Table of contents
Nebula Genomics DNA Report for Bipolar Disorder
Is bipolar disorder genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

To learn more about how Nebula Genomics reports genetic variants in the table above, check out the Nebula Research Library Tutorial.
| This information has been updated to reflect recent scientific research as of April 2021. |
What is Bipolar Disorder?
Bipolar disorder is the established short name for bipolar affective disorder (BAS). It is a mental illness that belongs to mood disorders (affect disorders). Previous names for this condition were manic-depressive illness or manic depression.
Patients manifest the disorder by extreme, bipolar opposite mood swings, drive, and activity levels. These swings occur in phases and extend far beyond normal levels. Those affected oscillate back and forth between depression and mania without being able to control these changes voluntarily. Symptoms usually become apparent gradually.
Doctors characterize depressive episodes by above-average depressed mood, energy, and decreased drive. They characterize a manic episode by increased drive and restlessness, often accompanied by inadequately exuberant or irritable mood. In the process, patients experience severly impaired ability to examine reality.
Depending on the course of the disease, there may be more or less long periods between the acute mood episodes in which the affected person has no symptoms at all. The condition occurs in a wide variety of degrees of severity. Individuals may appear to have a charismatic personality during the manic episode. However, possible negative social consequences of the disorder for the individual can be very severe.
Is Bipolar Disorder a Genetic Disorder?
Scientists published a review of fraternal and identical twin studies published in 2013 which suggests that the disorder can run in families, and estimates the heritability of an increased risk of bipolar disorder at over 80%. The risk of developing bipolar disorder is nearly ten-fold higher when a first-degree family member has the condition than in the general population. This evidence suggests that the answer to the question “is bipolar hereditary?” is positive.
A 2015 review suggested that, to date, scientists have identified a large number of genetic alterations in relation to the disorder. However, each genetic component only contributes very slightly to an increased risk factor. This means that many small genetic variants taken together likely influence a greater predisposition to the disease, but no single gene can be identified as a cause.
Genome-wide associations studies conducted in 2013 and 2014 showed several common single-nucleotide polymorphisms (SNPs) are associated with the disease, including variants within the genes CACNA1C, ODZ4, and NCAN. None of these associations could confirm a sizeable causal effect, helping to establish the belief that a person’s risk of disease results from a combination of genetic and environmental factors.
Out of these genes, CACNA1C is the most widely studied variant in relation to the disorder. It codes for the subunit of a voltage-dependent calcium channel that mediates the influx of calcium ions upon membrane polarization. Researchers have associated mutations in the gene with a disruption in brain connectivity in bipolar disorder patients and have also linked them to schizophrenia.
More recently, in 2016, experts associated two additional polymorphisms in TPH2 with the condition.
Scientists are conducting additional genome-wide association studies to search for more links between specific genes and bipolar disorder.
Current Research on Genetic Bipolar Disorder
There are enough peer reviewed studies to support a positive answer to the question, “Is bipolar disorder hereditary?” Scientists are conducting many studies in an effort to find favorable treatment options. These studies are open for the public to participate. This list from ClinicalTrials.org is a good start.
The National Institutes of Health’s National Institute of Mental Health is investigating whether bipolar disorder is genetic in those affected and their family members. Investigators are also trying to find genes that may increase a person’s chance of developing the condition.
This study from 2017 refers to rapid-cycling bipolar disorder and the biological markers associated with it. Besides genetics, it was trying to find other causes for predisposition.
According to a research paper from 2020, not only is bipolar disorder genetic, but it also shares more than half of its determinants with schizophrenia, as mentioned earlier. Furthermore, the Stanley Neuropathology Consortium conducted research to find disease-specific alterations in frontal cortex brain proteins in schizophrenia, bipolar disorder, and major depressive disorder.
You may be interested in reading this piece on the mental health and lifestyle impacts of COVID-19 on bipolar disorder.
Forms
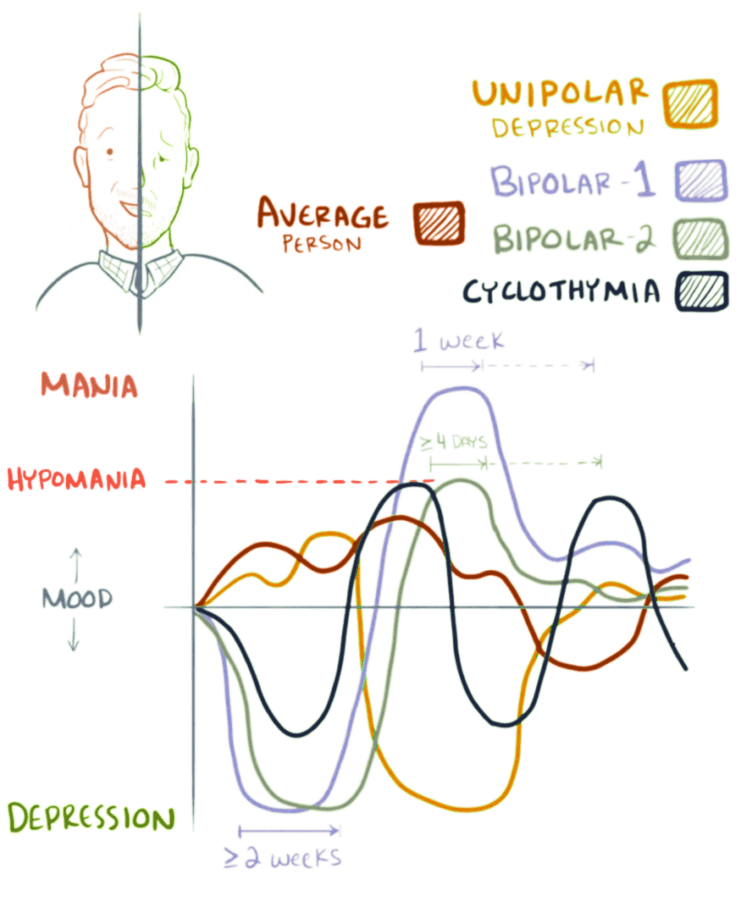
There are three types of bipolar disorder. While they are all characterized by drastic swings in high and low moods, experts distinguish them by the severity of the disease.
Bipolar I disorder: the patient experiences manic episodes for at least seven days or spells that are so life-disrupting that the patient needs immediate hospital care. Depressive episodes usually occur as well, lasting at least two weeks. Having depressive symptoms and manic symptoms at the same time is also possible.
Bipolar II disorder: the patient experiences a sequence of depressive episodes and hypomanic episodes, but not to the extent of the manic episodes of Bipolar I Disorder.
Cyclothymic Disorder: the patient has periods of hypomanic symptoms as well as periods of depressive symptoms, and they must last for at least two years. However, the symptoms do not meet the diagnostic requirements for a hypomanic episode and a depressive episode.
Other Specified and Unspecified Bipolar and Related Disorders: the patient has bipolar symptoms that do not fit into the other categories.
Epidemiology
Based on National Comorbidity Survey Replication (NCS-R) diagnostic interview data, an estimated 2.8% of U.S. adults had bipolar disorder between 2001 – 2003. Prevalence was nearly identical between males and females.
In 2017, the Global Burden of Diseases Study (GBD) estimated 4.5 million new cases in the U.S. and 45.5 new cases worldwide. Bipolar disorders have an annual incidence from 3 to 10 cases per 100,000 population.
Bipolar disorder in children often goes undiagnosed because of its similarity to other conditions, such as ADHD.
Characteristics and Symptoms
Symptoms and severity of bipolar disorder differ among individuals. Patients often suffer distinct episodes of mania and depression. However, sometimes people will go for years without symptoms. On the other hand, a patient can seemingly experience both symptoms simultaneously or in rapid succession.
Mania or hypomania: an elevated mood characterizes mania. Hypomania is a milder form of this effect. Although initial mood elevation may appear good, patients may find that they quickly become more irritable, their behavior more unpredictable, and their judgment more impaired.
Doctors often associate reckless conduct with a manic episode. To be diagnosed, a person must have experienced at least one manic episode.
Depression: In patients with the condition, the depressive state is often very debilitating and can be classified as major bipolar depression. The disorder generally affects sleep (sleeping too much or not sleeping enough). They may become obsessed with feelings associated with clinical depression, including feelings of loss, personal failure, guilt, or helplessness.
Life events such as a death in the family can heighten these symptoms. To be diagnosed, major depressive episodes must last every day for at least two weeks.
Feelings of suicide may occur in either the manic or depressive episodes of this condition. It’s important that if you are feeling suicidal, you contact 911 or a national helpline immediately.
Symptoms may also include psychosis, such as delusions or hallucinations.
Co-morbid conditions
Several conditions tend to co-exist with bipolar disorder. These other mental health disorders can exasperate bipolar symptoms and often lead to a misdiagnosis.
- Psychosis. Sometimes people who have severe episodes of mania or depression also have psychotic symptoms, such as hallucinations or delusions. These symptoms usually match the person’s extreme mood.
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Misuse of Drugs or Alcohol
- Eating Disorders
Causes
Research suggests that a combination of genetic factors and environmental triggers, such as a stressful event, ultimately play a role in the onset of bipolar disorder.
Non-genetic risk factors
Brain physiology
Using neuroimaging, changes in a person’s brain with bipolar disorder include decreased gray matter volume in the prefrontal and temporal cortex, hippocampus (memory functions), and amygdala (emotion responses). Also, doctors observe a decrease in the volume and function of white matter, which connects prefrontal and subcortical (such as amygdala and hippocampus) regions.
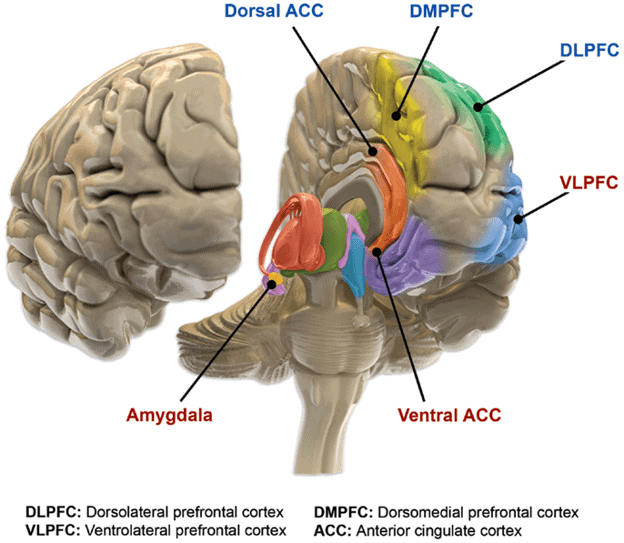
Brain chemistry
Disorders of neurochemical signal transduction mainly affect four of the most important neurotransmitters: the three monoamines-norepinephrine, dopamine, and serotonin- and especially glutamate. Additional variations within neurons in the secondary messengers play a crucial role and are necessary components of the theories of development and progression in bipolar disorder.
Environmental factors
Environmental influences and personality traits also play a decisive role. Doctors believe critical life events, such as trauma or psychosocial stress, trigger the illness, although they do not yet understand individual mechanisms.
Additionally, doctors also discuss weakened self-esteem, an irregular day/night rhythm, or alcohol and other drug abuse as triggering factors.
Diagnosis
Typically, doctors diagnose this condition in late adolescence or early adulthood.
According to the National Institute of Mental Health, experts diagnose the condition through:
- Complete a full physical exam, including family history and medically reviewed health history
- Order medical testing to rule out other illnesses
- Refer the person for an evaluation by a psychiatrist. The mental health professional may use criteria for bipolar disorder and related disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association, to confirm the diagnosis
Some people have bipolar disorder for years before it is diagnosed. This may be because:
- The condition has symptoms in common with several other mental health disorders and can be easily misdiagnosed
- Family and friends may notice the symptoms but not realize that the symptoms are part of a more significant problem
- People with the disorder often have other health conditions, which can make it hard to diagnose bipolar disorder
Treating Genetic and Non-genetic Bipolar Disorder
Although the symptoms may vary over time, the disorder usually requires lifelong treatment targeted at mediating symptoms. Following a prescribed treatment plan can help people manage their symptoms and improve their quality of life.
This website is not intended to diagnose any condition or provide medical advice. If you think you may have a mental disorder, please contact your doctor.
According to Mayo Clinic, treating bipolar disorder may include:
Medications and programs
Medications. These are often the first prescribed treatment and may include mood stabilizers, antipsychotics, antidepressants, antidepressant-antipsychotic, or anti-anxiety drugs. Unfortunately, many of these medications induce side effects. Finding the proper medication for an individual with bipolar disorder that is both effective and safe takes time and is often a process of trial and error
Continued treatment. This condition requires lifelong treatment in the long term with medications, even during periods when you feel better. If a patient skips regular treatment, they may risk a relapse of their symptoms. It may cause minor mood changes that will turn into depression or a full-fledged manic episode,
Day treatment programs. Programs that provide support and counseling, including talk therapy
Substance abuse treatment
Hospitalization. Your doctor may recommend hospitalization if you’re behaving dangerously, you feel suicidal, or you become detached from reality (psychotic)
Psychotherapy
Psychotherapy is a vital part of treatment. It can be conducted as an individual or in a support group or family group. Psychotherapy options include interpersonal and social rhythm therapy (IPSRT), cognitive behavioral therapy (CBT), psychoeducation, or family-focused therapy.
Treatment for bipolar disorder may also include electroconvulsive therapy (ECT) for some patients. In this approach, electrical currents are passed through the brain, intentionally triggering a brief seizure. The procedure seems to cause changes in brain chemistry that can alleviate symptoms. ECT is sometimes recommended to certain patients who find that medications are ineffective or can’t take traditional antidepressants.
It’s important to note that this article is for educational purposes and should not be substituted for medical advice.
Did you enjoy this article? You can check out more posts in the Nebula Research Library, including additional information on other behavior conditions like Tourettes.
You may also be interested in medication reviews for antidepressants like Lexapro and Zoloft.
June 22, 2022