Table of contents
Nebula Genomics DNA Report for Epilepsy
Is epilepsy genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of May 2021. |
What is Epilepsy?
Epilepsy, sometimes referred to as cerebral seizure disorder or cerebral spasm disorder, refers to a brain disorder with at least one spontaneously occurring epileptic seizure. There is currently no existing identifiable cause (such as an acute inflammation of the brain, a stroke, or brain injury/head injury) or trigger (such as withdrawal of alcohol in the case of existing alcohol dependency or massive sleep deprivation).
Epilepsy is a chronic disorder that can be diagnosed when unprovoked seizures occur at a recognizably high risk of recurrence. The condition is characterized by unpredictable seizures and can cause other health problems. It is also known as a spectrum condition with a wide range of seizure types and control varying from person to person.
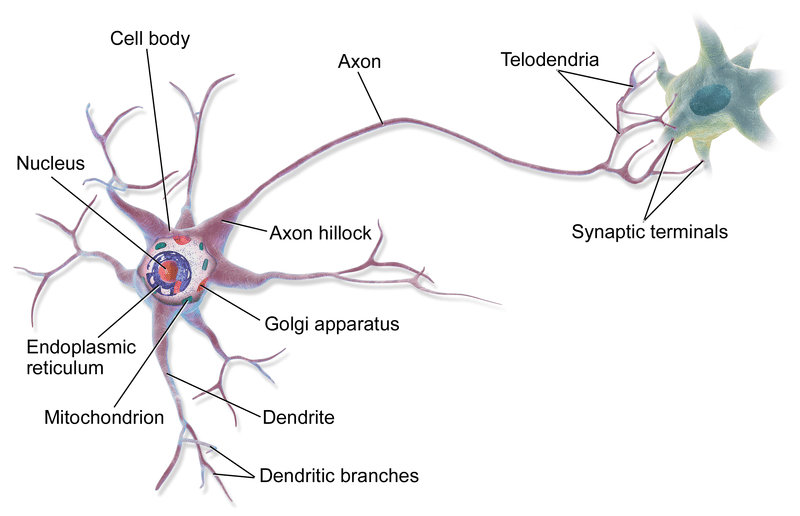
Biologically, an epileptic seizure is a consequence of sudden, synchronous electrical discharges of nerve cells (neuron groups) in the brain, which lead to stereotypical involuntary movement or mental health disorders. The exact activity in the brain can be unique. The location of the event, how it spreads, how much of the brain is affected, and how long it lasts all have profound effects.
For more information, the Epilepsy Foundation of America is a non-profit organization aimed to help people with the condition. The mission of the Epilepsy Foundation is “To lead the fight to overcome the challenges of living with epilepsy and to accelerate therapies to stop seizures, find cures, and save lives.” (copyright 2020) You can make a tax-deductible donation directly to the organization on their website and check their tax-exempt status. The website is also full of helpful information and resources.
Is Epilepsy Genetic?
Some types of epilepsy tend to run in families and are genetic conditions. To answer the question, “Is epilepsy hereditary?” not all epilepsies due to a genetic cause include a pattern of inheritance. Other types may be due to genetic changes that were inherited or happened for the first time in an individual. In the latter instance, there may not have been any family history.
In the case of cryptogenic epilepsy, there is no known cause for it, but brain imaging can help identify some lesions in the brain that led to its development. These represent about half of the cases. For some patients, it is not possible to determine the role of genetics in their seizures.
Is epilepsy inherited? Not all genetic epilepsy cases are inherited. If a person has a close family member with the disease, the risk of them developing the disorder by the age of 40 is less than 1 in 20. However, there is an increased risk of epilepsy if the first-degree relative has a generalized epilepsy form rather than focal.
Autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE) is an uncommon form of epilepsy that runs in families. Patients typically experience seizures at night during sleep.
The first few epilepsy-related genes were identified in the late 1990s. Advances in DNA sequencing now have identified hundreds of genes that play a role in epilepsy.
Some of these genes associated with epilepsy disorder include ALDH7A4, DEPDC5, EPM2A, GABARG2, GRIN2A, KCNQ2, LGI1, PCDH19, POLG, SCN1A, and STXBP1.
In addition, epilepsy can also occur in diseases based on a change in the genetic make-up. In these cases, the seizure is only a symptom of the disease. Examples are tuberous sclerosis or Angelman syndrome.
Current Research on Epilepsy
In 2016, the Genetics Commission of the International League Against Epilepsy published an article about the building blocks of epilepsy genetics. This was the first part of a primer of the Genetic Literacy Series. The primer part 2 came two years later and is an application of the principles discussed in Part 1. These studies offer a deep understanding of genetic variation, inheritance patterns, and how they are associated with developing the disorder.
This interesting study from 2017 assesses the psychological treatments for people with the condition. Essentially, it studies how these treatments improve a patient’s health-related quality of life (HRQoL) and provides recommendations and research designs. You may want to look at these other articles published that same year; one about the evidence for cannabis and cannabinoids for treating the condition (study conducted in 2017 and published the following year) and the other on the effects of yoga.
In 2018, FDA approved the first drug composed of an active ingredient derived from cannabis to treat severe forms of epilepsy. The antiepileptic drug Epidiolex is now used to treat Lennox-Gastaut syndrome and Dravet syndrome.
In February 2020, a paper was published in Epilepsy Research on the “Effects of seizure frequency, depression and generalized anxiety on suicidal tendency in people with epilepsy.”
About the COVID-19 pandemic, two exciting studies were published in 2020. One of them deals with how effectively a form of child epilepsy known as West syndrome was treated during hospital overflow during coronavirus patients. Then an article published in June studies the higher risk that epilepsy patients on immunosuppressive medications face.
Research in 2021 has shown that de novo seizures may occur in people infected with COVID-19.
Epidemiology
According to the CDC, in 2015, 1.2% of the US population (3.4 million people) had active forms of the condition. This number includes 3 million adults and 470,000 children with epilepsy.
An individual 18 or older is considered to have active epilepsy if a certified physician made the diagnosis. The patient reports a history of epilepsy or seizure disorder and is under treatment. They also have had one or more seizures in the past year.
A child aged 17 years or younger has active epilepsy if their parent or guardian reports that a doctor or health care provider has ever told them that their child had the condition and if their child currently has epilepsy or seizure disorder.
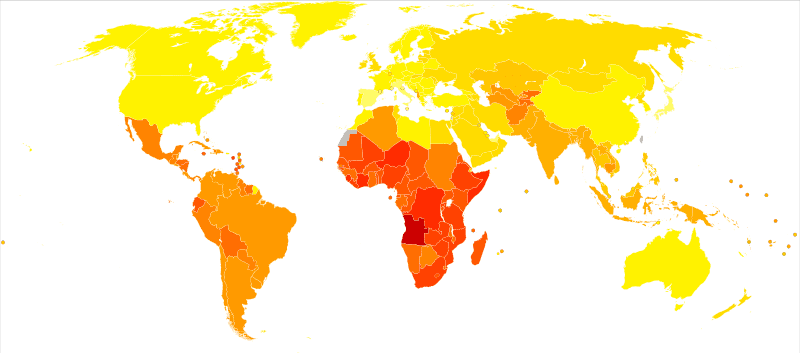
The condition affects both males and females of all races, ethnic backgrounds, and ages. A seizure article from 2018 reports that about 80% of patients live in low-middle income countries (LMIC), and 75% do not receive any treatment.
Symptoms
Seizures are a hallmark of this common neurological disorder. Seizure symptoms can vary significantly between individuals, although most patients living with it tend to have the same types of seizures. Usually, for a condition to be diagnosed as epilepsy, an individual has at least two unprovoked seizures.
Mayo Clinic notes the most common symptoms of seizures:
- Temporary confusion
- A staring spell
- Uncontrollable jerking movements of the arms and legs
- Loss of consciousness or awareness
- Psychic symptoms such as fear, anxiety, or deja vu
Forms of the condition may appear as one of two types of seizures, focal or generalized.
Focal seizures
Focal seizures originate in one portion of the brain. They may occur without loss of consciousness, where the patient experiences altered emotions or changes the way things look, smell, feel, taste or sound. They may also experience involuntary jerking of a body part, such as an arm or leg, and spontaneous sensory symptoms such as tingling, dizziness, and flashing lights. Focal epilepsy seizures can also occur with impaired awareness where the individual either loses consciousness or behaves strangely with their environment, such as staring blankly.
Generalized seizures
Generalized seizures affect the entire brain. They are classified into six categories:
- Absence seizures often occur in children and are characterized by staring into space or subtle body movements such as eye blinking or lip-smacking.
- Tonic seizures cause stiffening of your muscles.
- Atonic seizures cause a loss of muscle control, which may cause you to collapse or fall suddenly.
- Clonic seizures often include repeated or rhythmic jerking muscle movements. These seizures usually affect the face, neck, and arms.
- Myoclonic seizures are usually brief shock-like jerks in the muscles of the arms and legs.
- Tonic-clonic seizures, also known as grand mal seizures, are the most dramatic type of epileptic seizure and can cause an abrupt loss of consciousness, body stiffening and shaking, and sometimes loss of bladder control or tongue-biting.
A patient may experience a single seizure, partial seizures, or status epilepticus, which is a type that lasts more than 5 minutes or several within that time frame.
Epilepsy Causes
Although knowledge about the development of this disorder has increased significantly in recent decades, much is still unknown. The occurrence of epileptic seizures is caused by the over-excitability of nerve cells and abnormal brain electrical activity of larger nerve cell assemblies. Therefore, it is assumed that an imbalance of excitation and inhibition in these neural networks leads to epileptic seizures and is what causes epilepsy. About 3 out of 10 people who develop epilepsy have a change in their brain structure, causing the electrical storms of attacks.
Increased excitation or decreased inhibition of brain cells can be caused both by changes in the membrane properties of the nerve stimulator cells and in the transmission of excitation from nerve cell to nerve cell by neurotransmitters. For example, defects in the ion channels for sodium and calcium ions can participate in generating seizure discharges.
Often, the types of seizures are associated with the age of the patient. The Epilepsy Foundation summarizes what triggers attacks in patients of various ages:
Newborns may have seizures due to prenatal factors such as brain malformations, lack of oxygen during birth, low levels of blood sugar, electrolyte problems such as blood magnesium and blood calcium, inborn errors of metabolism, intracranial hemorrhage, and maternal drug use. Infants and children are most susceptible to fever, brain tumor (rarely), or infections (scarring in the brain).
Children and young adult seizures are most commonly brought on by congenital conditions (Angelman’s syndrome; Down’s syndrome; tuberous sclerosis and neurofibromatosis), genetic factors, progressive brain disease (rare), or environmental factors such as head trauma. Brain damage can occur at any age but is most prevalent and serious in young adults. In seniors, stroke, Alzheimer’s disease (you can read more about the genetics of Alzheimer’s disease and dementia in our Research Library), or trauma is most likely the cause.
Diagnosis
For diagnosis, the medical history of people who have had a seizure is taken. Doctors try to understand if the event was, in fact, an actual seizure, if it was caused by epilepsy and the type of seizures that are occurring.
Patients are also asked about family history of epilepsy, other diseases of the nervous system, and previous illnesses that may cause symptomatic epilepsy. These include disorders and increased risk to women with epilepsy during pregnancy, problems during childbirth leading to oxygen deficiency, accidents with craniocerebral trauma (brain conditions), or inflammatory diseases of the central nervous system.
This is followed by a physical examination, especially of the nervous system, with an assessment of strength, feeling (sensitivity), reflexes, cranial nerve function, balance, and coordination.
Blood tests are also used to identify possible causes of symptomatic epileptic seizures (such as hypoglycemia or mineral deficiency). They also test for signs of kidney or liver malfunction and other common problems. A lumbar puncture (sometimes called a spinal tap) may be used to rule out infections, like meningitis and encephalitis, and a toxicology screen may be used to look for toxins.
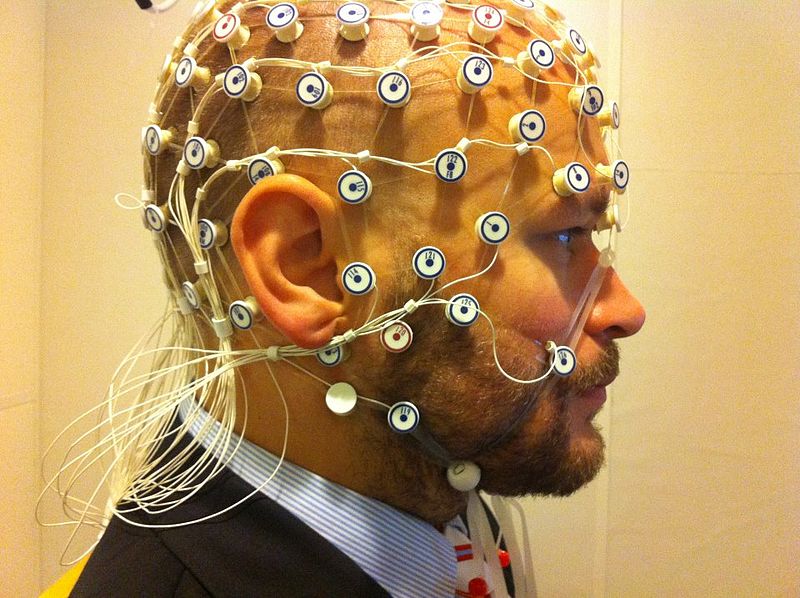
Typically, an electroencephalogram is performed. Imaging is usually part of routine diagnostics, while more specialized procedures are reserved for special questions.
Electroencephalogram (EEG)
This is the most common test for people living with epilepsy. A computer records the electrical activity in the brain. The EEG of a person with epilepsy may show abnormal spikes or waves in the brain’s electrical activity patterns. Unfortunately, this test is not always conclusive because many patients have normal EEGs in between seizures.
Imaging tests
An MRI and a CT scan are imaging tests that allow a doctor to view the brain. The scans can show scar tissue, tumors, or structural problems in the brain that may cause seizures or epilepsy. Imaging tests may not be done after a first seizure, but they are recommended in many situations, such as head injury.
Treatment
Treatment of epilepsy initially consists of the administration of drugs that control seizures (anticonvulsants). In therapy-resistant cases, other methods such as epilepsy surgery are also used. Epilepsy has a variety of effects on the affected person’s daily life (such as suitability for certain professions or driving a car), which must also be considered in the treatment.
Medications
Most people can reduce the incidence of epilepsy and severity of seizures with anti-epileptic medications. Some people see a stop in episodes completely. Many people can eventually discontinue medicines in the absence of symptoms.
You should always consult your doctor before stopping any seizure medication. Usually, epilepsy medications are started at a low dose and increased gradually.
You should notify your doctor immediately if you notice new or increased feelings of depression, suicidal thoughts, or unusual changes in your mood or behaviors. Tell your doctor if you have migraines, as they may prescribe one of the anti-epileptic medications that can prevent your migraines and treat epilepsy.
Some common side effects include:
- Fatigue
- Dizziness
- Weight gain
- Loss of bone density
- Skin rashes
- Loss of coordination
- Speech problems
- Memory and thinking problems
More-severe but rare side effects include:
- Depression
- Suicidal thoughts and behaviors
- Severe rash
- Inflammation of certain organs, such as your liver (Did you know you can test inflammation markers at home? Learn more in our article about at home inflammation tests).
In many cases, these medications are very effective, and patients become seizure-free.
Epilepsy Surgery
When medications fail to provide adequate control over recurrent seizures, surgery may be an option. In this surgery, a surgeon removes the area of the brain that’s causing seizures.
You may be a candidate for surgery if the seizures originate in a small, well-defined area of your brain. The site in the brain to be operated must not interfere with vital functions such as speech, language, motor function, vision, or hearing.
Oftentimes, patients who have surgery can then take a reduced amount of medications. In a small number of cases, surgery for epilepsy can cause complications such as permanently altering your cognitive abilities.
Alternative therapies
Other potential therapies to treat seizures have been used with various degrees of success. These options include:
- Vagus nerve stimulation (a device similar to a pacemaker)
- Ketogenic diet (You should consult a doctor if you or your child is considering a special diet as the patient may become malnourished if not eating correctly. Supervision by a nutritionist is best)
- Deep brain stimulation (implanted electrodes in the brain)
The United States National Institute of Neurological Disorders and Stroke has many resources for patients, as well as the Center for Disease Control and Prevention. You may also want to check out the International League Against Epilepsy (ILAE).
If you liked this article, you should check out our other posts in the Nebula Research Library!
July 9, 2022
