Table of contents
Nebula Genomics DNA Report for Lupus
Is lupus genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

What is Lupus?
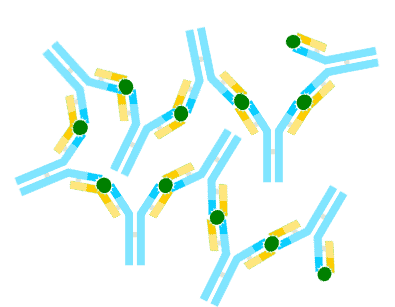
Lupus is an autoimmune disease. In healthy people, proteins called antibodies protect the body by attacking foreign invaders. When a person has this condition, the antibodies cannot tell the difference between foreign material and healthy cells.
Thus, the immune system attacks healthy tissue. In this case, autoantibodies cause pain, inflammation, and damage in multiple parts of the body. The most common areas affected are skin, joints, and internal organs like the kidneys and heart.
Forms of Lupus
The disease can occur in various forms. The types of lupus are:
- Systemic lupus erythematosus (SLE) – a rheumatic disease in the collagenosis group and can affect all organs
- Cutaneous lupus erythematosus (CLE) – this form of lupus is a dermatologic condition that usually only affects the skin. Although the rashes do not normally hurt or itch, they may become discolored. The affected areas can also be photosensitive.
Discoid lupus – appears as a skin rash consisting of disk-shaped, round lesions. The sores usually appear on the scalp and face as red, scaly, and thick lesions.
Subacute cutaneous lupus – lesions may develop as areas of red scaly skin with distinct edges or as red, ring-shaped. They usually occur on the sun-exposed areas of the arms, shoulders, neck, and body.
Acute cutaneous – a malar rash–flattened areas of red skin on the face that resemble a sunburn. It usually appears as a “butterfly rash” on the cheeks and nose, although it may appear on other areas as well.
- Neonatal lupus erythematosus – occurs in newborns born to mothers with lupus
- Drug-induced lupus – a lupus-like disease caused by certain prescription drugs
You can learn more about the different types at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (a section of the National Institutes of Health).
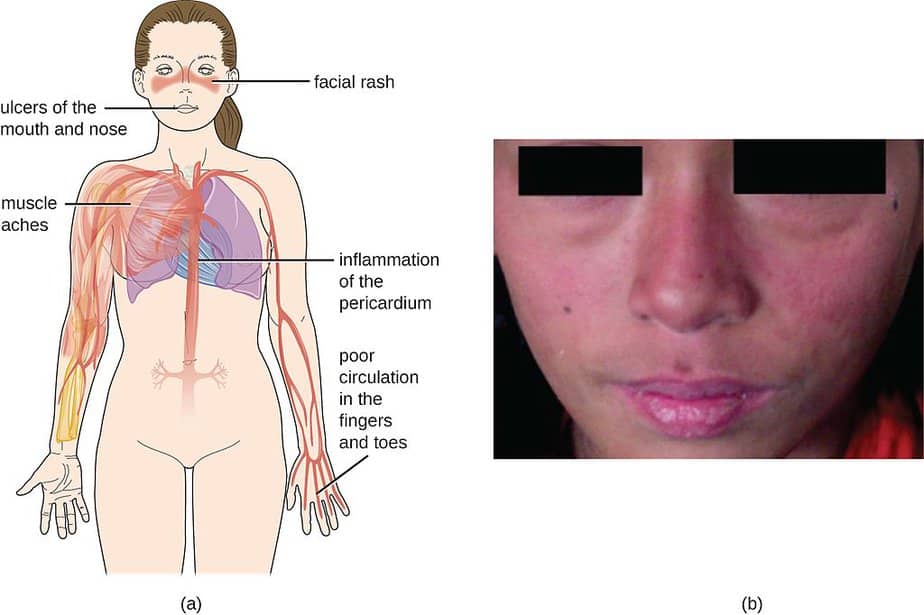
People with lupus may have a family history of the disease or other immune disorders, a reason why people believe lupus is genetic, or heritable. The condition usually progresses in relapses. Between relapses, there may be long phases in which the disease is not active or only slightly active. Particularly characteristic of lupus is butterfly erythema, a redness that extends symmetrically from the bridge of the nose to the zygomatic and cheek regions.
Is Lupus Genetic?
It is not a single gene that causes the condition. Instead, gene mutations in many genes can affect the risk of developing lupus. In most cases experts believe multiple genetic factors are involved. Most of the genetic variants associated with lupus relate to immune system function, and these genes likely affect proper targeting and control of the immune response.
Experts have linked several genetic variations to lupus including IRF5, NCF2, PTPN22, STAT4, and TREX1.
IRF5: Produces a protein that acts as a transcription factor to regulate certain genes’ activities that produce interferons and other cytokines. Cytokines promote inflammation and control other parts of the immune system when an infection is present. They also stimulate the activity of certain immune cells called natural killer cells.
NCF2: Produces a subunit of a protein that helps regulate the immune system, namely immune cells called phagocytes that catch and destroy foreign invaders. This protein also plays a role in regulating neutrophils, which adjust the body’s inflammatory response to injury.
PTPN22: Creates PTP proteins that regulate signal transduction, a process that relays messages from outside of the cell to the cell nucleus. They are involved in signaling that helps regulate immune cells called T cells, which identify foreign substances and helps protect the body from infection.
STAT4: Like IRF5, this gene produces a transcription factor. When activated, this protein enhances the activity of genes that help immune cells called T-cells mature into specialized T-cells.
TREX1: Produces an enzyme that trims molecules of DNA (DNA exonuclease). It removes unneeded DNA fragments created during replication.
Current Research on Genetic Lupus
Lupus is not curable, but doctors can treat it with medication. There is ongoing medical research, many of it cataloged in this PubMed curation of tens of thousand studies of the disease. After a decade of having only one treatment approved in half a century, 2020 saw a rebirth of investigation on the condition.
This resulted in the approval of therapies to treat lupus nephritis (a severe kidney complication), most recently Voclosporin. After two years of a controlled trial of intravenous Belimumab, results showed that patients who received it had a primary efficacy renal response.
To better understand the relationship between genes and lupus, we need to find the genetic markers that predispose it. This “Genome-wide association study meta-analysis identifies five new loci for systemic lupus erythematosus” is a positive path in that direction. Scientists perform this type of genetic lupus research in the hopes of preventing the disease from developing in the first place.
A 2019 article in Science Magazine reported that doctors used a treatment known to have successfully treated certain leukemias (blood cancer) in children and lymphomas in adults to wipe out the condition in mice. This therapy is known as chimeric antigen receptor (CAR)-T and was applied to 26 mice whose spleens, skin, kidneys, and other body parts recovered from lupus.
Epidemiology
The condition can affect people of all ages, including children. However, women of childbearing age (15 to 44 years) are at higher risk than the general population. In fact, 9 out of 10 people with lupus are women. Overall, women are generally ten times more likely than men to develop lupus.
According to the Lupus Foundation of America, lupus affects an estimated 1.5 million Americans and at least five million people worldwide.
Recent national estimates of prevalence and incidence are not available for systemic lupus. Experts attribute lack of data to the fact that SLE is relatively uncommon, is difficult to diagnose, and is not a reportable disease. No recent studies determine SLE prevalence or incidence behavior over time.
A conservative estimate from 2008 suggests a prevalence of 161,000 with definite SLE and 322,000 with definite or probable SLE.
Certain ethnic groups, including African American, Asian/Pacific Islander, and Hispanic populations, are more susceptible to developing lupus and at higher risk of developing more severe symptoms. The condition also appears to be more prevalent in Native American populations, with earlier ages of onset, higher rates of autoantibodies, and different clinical patterns than other populations.
According to the CDC and National Center for Health Statistics, doctors identified SLE as the underlying cause of death for an average of 1,176 deaths per year from 2010–2016.
Characteristics and Symptoms
Characteristics
The symptoms of lupus are different for each individual. They may come on suddenly or gradually and range from mild to severe. Many people experience episodes, or flares, in which symptoms grow worse for a time before improving or even disappearing.
Symptoms
The characteristics depend on which parts of the body the disease is affecting. Some of the most common symptoms include:
- Fatigue
- Fever
- Joint pain, stiffness, and swelling
- Facial butterfly-shaped rash covering the cheeks and nose bridge
- General body rashes
- Photosensitivity: Skin lesions that worsen with sun exposure
- Raynaud’s phenomenon: white or blue fingers and toes when exposed to cold temperature or stressful situations
- Breath shortness
- Chest pain
- Dry eyes
- Headaches
- Confusion
- Memory loss
Causes
Both genetic and environmental triggers cause lupus.
In the lupus erythematosus forms, it dysregulates the normal immune system. It is permanently activated and persistently produces an increased number of antibodies against the body’s own cell nuclear components, so-called antinuclear antibodies (ANA). These autoantibodies damage the body’s own cells.
As cells die, they release their nuclear components. The immune system reacts to the cell nuclear components of healthy endogenous cells that are falsely recognized as foreign. Then, activation of the endogenous immune system and production of more antinuclear antibodies occurs. The activation of the immune system triggers an inflammatory reaction, causing additional body tissue damage.
Immune complexes form from cell nuclear components and autoantibodies in ways that increase arteriosclerosis and lead to vasoconstriction or vascular occlusion. Now, organs or organ systems do not have an adequate blood supply and are susceptible to additional damage. Inflammatory reactions caused by the deposition of immune complexes on the blood vessel walls can also occur.
The exact cause of this pathological reaction of the immune system is as yet unknown. However, it is assumed, among other things, that an increased interferon activity of type I interferon plays an important role.
Cutaneous lupus erythematosus only affects the skin. However, CLE can progress into systemic lupus.
Triggers
According to Mayo Clinic, doctors suspect that people with a genetic predisposition develop lupus when they experience an environmental factor that triggers it. Potential triggers include:
- Sunlight – exposure to the sun may bring on skin lesions or trigger an internal response in susceptible people
- Infections – having an infection can initiate the condition or cause a relapse in some people
- Medications – These include several types of blood pressure medications, anti-seizure medications, and antibiotics. People with drug-induced lupus tend to get better when they suspend the medication. Rarely, symptoms may persist even after drug use stops. Experts believe about 10 percent of SLE cases are triggered by drug exposure and more than 80 drugs may be involved
Diagnosis
A health care professional will usually first check for signs of inflammation, including heat, pain, swelling, redness, and loss of function at a particular place in the body. Diagnosis is difficult since the symptoms mimic those of many other diseases. The most distinctive sign of lupus – a facial rash that resembles butterfly wings unfolding across both cheeks – occurs in many but not all cases of lupus.
Did you know you can test inflammation markers at home? Learn more in our article about at home inflammation tests.
According to the Lupus Foundation of America, diagnosis will include the following review with a physician:
- Current symptoms
- Laboratory test results
- Medical history
- Medical history of your close family members (grandparents, parents, brothers and sisters, aunts, uncles, cousins)
Doctors can use a variety of laboratory and blood tests to help diagnosis, but no single test can give a definitive answer. The most common lab test associated with lupus is called the antinuclear antibody (ANA) test. This test detects antinuclear antibodies (antibodies that attack cellular nuclei) in the blood.
A problem is that the ANA test is not specifically for lupus. It is also used to diagnose rheumatoid arthritis, Scleroderma (a rare disease affecting the skin, joints, and blood vessels), and Sjogren’s syndrome (another rare condition affecting the body’s moisture-making glands).

Often, patients may need to consult a professional rheumatologist. They can obtain a more confident diagnosis, provide medical advice, and prescribe a treatment plan.
Treatment
While there is no cure for lupus, diagnosis and treatments can be used to prevent flares, treat symptoms, and reduce organ damage. The potential medicines prescribed are used to reduce pain and swelling, calm the immune system, reduce or prevent joint damage, and/or reduce or prevent organ damage.
Some medicines to help patients cope with lupus and improve quality of life include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – over-the-counter NSAIDs, such as naproxen and ibuprofen, help reduce mild pain and swelling in muscles and joints
- Corticosteroids – these medicines reduce swelling, tenderness, and pain. In high doses, they can calm the immune system
- Antimalarial drugs – these will treat joint pain, skin rashes, fatigue, and lung inflammation. Two common antimalarial medicines are hydroxychloroquine (Plaquenil) and chloroquine phosphate (Aralen)
- BLyS-specific inhibitors – these drugs limit the number of abnormal B cells (cells in the immune system that create antibodies) found in people with lupus. A common type of BLyS-specific inhibitor that treats lupus symptoms, belimumab, blocks the action of a specific protein in the body that is important in immune response
- Immunosuppressive agents/chemotherapy. These medicines may be used in severe cases of lupus, when it affects major organs and other treatments do not work
- Other medicines. Many people with lupus are also at risk for high blood pressure and blood clots, which can cause a stroke or heart attack. Your doctor may prescribe anticoagulants, or blood thinners, such as warfarin or heparin, to prevent your blood from clotting too easily
Did you like this article? You can read more in our Nebula Research Library, including those on other autoimmune disorders such as Addison’s disease, rheumatoid arthritis, MS, and psoriasis.
June 23, 2022
