Table of contents
Nebula Genomics DNA Report for Schizophrenia
Is schizophrenia genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of April 2021. |
What is Schizophrenia?
The term schizophrenia refers to a severe mental illness or psychotic disorder with symptoms similar to psychoses, where the patient abnormally interprets reality. Doctors generally consider it an abnormality in brain development and poses genetic and environmental risks of developing other conditions such as autism.
In the acute stage of the disease, a schizophrenic person suffers from various characteristic disorders that affect almost all areas of experience and behavior. This includes perception, thinking, emotional and emotional life, will formation, psychomotor skills, and drive.
Often, patients hear voices that are not present. Additionally, they can have delusions of being followed, spied on, or controlled. Persistent hallucinations of any sensory modality are also possible.
A person with schizophrenia will often display characteristics that appear as social withdrawal, lack of drive, lack of motivation, emotional flattening, and joylessness. Depending on the prevailing symptoms, doctors distinguish several subgroups.
It’s important to note that schizophrenia and split personality disorder are not the same. The former does not associate with multiple personalities as the latter does. The condition is also distinct from bipolar disorder, a different mental illness that causes extreme mood shifts.
In many cases, the symptoms disappear after the initial phase of the disease. Thereafter, further phases of the disease relapses or psychotic episodes may follow at irregular intervals.
In about one-third of the patients, all symptoms disappear entirely after a certain point. Another third have recurrences occur repeatedly. In the last third, the course of the disease becomes chronic, leading to a permanent mental disability.
Is Schizophrenia a Genetic Disorder?
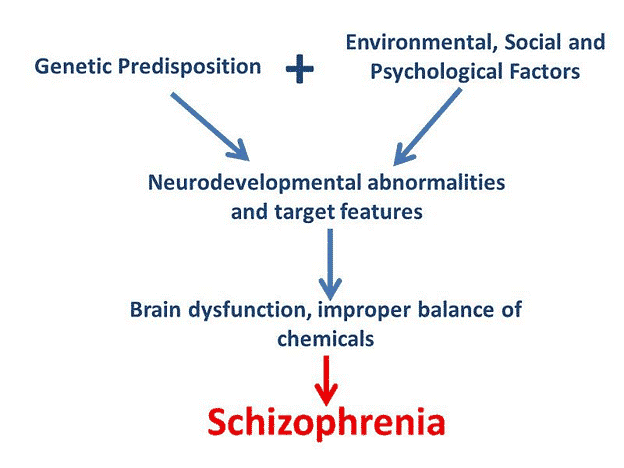
Research suggests that genes play a role in the risk factor of developing schizophrenia. However, there is no single “schizophrenia gene.” Instead, experts believe many genes each have a small effect. A small percentage of patients living with schizophrenia appear to have a small deletion (microdeletion) in a region of chromosome 22, known as 22q11.
As such, most generally consider that a combination of genetic and environmental factors lead to schizophrenia.
Experts know that having a family member with or family history of schizophrenia increases the chance of developing the disorder. In the case of a schizophrenic parent, it is five to ten percent likely that a child will develop it. For siblings, it is eight to ten percent. In the case of identical twins 45 percent, and about 21 percent in the case of fraternal twins.
However, in the context of the gene-environment interaction, for example, birth complications such as lack of oxygen, infection, or stress on the mother, increase the risk of developing schizophrenia. Patients with schizophrenia tend to have immune system defects. Biographical, psychological, and social factors can also be significantly responsible for the development of schizophrenia if genetic vulnerability is present.
Current Research on Genetic Schizophrenia
The National Center for Biotechnology Information has a thorough resource through the Genetic Testing Registry with reports on clinical and research tests for the condition. It includes a section test for all associated and related genes.
The U.S. National Library of Medicine has a catalogue of more than 3000 studies on schizophrenia, including some currently happening and expected to report results within a year or two.
This catalogue from Omim includes a phenotype-gene relationships table with details on the location of genes associated with the condition.
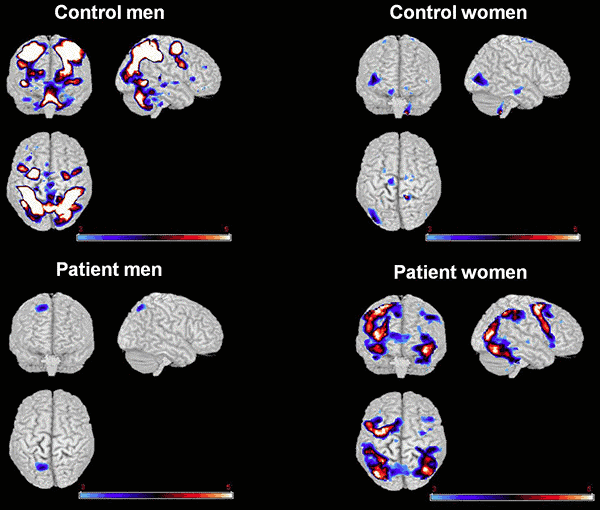
There is no doubt that this condition has earned a number of studies to understand it and better study the effect of genetic variation on function and structure of the brain. This 2018 abstract from PubMed gives a description of imaging genetics for the study of schizophrenia.
If you are interested in updated information and clinical implications related to the genetics of antipsychotic treatment, take a look at this publication from Karger. This study showed details from clinical trials of Lumatoperone for the treatment of schizophrenia.
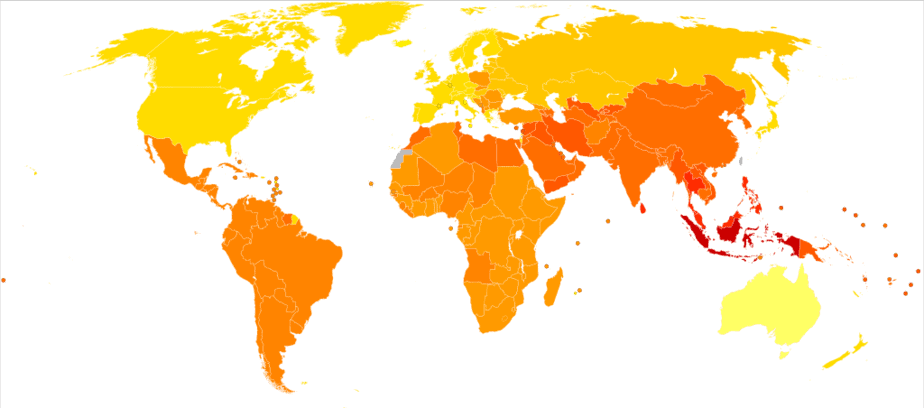
Epidemiology
As of 2019, schizophrenia affects 20 million people worldwide. It is not as common as other mental health conditions. People with schizophrenia are 2 – 3 times more likely to die early than the general population due to physical illnesses, such as cardiovascular, metabolic, and infectious diseases.
The risk of developing the disorder is the same for men and women, although usually schizophrenia affects men at a slightly earlier age. Men may exhibit symptoms in the early to mid-20s, while women’s symptoms typically begin in the late 20s. It’s uncommon for doctors to diagnose children with the condition and it is rare for those older than age 45.
Symptoms
Doctors traditionally divide the symptoms of schizophrenia into two broad areas: Positive and negative. Recently, the cognitive symptoms of the disorder have also received increasing attention and are seen as a separate third area.
According to Mayo Clinic, signs and symptoms may vary among individuals but usually include delusions, hallucinations, or disorganized speech and reflect an impaired ability to function. Thinking can become short-stepped, and the patient can no longer understand multilayered relationships in their complexity. Linguistic expression becomes impoverished.
The severity of the symptoms depends in part on the personality of the person affected. Although the symptoms vary greatly between individuals, the individual patients often retain their unique pattern of symptoms for long periods. Once doctors diagnose a person with schizophrenia, they can explore treatment options such as prescription antipsychotic medications or attend support groups. Experts will constantly monitor patients for relapses and long-term side effects.
Positive symptoms
Positive symptoms refer to exaggerations of the day to day experience and are therefore seen as a kind of “excess” of the healthy state. These include severe misconceptions of the experienced reality, such as hallucinations and loss of reality. Schizophrenia with predominantly positive symptoms often begins suddenly, and there are usually no outwardly noticeable features before the onset of the condition. The course of the disease is rather favorable.
There are various positive symptoms of schizophrenia, including:
- Delusions. False beliefs that are not based on reality. For example, you think that you’re being harmed or harassed, another person is in love with you, or a major catastrophe is about to occur. Delusions are one of the most common symptoms in people with schizophrenia.
- Hallucinations. Seeing or hearing things that don’t exist. While hallucinations can be in any of the five senses, hearing voices is the most common one.
- Disorganized thinking (speech). Speech becomes sloppy. Individuals have impaired communication and answers to questions may be partially or completely unrelated.
- Highly disorganized or abnormal motor behavior. These symptoms vary from childlike foolishness to unpredictable agitation. It’s hard for individuals to do tasks. Behavior can include resistance to follow instructions, inappropriate or bizarre aspects, a complete lack of response, or useless and excessive movement.
Negative symptoms
Negative symptoms refer to limitations in everyday experience and mental functions previously present but that have been reduced or are completely absent due to the disease. These symptoms, therefore, represent a deficiency compared to the healthy state.
For example, the person may overlook personal hygiene or appear emotionless (no eye contact, unfazed, or speaks in a monotone). The person may lose interest in everyday activities, keep social distance, or become unable to experience pleasure.
Schizophrenia with pronounced negative symptoms often begins gradually, and the course of the disease can be unfavorable. Early signs are very often sleeping disorders and depressive symptoms. Negative symptoms can occur months or years before the acute psychotic symptoms and usually intensify or harden with increasing duration of the illness.
You can find more information and resources on the National Alliance of Mental Illness’s website.
Causes
Experts have not identified a single cause for schizophrenia. As of 2020, they assume there is an interaction of several triggering factors.
The general explanation for the cause of schizophrenia is currently based on a multifactorial interplay of biological (e.g., genetic, infectious, metabolic) and psychosocial (e.g., social environment, psychological stress in the biography) causes. Accordingly, several of these factors in combination can trigger schizophrenia. Experts consider exceeding a stress threshold as the triggering factor that causes the psychosis to break out in a biologically susceptible (vulnerable) person.
Non-genetic factors
Neurobiology
Imaging techniques demonstrate that the brain shows multiple variations in anatomy and physiology in cases of schizophrenia. Recent research is looking to clarify the connection between certain deviations and the expected course of the disease.
Diagnosis of schizophrenia is also accompanied by biochemical changes in the brain. For example, the signal transmission between nerve cells in the brain deviates from their normal functioning with regard to the neurotransmitter systems that work with dopamine, GABA, or glutamate.
The condition also appears to develop when there is an imbalance of a neurotransmitter called dopamine, and possibly also serotonin, in the brain.
Toxic factors
In general, the use of substances that strongly alter consciousness leads to a higher risk of schizophrenia. However, it also depends on both the genetic disposition and the individual personality. Psychotropic substances such as alcohol, amphetamines, cocaine, and phencyclidine can trigger substance-induced psychoses.
We also know that non-consciousness-altering substances such as steroids can cause psychosis.
Hormonal factors
There has been evidence for many decades that estrogens influence risk and the severity of symptoms. More recently, research has shown that, as an addition to standard drug treatment, selective estrogen receptor modulators, such as raloxifene, can slightly reduce the symptoms of schizophrenia. Both men and women can use these for more extended periods.
Psychosocial factors
Ego developmental deficits or serious neglect in the first years of life can be factors that lead to greater susceptibility to disease, increasing vulnerability. Trauma during birth, malnutrition before birth, viral infections, and additional trauma may also contribute to disease development.
A comprehensive follow-up study found that children of mothers who had described their child as “unwanted” in late pregnancy were more than twice as likely to develop schizophrenia during their lifetime as a control group. According to the authors, the results suggested that either psychosocial stress during pregnancy or a particular tendency in the mother’s general behavior was associated with increased risk.
There is also evidence that people with schizophrenia have a statistically increased incidence of childhood trauma.
For additional information on Schizophrenia treatment, diagnosis, causes, and health care professionals, refer to The National Institute of Mental Health.
Diagnosis
To diagnose schizophrenia, a mental health professional will use the criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
According to the criteria, a person must have at least two of the following symptoms for a month:
- delusions
- hallucinations
- disorganized speech
- crassly disorganized or catatonic behavior
- negative symptoms, such as lack of speech, emotional flatness, or lack of motivation
They must also experience considerable impairment in their ability to function in school or at work, interact with others, or carry out self-care tasks. Symptoms should persist for six months or more.
It can be hard to tell the difference between schizophrenia and a similar condition called schizoaffective disorder. The latter brings on schizophrenia-like symptoms but, doctors characterize it by a detachment from reality rather than altered reality.
Treating Genetic and Non-genetic Schizophrenia
Schizophrenia is a lifelong condition, but various medications can help control symptoms, improve quality of life, and help patients avoid hospitalization. According to Medical News Today, treatment options include:
- Antipsychotic drugs
- risperidone (Risperdal)
- olanzapine (Zyprexa)
- quetiapine (Seroquel)
- ziprasidone (Geodon)
- clozapine (Clozaril)
- haloperidol (Haldol)
- Counseling
- Coordinated special care
In many cases, affected individuals require duel diagnosis treatment, where doctors treat schizophrenia along with common co-occurring addition problems with drugs and alcohol.
Remember that this article is for educational purposes only and not a substitute for medical advice, diagnosis, or treatment.
If you liked this article, you should check out our other posts in the Nebula Research Library, including some on other behavior conditions like Tourettes.
You may be particularly interested in our other schizophrenia articles and those on other mental illnesses such as Alzheimer’s disease and dementia, disorders that affect the brain as we age.
June 21, 2022