Table of contents
Nebula Genomics DNA Report for Alzheimer’s
Is Alzheimer’s genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

To learn more about how Nebula Genomics reports genetic variants in the table above, check out the Nebula Research Library Tutorial!
What is Alzheimer’s?
Alzheimer’s disease is a neurodegenerative disease. It occurs in its most common form in people over the age of 65, characterized by increasing dementia.
Although popular language uses the terms interchangeably, Alzheimer’s disease and related dementias refer to different conditions. Dementia is the generic term for various diseases that affect the brain. Experts clearly describe the scientific discussion on the basis of diagnostic criteria. Increasing loss of cognitive functioning, emotional and social abilities are common to all types of dementia.
Alzheimer’s disease is the most common form of dementia, accounting for 60-80% of cases.
This disease is progressive, where dementia symptoms gradually worsen over time. As of 2017, it was the sixth leading cause of death in the United States.

Is Alzheimer’s Genetic?
To date, we have not fully clarified the cause of Alzheimer’s disease, although we suspect a combination of factors. The greatest risk factors for Alzheimer’s are:
- Older adults of advanced age
- Carrying the e4 form of the APOE gene
- Family history
Understanding the genetics: Genetically, researchers have identified a variant in the gene for ApoE as a risk factor for the development of the disease. In addition, causal mutations in three different risk genes called presenilin-1 and -2 and amyloid precursor protein (APP). They beleive these mutations cause only a small percentage of cases (1 percent or less).
However, patients inheriting a mutation to the APP gene or presenilin 1 gene are guaranteed to develop Alzheimer’s disease, while those inheriting a mutation to the presenilin 2 gene have a 95 percent chance of developing it.
Certain genetic mutations and the extra copy of chromosome 21 that characterizes people with Down syndrome are uncommon genetic factors that strongly influence Alzheimer’s risk.
A genetic test can prove the predisposition for Alzheimer’s genes. If interested in genetic testing, you should check out this product reviews:
- 23andMe – Health + Ancestry service
- GeneDx – wide variety of clinical genomic tests
- Invitae – diagnostics, proactive health, and reproductive health
- Myriad Genetics – diagnostics, reproductive tests, and precision medicine tests
Current Research on Genetic Alzheimer’s
African-American are twice as likely to develop the disease than their non-Hispanic white counterparts from the same community. In December 2020, AIMS Neuroscience published an article on the various genetic elements and biological processes that are concerned with Alzheimer’s disease.
The result shows the major biological pathways involved and the mechanism through which each of these pathways helped in the development of the disease.
In March 2021, scientists led by Yoshihide Nakamura published an article on how enhancing calmodulin binding to the ryanodine receptor can help limit neuronal loss associated with Alzheimer’s disease. The aim of this experiment was to help find new ways of treating the condition.
According to meta-analyses of randomized clinical trials, controlling hypertension can reduce the risk of cognitive impairment and dementia. JAMA neurology conducts another study titled “Association of Intensive vs. Standard Blood Pressure Control With Magnetic Resonance Imaging Biomarkers of Alzheimer Disease: Secondary Analysis of the SPRINT MIND Randomized Trial.” This study examines the effects of controlling high blood pressure or hypertension on Alzheimer’s disease.
The study involves 454 adults with hypertension subjected to intensive treatment and follow-up magnetic resonance. The result shows that subjecting a patient to intensive or standard blood pressure treatment doesn’t have any clinically significant difference in their magnetic resonance imaging Biomarkers. Thus, controlling high blood pressure doesn’t interpret as controlling Alzheimer’s disease.
Non-genetic Risk Factors of Alzheimer’s
In addition to aging and genetic predisposition, other health and environmental factors play a role in Alzheimer’s disease risk:
- Previous craniocerebral trauma
- Metabolic diseases
- Insulin resistance and hyperinsulinemia
- Diabetes
- High cholesterol levels
- Diseases of the cardiovascular system like heart disease
- High blood pressure
- Stroke
Individuals who are in good physical health and engage in physical activity have a smaller likelihood developing the condition.
Mild cognitive impairment (MCI) is a different disease in which patients experience a slight but noticeable decline in cognitive abilities, including memory and thinking skills. A person with MCI is at an increased risk of dementia.
Epidemiology
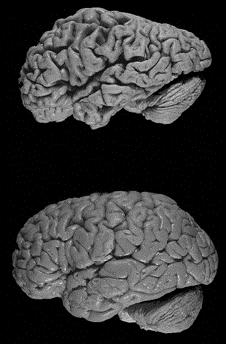
According to the Alzheimer’s Association, there were around 5.8 million individuals living with Alzheimer’s disease in the United States in 2019, 97% of whom are age 65 or older. The association based this number on clinical diagnostic criteria. However, experts acknowledge that the disease begins many years before the onset of symptoms, through biological changes in the brain that control memory and cognition.
Women are significantly more likely to develop Alzheimer’s than men. One reason is their higher life expectancy. Moreover, recent research has revealed connections between fluctuations in hormone levels during menopause and the risk of developing Alzheimer’s.
The disease also has a higher prevalence in minorities compared with whites. Experts believe a higher risk for health conditions, such as cardiovascular disease and diabetes, which are associated with an increased risk for Alzheimer’s and other dementias, may account for these differences.
In 2017, doctors diagnosed 37,000 commercially insured Americans between the ages of 30-64 with early onset Alzheimer’s disease, which occurs in persons of a younger age than expected.
According to estimates by Alzheimer’s Disease International, approximately 46.8 million people worldwide were affected by dementia in 2015. According to the evaluation of computer models, experts believe this number (based on population projections by the United Nations) will increase to around 131.5 million patients by 2050.
Characteristics and Symptoms
Doctor’s characterize Alzheimer’s by an increasing deterioration in cognitive performance, usually accompanied by a decrease in the ability to cope with the activities of daily life, with increasing behavioral abnormalities and an increase in neuropsychiatric symptoms. Symptoms of Alzheimer’s such as memory loss may be mild early in the disease but often become more pronounced with late stage Alzheimer’s, with individuals losing the ability to carry on a conversation and respond to their environment.
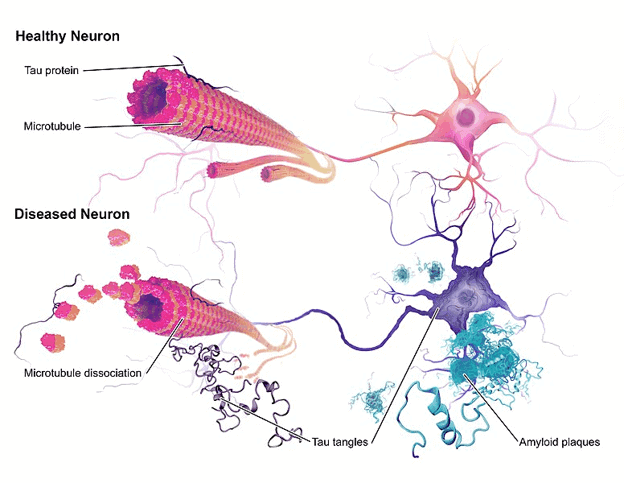
Many years before the first clinical symptoms become visible, plaques and tangles consisting of misfolded beta-amyloid (Aβ) peptides form in parts of the brain. Amyloid plaques and neurofibrils, which are deposited in the neurons in the form of balls, are characteristic of the disease.
The disease belongs to the tauopathies since in this neurodegenerative disease, defective tau proteins attach themselves from the neuron (brain cell) body to the neuron axons, incapacitating the cells. As the disease progresses, brain cells die and cells lose connections among themselves, causing cognitive difficulties to worsen.
Alzheimer’s is not a normal part of aging. The first symptoms of Alzheimer’s vary among affected people. Memory problems are usually one of the first noticeable signs of Alzheimer’s. Mild cognitive impairment may also be an early symptom.
As the disease progresses, people experience greater memory loss and cognitive declines.
According to the National Institute of Aging, a national center at the National Institutes of Health, people experience several symptoms in various stages: mild (early-stage), moderate (middle stage), and severe (late-stage).
Early stage (mild)
A patient may function independently at the early stage of Alzheimer’s. They may experience some memory lapses, such as misplacing objects or forgetting familiar words. While the symptoms may not be widely apparent, close family and friends may notice them.
- Memory loss
- Poor judgment leading to bad decisions
- Loss of spontaneity and sense of initiative
- Taking longer to complete regular daily tasks
- Repeating questions
- Trouble handling money and paying bills
- Wandering and getting lost
- Losing things or misplacing them in odd places
- Mood and personality changes
- Increased anxiety and/or aggression
Middle stage (moderate)
This type of Alzheimer’s can last for many years. Dementia symptoms are more pronounced, and the person may become confused, frustrated, or angry.
- Increased memory loss and confusion
- Inability to learn new things
- Difficulty with language and problems with reading, writing, and working with numbers
- Difficulty organizing thoughts and thinking logically
- Shortened attention span
- Problems coping with new situations
- Difficulty carrying out multi-step tasks, such as getting dressed
- Problems recognizing family and friends
- Hallucinations, delusions, and paranoia
- Impulsive behavior such as undressing at inappropriate times or places or using vulgar language
- Inappropriate outbursts of anger
- Restlessness, anxiety, agitation, tearfulness, rambling—especially in the late afternoon or evening
- Repetitive statements or movement, random muscle twitches
Late stage (severe)
Individuals lose the ability to respond to their environment, carry out a conversation, and, eventually, to control movement. The individual normally has difficulty communicating and carrying out daily activities.
- Inability to communicate
- Weight loss
- Seizures
- Skin infections
- Difficulty swallowing
- Groaning, moaning, or grunting
- Increased sleeping
- Loss of bowel and bladder control
Diagnosis
Doctors often diagnose the condition during the mild or early-stage of the disease. There is no single test for Alzheimer’s disease. Physicians use a variety of approaches and tools to make a diagnosis. Some of the most common diagnostic methods include:
- Medical and family history, including psychiatric history and history of cognitive and behavioral changes
- A family member’s account of thinking and behavioral changes
- Cognitive tests and physical and neurologic examinations
- Blood tests and brain imaging to rule out other causes
- Brain imaging to assess levels of beta-amyloid, a hallmark of Alzheimer’s
Treatment
There is currently no cure for Alzheimer’s. Some medications can treat the symptoms of the disease.
The U.S. Food and Drug Administration (FDA) has approved two types of medications for persons with Alzheimer’s: cholinesterase inhibitors for early to moderate stage (Aricept®, Exelon®, Razadyne®) and memantine for late stage (Namenda®), to treat the cognitive symptoms (memory loss, confusion, and problems with thinking and reasoning). These medications may help lessen or stabilize symptoms for a limited time by affecting certain chemicals involved in carrying messages among the brain’s nerve cells. Sometimes, they are taken together.
For behavioral and personality changes that accompany the disease, such as anxiety, depression, emotional distress, and hallucinations, patients may undergo non-drug treatments that promote physical and emotional comfort. If appropriate and approved by a physician, some medications that can be used include antidepressants, anxiolytics, and antipsychotics. All medications come with a risk of side effects.
In recent years, many novel drugs have been used in clinical trials as possible treatments for early Alzheimer’s disease. However, none have been shown clinically effective. In November 2020, the FDA failed to endorse the newest candidate, Aducanumab. The FDA has not approved a new drug for Alzheimer’s in 17 years.
Prognosis
A common cause of death for people with Alzheimer’s is aspiration pneumonia, which a person develops when they cannot swallow properly and takes food or liquids, instead of air, into the lungs.
Once the disease is diagnosed, the remaining life expectancy is about seven to ten years, although there are cases in which the final stage is reached after only four to five years. On the other hand there have been patients who have lived for more than 20 years. Support groups and care provided by family caregivers and friends is an important component of a positive prognosis in the long term.
If you enjoyed this article, check out our other posts in the Nebula Research Library.
You may be especially interested in these articles on conditions that may accompany Alzheimer’s, such as:
- Depression and other mental illnesses
- Schizophrenia (reality interpretation)
- Alcoholism (an addiction disorder)
- Bipolar disorder (mood disorder driven by mood swings)
May 17, 2022
