your doctor may perform the following tests:
Imaging
Multiple imaging tests can be performed in order to create an image of the pancreas. These images can be used to detect abnormal growths, such as tumors. These imaging techniques include ultrasound, magnetic resonance imaging (MRI), computerized tomography (CT) scans, and, sometimes, positron emission tomography (PET) scans. An endoscopic ultrasound (EUS) passes a small ultrasound device called an endoscope through your esophagus and into your stomach in order to obtain the images.
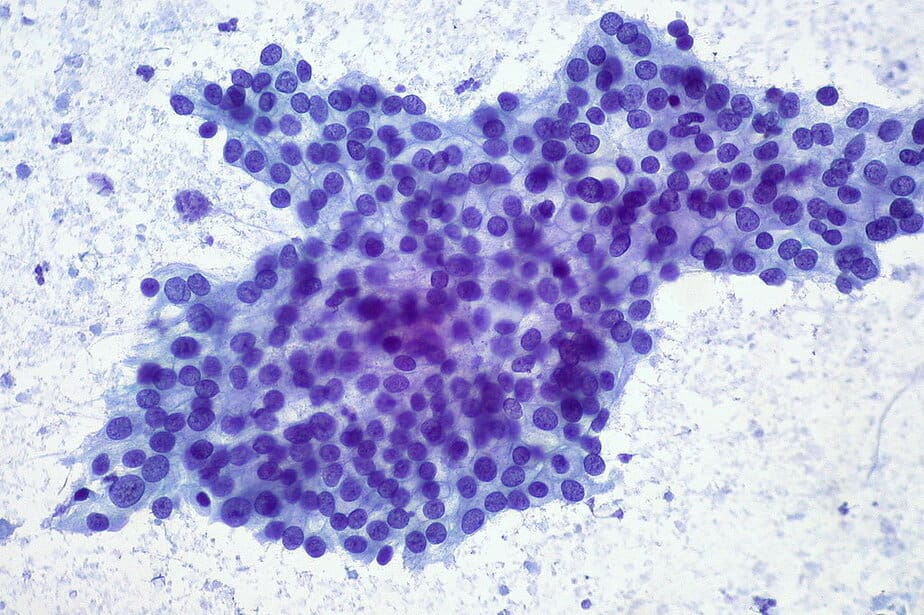
Biopsy
A biopsy requires taking a small tissue sample from your pancreas and observing it under a microscope. A sample can be collected by either EUS or by inserting a needle through your skin and into your pancreas (fine-needle aspiration).
Blood tests
Some blood tests can detect certain tumor markers shed by the pancreas, such as CA19-9. As some patients don’t experience this shedding, this test is not as useful as other diagnostic procedures.
Stages of pancreatic cancer range from I to IV. Stage I indicates that the cancer is localized to the pancreas, while stage IV indicates that the cancer spreads to other parts of the body.
Treatment
Treating pancreatic cancer largely depends on the specific cancer stage and location of the tumor. Sometimes, overall health and personal preference also influence pancreatic cancer treatment options.
Most treatment options focus on eliminating the disease. Treatment may include surgery, radiation, chemotherapy, or a combination. If the cancer is advanced, the focus may be on quality of life and palliative care.
Surgery: Sometimes, only a part of the pancreas needs to be removed. If the tumor is the pancreatic head, surgeons will perform what is commonly known as a Whipple procedure. This surgery removes the head of the pancreas, the duodenum (first section of the small intestine), the gallbladder, part of the bile duct, and lymph nodes in the vicinity.
The surgeon reconnects the remaining parts of these organs. If the tumor is located in the body or tail, surgeons will remove the left side (body and tail) of the pancreas. The spleen is also removed.
In some cases, the entire pancreas can be removed. Patients who undergo this type of surgery (pancreatectomy) need lifelong insulin and enzyme replacement but can otherwise lead a normal life.
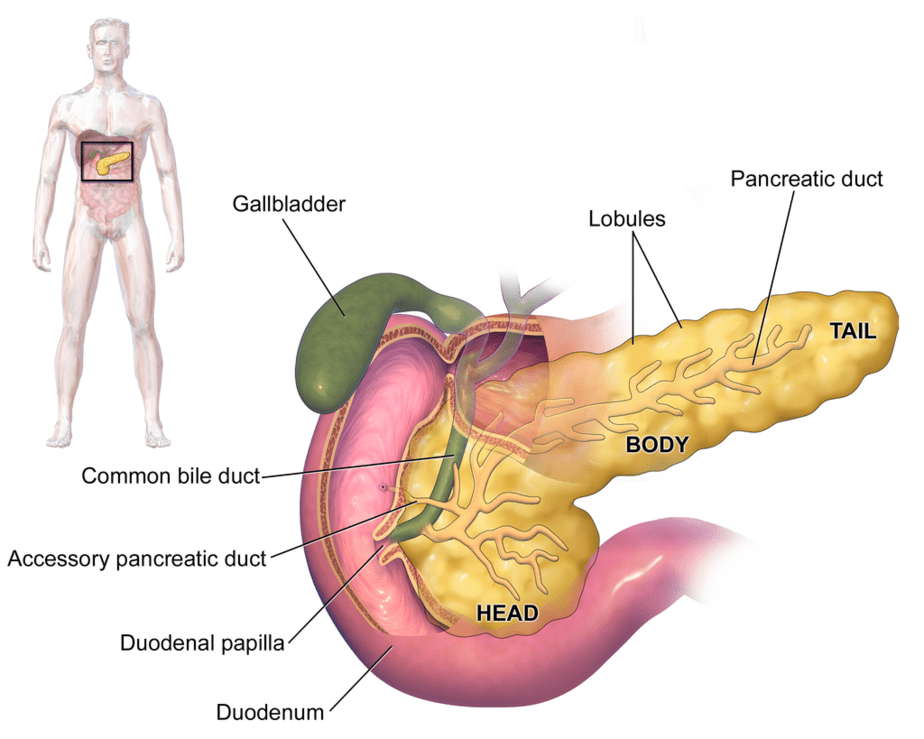
WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0, via Wikimedia Commons
If an advanced stage of the disease is found to invade surrounding blood vessels, very specialized surgeons may be able to offer special surgery that includes removing and reconstructing affected blood vessels.
Any of these procedures tend to be very complex surgeries. There is always a risk of serious side effects, including bleeding and infection. Patients may also experience nausea and vomiting. Recovery includes several days in the hospital followed by several weeks at home.
Chemotherapy: This is a drug treatment that is used to help kill cancer cells. Chemotherapeutic drugs are either intravenous injections or oral doses. Multiple chemotherapies are often used at the same time. Sometimes, chemotherapy is used in combination with radiation therapy.
Radiation therapy: This treatment uses high-energy beams, such as those made from X-rays and protons, to destroy cancer cells. Radiation is often used before or after surgery or as a substitute when surgery is not recommended. Radiation therapy usually targets only the affected area of the body.
Targeted therapy: These drugs work differently from chemotherapeutics in that they target specific factors in the body that are influencing the cancer. These are newer drugs and there are many still in clinical trials.
To learn more about this disease, you can explore many online resources, including Cancer.org and the Pancreatic Cancer Action Network, where you can find treatment support, learn about new research, and also make tax-deductible donations.
Prognosis
While pancreatic cancer is often incurable, prognosis for the disease is can still be positive in some cases. Long-term prognosis depends on the degree of the tumor spread, lymph node involvement, and the size and type of the tumor at the time the cancer is diagnosed. Basically, the most important factor in the probability of pancreatic cancer getting cured is how quickly it is diagnosed. If diagnosed early, there is a chance of the patient getting cured.
However, the chances of early diagnosis are decreased because the disease shows little or no symptoms until the cancer is well advanced.
For patients who do get an early diagnosis, their tumor is not yet metastasized, hence they can be surgically removed (resected). However, the tumor must still be in either the first or second stage (stage I and II tumors). Some stage III tumors also have a chance of being resected; however, this is dependent on the skill of the surgeon in charge.
Despite surgical removal, some of these tumors can still grow back. Hence, even patients whose tumors were resected live for an average of 2.5 years after their diagnosis. The five-year survival rate is between 20 – 30 percent of all pancreatic cancer patients.
You can also see our posts in the Genetic Cancer Testing series and explore the Nebula Research Library to learn about hundreds of other conditions influenced by genetics, including many cancers.
August 3, 2022
