Table of contents
Nebula Genomics DNA Report for Psoriasis
Is psoriasis genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Psoriasis?
Psoriasis is a non-contagious chronic disease of the autoimmune system that appears mainly as an inflammatory skin disease (dermatosis). It causes red, scaling skin areas on the knees, elbows, trunk, and scalp, often with severe itching. Other affected parts of your body include the legs, soles of the feet, scalp, face, and palms. Mild to moderate cases occur when patches cover less than 10 percent of the body, while moderate to severe psoriasis covers more than 10 percent.
It occurs when the immune system, designed to remove foreign invaders, attacks the body’s healthy cells.

It is a systemic disease that primarily affects the joints and associated ligaments and adjacent soft tissues, eyes, vascular system, the heart, metabolic syndrome and is also linked to depression. In addition, experts have associated it with diabetes mellitus and strokes.
The condition is a common, long-term disease with no cure. However, there are treatments to help manage symptoms. The condition tends to go through cycles. That is, people with psoriasis will notice a flare-up for a few weeks or months, then the symptoms will subside for a while or go into remission.
Types
There are several types of psoriasis including:
Plaque psoriasis: This is the most common type of psoriasis. It causes dry, raised, red skin patches covered with silvery scales named plaques. These plaques might be itchy or tender and usually appear on elbows, knees, lower back, and scalp.
Nail psoriasis: This form affects fingernails and toenails, causing pitting and abnormal growth and discoloration. Severe cases may cause enough damage that breaks apart the nail.
Guttate psoriasis: Usually triggered by a bacterial infection such as strep throat, it causes numerous small, drop-shaped, scaling skin lesions on the trunk, arms, or legs. This type is more common in young adults and children.
Inverse psoriasis: Usually fungal infections trigger psoriasis of this type, which mainly affects the skin folds of the groin, buttocks, and breasts. Unlike other forms, the patches are red and smooth and worsen with friction and sweating.
Pustular psoriasis: This is a rare form of psoriasis that produces clearly defined pus-filled lesions in widespread patches (generalized pustular psoriasis) or small areas on the palms of the hands or feet soles.
Erythrodermic psoriasis: This is the least common psoriasis type. It covers the entire body with a red, peeling rash that can intensely itch or burn.
Psoriatic arthritis (PsA): Psoriatic arthritis causes swollen, painful joints typical of arthritis. Sometimes the symptoms of this type of arthritis are the only ones of the larger disease and patients do not experience the red, scaly patches. Other times, people with PsA see changes to their nails, as in nail psoriasis.

Other information
Symptoms range from mild to severe. The condition can cause joint pain, stiffness, and swelling and progressive joint damage.
Rheumatoid arthritis (RA) is a similar but distinct disease. Whereas RA is an immune response against the tissues lining the joints, PsA occurs when the immune system attacks both the joints and the skin.
Is Psoriasis Genetic?
Scientists do not know the exact cause of psoriasis, and an individual can develop the condition even if they have no family history. Experts largely believe it is a combination of environmental triggers affecting the immune response and genetic factors play a role in increasing your risk of psoriasis.
So, is psoriasis hereditary? Yes, it tends to run in families. If one parent has the condition, there is about a 10 percent chance of a person developing psoriasis. If both parents have psoriasis, the risk raises to about 50 percent.
Overall, about one-third of patients diagnosed have a family member with the disease.
Scientists do not fully understand the link between specific genetic mutations and the occurrence of psoriasis. Early research suggested that a single gene, human leukocyte antigen (HLA-Cw6), contributed to the disease, but later studies found that this gene alone was insufficient. Experts now largely believe that a complex mechanism of multiple genes and immune triggers causes the condition. Currently, about 25 different genes are associated with it.
Current Research on Psoriasis
Given the number of people who live with the condition, it is no surprise that ongoing research fills up a catalog of almost 400 studies in ClinicalTrials.gov. These studies include research on psoriasis, psoriatic arthritis, psoriatic arthropathy, and arthritic psoriasis.
If you want to learn more about the genetic basis of psoriasis, this 2017 study deepens into genes that play a role.
Some studies like this one by several universities from France, UK, and Egypt, assess the effects of non-antistreptococcal interventions for a form of psoriasis known as guttate psoriasis. Another study from that same year (2019) studies the risk of cancer cases and mortality in patients with psoriasis.
A 2019 paper contemplated the effectiveness of indoor saltwater baths and artificial ultraviolet light on patients with chronic plaque psoriasis. Studies on the genetics of psoriasis are also on the rise. This 2018 study delves into the “genetic polymorphism associated with psoriasis and development of psoriatic arthritis.”
For more resources on psoriasis causes and treatment, you should visit the American Academy of Dermatology.
Epidemiology
According to the National Psoriasis Foundation, psoriatic arthritis and psoriasis affected more than 8 million people in the United States and 125 million people worldwide in 2020. About 30 percent of those with psoriasis also develop psoriatic arthritis.
Psoriasis diagnosis is higher in Caucasians (3.6 percent) compared with African Americans (1.9 percent). However, this is likely an underdiagnosis due to the condition being more easily recognizable on lighter skin.
The condition can develop at any age, but onsets are most likely to occur between 20-30 and between 50-60. Likewise, psoriatic arthritis may also occur at any age but is most prevalent between the ages of 30-50.
Symptoms
Signs and symptoms of psoriasis vary from person to person. It can be as mild as a few spots or as severe as covering most of the skin. You can usually see the hallmark symptoms through physical inspection of psoriasis, including:
- Red patches of skin covered with thick, silvery scales
- Small scaling spots (more common in children)
- Dry, cracked skin
- Itching, burning, or soreness
- Thickened, pitted, or ridged nails
- Swollen and stiff joints (a sign of the autoimmune disease)
Causes
Is psoriasis an autoimmune disease? Yes. The condition occurs when white blood cells in the immune system mistakenly attack the body’s skin cells. The influx of white blood cells signals to the skin cells that there is some type of infection, causing the skin cells to mass-produce.
Since there is no active infection, there become too many cells at the site, and excess skin cells pile up on the skin’s surface.
The pile-up of cells is what patients observe as plaques. The overactive immune response also causes the areas to appear red, inflamed, and itchy.
Environmental factors increase a person’s chance of developing psoriasis. Common psoriasis triggers include stress, illness (particularly strep infections), injury to the skin, and certain medications.
Diagnosis
Usually, doctors can easily diagnose cases of the condition through physical examination by a specialist known as a dermatologist. This health care provider will examine the location, distribution, size, shape, and appearance of lesions. Other important information includes when the lesions started, whether they are itchy or painful, and whether you have painful or swollen joints. They will also ask whether you have a family history of the disease.
Sometimes, psoriasis can prevent itself in a similar way to other conditions such as eczema or lupus. In these cases, your dermatologist may recommend a skin biopsy to confirm psoriasis or rule out these other conditions. A skin biopsy is normally a minimally invasive procedure.
The dermatologist uses a thin device the size and shape of a pencil to puncture the skin and remove a small tissue sample. They close the incision with one or two stitches. A specialist views the sample under the microscope, and the morphology can tell which condition is causing the response.
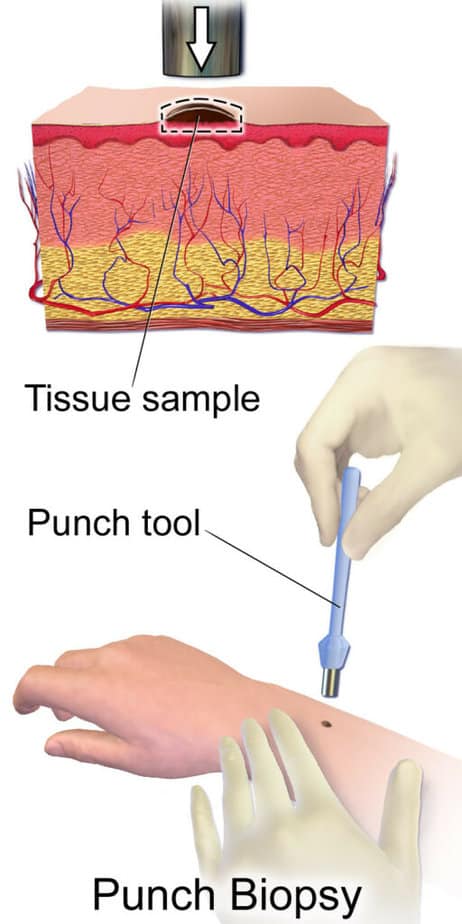
Results of a skin biopsy usually take about a week.
Treatment
Options for the treatment of psoriasis will depend on how the condition presents itself. Treatment options are often based on how severe the condition is and where it appears on the skin. If only the plaque needs treatment, topical ointments are usually the first line of recommended therapy. If other symptoms, such as joint pain, are involved, the patient may need additional medication.
It’s important to note that even with treatment, there is a high chance the condition will return after a period of remission.
Topical treatments
Whether or not your form of psoriasis is genetic, most patients respond well to topical ointments and creams.
Steroid creams: Doctors usually prescribe these drugs for treating mild to moderate psoriasis. They generally recommend mild ointments for sensitive areas, such as your face or skin folds, and treat widespread patches. Topical corticosteroids can be applied as often as once a day during psoriasis flares or more sporadically during remission.
Stronger ointments are available for small, less-sensitive areas or plaques that are tougher to treat.
It’s important to consult with your doctor as this treatment may eventually stop working. Long-term use or overuse of strong corticosteroids are also known to thin the skin. As an alternative, your doctor may ask you to use an over-the-counter moisturizer to hydrate dry skin and provide some relief.
Other types
Anthralin: This tar product is a cream used to slow skin cell growth. It can also remove scales and make skin smoother. Anthralin should not be used on the face or genitals, and it can irritate the skin. It also stains almost anything it touches.
Usually, a patient will apply the cream to the affected area for a short time and then wash it off.
Vitamin D3 ointment: Synthetic forms of vitamin D slow skin cell growth. Sometimes it is prescribed alone or with topical corticosteroids. It is often used as a substitute for sensitive areas as it causes less irritation.
Retinoids: This medication is available as a gel and cream and applied once or twice daily. The most common side effects are skin irritation and increased sensitivity to light.
This product may cause congenital issues and is therefore not recommended if you’re pregnant or breastfeeding or intend to become pregnant.
Salicylic acid: Salicylic acid is a component of some medicated shampoos and bath solutions. Their purpose is to reduce the scaling of scalp psoriasis. It may be used alone or to enhance the ability of other medications to more easily penetrate the skin.
Light therapy
When medication is not effective, your doctor may prescribe additional therapies:
Light therapy: Exposure of the affected area to UVB light at certain wavelengths decreases skin inflammation and helps slow skin cell production. UVB therapy is usually applied two to three times a week until the condition improves and then less often to remain in remission. Short-term side effects might include redness, itching, and dry skin. Your doctor may prescribe a moisturizer to help with the discomfort.
Psoralen plus ultraviolet A (PUVA): This is a combination of light- and medicine-based treatment. It involves taking a light-sensitizing medication (psoralen) before exposure to UVA light. The combination of the deeper penetrating light source (UVA) and the medication will result in more effective treatment. It is often used for more severe cases of psoriasis.
You may experience nausea, headache, burning, and itching. Long-term side effects include dry and wrinkled skin, freckles, increased sun sensitivity, and increased risk of skin cancer, including melanoma.
Additional medications
Methotrexate: This oral anti-inflammatory medication decreases the production of skin cells and suppresses inflammation. It is sometimes recommended for severe cases but may cause liver damage.
Men and women should stop taking methotrexate at least three months before attempting to conceive. This drug is not recommended when you’re breastfeeding.
Cyclosporine: This is another medication that can help severe psoriasis. However, it may also cause high blood pressure and kidney damage.
Some early research suggests an association between psoriasis and celiac disease. In the latter condition, the autoimmune system attacks the lining of the small intestine. Because of this connection, some doctors may suggest a gluten free diet to help manage psoriasis, as well as celiac disease.
For more resources on causes and treatment, you should visit the American Academy of Dermatology.
If you liked this article on whether psoriasis is genetic, you should check out our other posts in the Nebula Research Library, including those on other autoimmune disorders such as Addison’s disease, rheumatoid arthritis, MS, and lupus.
August 3, 2022
