Table of contents
Nebula Genomics DNA Report for Psychosis
Is psychosis genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of May 2021. |
What is Psychosis?
Doctors describe psychosis as an abnormal illness of the mind made up of symptoms, including hallucinations, delusions, loss of contact with reality, or ego disorders. This condition affects a person in that they almost always have an impaired relationship with reality. There may also be incoherent speech, inappropriate behaviors, sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. During a period of psychosis, a person is said to be undergoing a psychotic episode.
These different symptom types can occur individually or in combination. Causes include mental illnesses such as schizophrenia or bipolar disorder, sleep loss, some medical conditions, certain medicines, and drugs such as alcohol or cannabis. A temporary agent can cause a one-off experience of psychosis or it can be part of a long-term mental health condition.
According to the National Institute of Mental Health, the three most common signs of psychosis include hallucinations, delusions, and cognitive experiences or disturbing thoughts.
Hallucinations are seeing, hearing, or feeling things that aren’t there. A person may hear voices, have strange sensations, or see glimpses of objects or people that are not there.
Delusions are strong false beliefs that are not consistent with the person’s culture, are unlikely to be true, and may seem irrational. A person may believe an external force controls them, believe that trivial remarks, events, or objects have personal meaning or significance, or think that they have special powers. There are many other examples of delusions.
Cognitive experiences relate to mental action. People with psychosis may find it difficult to learn, remember, make decisions, or concentrate.
Is Psychosis Genetic?
People are more likely to experience psychosis if a family member, such as a parent or sibling, has the condition. Children born with the genetic mutation known as 22q11.2 deletion syndrome are at risk for developing a psychotic disorder, especially schizophrenia. In most cases, multiple genetic factors, each with a small effect, combine to increase the risk of developing the brain disorder.
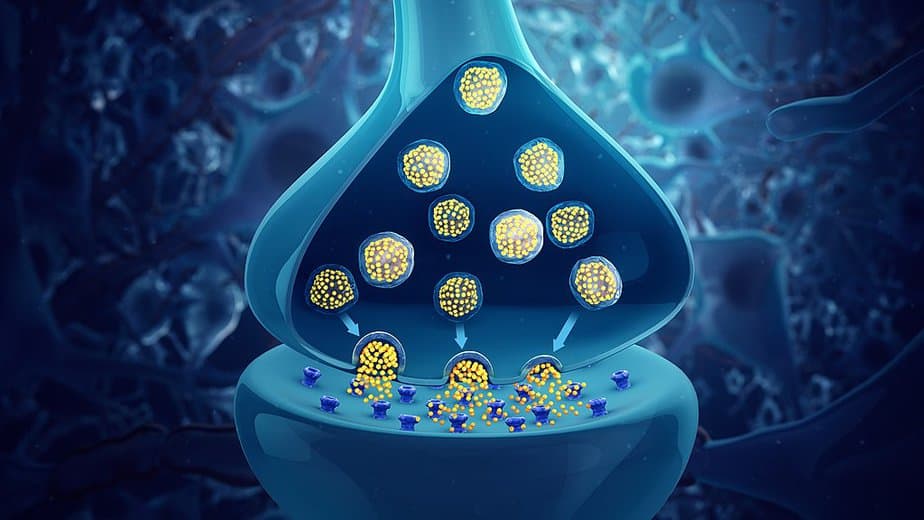
The two most studied forms of psychosis in this genetic regard are schizophrenia and bipolar disorder, both associated with the overproduction of the neurotransmitter dopamine in the brain. Other studies have been conducted that investigate genes related to the functioning of this chemical in the brain.
A 2019 study revealed that a cluster of epigenetic markers, which switch genes on and off, affects a gene called IGF2, which plays a role in synaptic development. The enhancer also regulates dopamine. This revelation could explain why dopamine-based illnesses are often accompanied by a disruption of brain synapses. Thus the genetic field of epigenetics may ultimately contribute to psychosis.
The genetics of schizophrenia and other psychosis conditions are areas of active research. It is most likely that genetic predispositions combined with environmental factors, especially stressors, bring on psychosis episodes.
Current Research on Genetic Psychosis
In 2019, researchers published a paper titled Effects of traumatic life events, cognitive biases, and variation in dopaminergic genes on psychosis proneness. It aimed to test the effects of interactions between variation in dopaminergic genes and traumatic life events (TLEs) on the severity of psychotic‐like experiences (PLEs).
The authors showed that decreased dopamine catabolism related to the catechol‐O‐methyltransferase (COMT) rs4680 genetic polymorphism is associated with and may increase in psychosis in individuals with a history of traumatic life events (TLEs) and high levels of cognitive biases.
Another group published research on Longitudinal trends in childhood insulin levels and body mass index and associations with risks of psychosis and depression in young adults in 2021.
They aimed to examine whether specific genetic developmental trajectories related to body mass in early childhood were associated with the prevalence of psychosis and depression in young adults.
The result seems to agree with this hypothesis. Specifically, disrupted insulin sensitivity (a contributing factor to obesity, heart disease, and diabetes) also appears to increase the condition.
Additionally, the study showed that a major increase in BMI around puberty could increase a young person’s risk of developing depression later in life.
Epidemiology
According to the National Alliance on Mental Illness, 3 in 100 people will have an episode at some point in their life, although this does not mean that they will have a psychotic disorder. Even though in the U.S Approximately 100,000 young people experience psychosis of some type each year, less than 1% of the U.S. population lives with a psychotic disorder.
Women are at a higher risk of the condition after giving birth. Doctors call such psychosis postpartum psychosis, characterized by a severe postnatal mood disorder. A 2021 study revealed that 1 – 2 out of 1000 births result in this type of mental disorder. The condition usually develops during adolescence or early adulthood, with the average age of onset being 24 years.
Causes
There is no single factor that causes a person to develop psychosis. The current belief is that a combination of genetic and environmental factors contributes to the condition. Specifically, any existing predisposition (disposition; genetic or prenatal) interacts with subsequent stress, assumed to be the trigger. Stressors include:
- Pre- and perinatal factors such as maternal stress during pregnancy
- Influences on the immune system (childhood infections),
- Socialization and psychological development of the child
- Anatomical and functional deviations in the structure of the brain and brain cells
- Mechanical impact on the brain (e.g., through craniocerebral trauma or brain tumors),
- Hormonal influences
- Drugs and medicines
- Various somatic diseases (autoimmune/rheumatic, endocrine)
Types of psychosis
Doctors divide the condition into two main categories that separate neurocognitive disorders describing reduced brain function due to illnesses not psychiatric in nature and psychiatric disorders.
Neurocognitive disorders
- Degenerative brain diseases (Alzheimer’s or Lewy Body type dementias, vascular dementia – you can read more about Alzheimer’s disease in our Research Library)
- Brain injuries (craniocerebral trauma)
- Focal processes (epilepsy, stroke)
- Malignant neoplasms (tumors both primarily in the brain and as metastases)
- Infections (meningitis)
- Autoimmune diseases (anti-NMDA receptor encephalitis, Hashimoto’s thyroiditis, lupus erythematosus, multiple sclerosis, vasculitis)
- Endocrine diseases (hypo- and hyperthyroidism, hypo- and hyperparathyroidism)
- Congenital or acquired metabolic disorders (leukodystrophy, lysosomal storage diseases, mucopolysaccharidoses, porphyria)
- Other metabolic disorders (hypo- and hypernatremia, hypoglycemia)
- Poisoning with medicines or drugs, drug withdrawal
- Parasites (neurocysticercosis)
- Special forms like the postpartum psychosis
Psychiatric disorders
- Schizophrenia or diseases of the schizophrenic for
- Persistent delusional disorder
- Acute or temporary psychotic disorders
- Induced delusional disorder
- Schizoaffective disorder
- Affective psychoses (this includes some forms of bipolar disorder or major depression)
Substance-induced psychosis
Another form is substance-induced psychosis that is a psychotic disorder caused by one or more psychotropic substances. Psychotic states can normally be reversible or only temporary. Some categories of these substances include alcohol, amphetamines, benzodiazepines, caffeine, cocaine, and LSD.
Characteristics and Symptoms
According to Healthline, psychosis is a combination of symptoms. In general, the three main symptoms that characterize the condition are hallucinations, delusions, and confused and disturbed thoughts. Some of the specific symptoms of people experiencing psychosis:
- Difficulty concentrating
- Depressed mood or mood disorders
- Sleeping too much or not enough
- Anxiety
- Suspiciousness
- Withdrawal from family and friends
- Delusions
- Hallucinations
- Disorganized speech, such as switching topics erratically
- Depression
- Suicidal thoughts or actions

Early psychosis usually occurs as a gradual onset of symptoms. Experts sometimes refer to it as first-episode psychosis (FEP) and they characterize it as a time in which someone first shows signs of beginning to lose contact with reality. Early warning signs can be difficult to distinguish from normal young adult behavior which is why it is important to see a health care provider if the condition is suspected. Some indicative signs of a psychotic episode are:
- Seeing, hearing, tasting, or believing things that others don’t
- Repeated, unusual thoughts or beliefs that can’t be stopped regardless of what others believe
- Strong and inappropriate emotions or no emotions at all
- Withdrawing from family or friends
- A sudden decline in self-care
- Trouble thinking clearly or concentrating
Not every person with psychosis develops the same symptoms, and the symptoms in one person can vary over time.
Diagnosis
There is no test to diagnose psychosis positively. However, a doctor will normally ask about symptoms and possible causes. Questions may focus on the person’s experiences, family history of psychiatric illness, and medicinal and recreational drug use. They may also do additional lab and imaging tests to rule out other factors. Blood tests and brain imaging (such as MRI scans) are common tests when diagnosing psychosis.
If there is no physical reason for the symptoms, a doctor may refer the patient to a psychiatrist or psychologist. These mental health professionals can determine if a mental health condition causes the observed symptoms by performing a psychological evaluation that includes a specially designed interview and assessment tools.
The sooner doctors diagnose and treat the condition, the better the ultimate prognosis becomes.
Treatment
The exact treatment for psychosis depends on the underlying disease. Common forms of treatment include antipsychotics and psychotherapy.
Antipsychotics
These drugs alleviate the symptoms but do not cure the disease. They are the main form of treatment for people with a psychotic illness and work by blocking dopamine. Examples of medications include:
- haloperidol (Haldol)
- chlorpromazine (Thorazine)
- clozapine (Clozaril)
Not all patients should use antipsychotics. They can often negatively interfere with other conditions, such as epilepsy or heart disease. Antipsychotics can reduce anxiety rather quickly but may take several days or weeks to reduce psychotic symptoms, such as hallucinations and delusions.
Some patients take antipsychotics orally, while others take them as administered injections. Several slow-release medications delivered via injection only need to be taken every 1 to 4 weeks.
Like many medications, side effects differ among patients. Some common side effects from antipsychotics include:
- drowsiness
- shaking and trembling
- weight gain
- restlessness
- muscle twitches and spasms – where your muscles shorten tightly and painfully
- blurred vision
- dizziness
- constipation
- loss of sex drive (libido)
- dry mouth
Always consult a doctor before stopping medication such as antipsychotics as suddenly stopping a prescription may result in a relapse of symptoms.
Psychotherapy
These treatments do not reduce the primary symptoms of psychosis but can help reduce the intensity and anxiety experienced by patients. Cognitive-behavioral therapy (CBT) and family intervention are common approaches to help patients and their families treat the symptoms of psychosis.
While psychosis symptoms may make everyday activities difficult and pose serious health risks, these mental disorders are treatable. Most people have a good recovery with treatment (especially with early intervention) and close follow-up care. When treated early, many people do not continue to have psychotic episodes and live productive lives.
More information on psychosis can be found at the National Library of Medicine. Read more in our other articles about schizophrenia.
If you liked this article, you can find more posts like this in the Nebula Research Library, including some on other behavior conditions like Tourettes.
June 21, 2022
