Table of contents
Nebula Genomics DNA Report for Alcoholism
Is alcoholism genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!
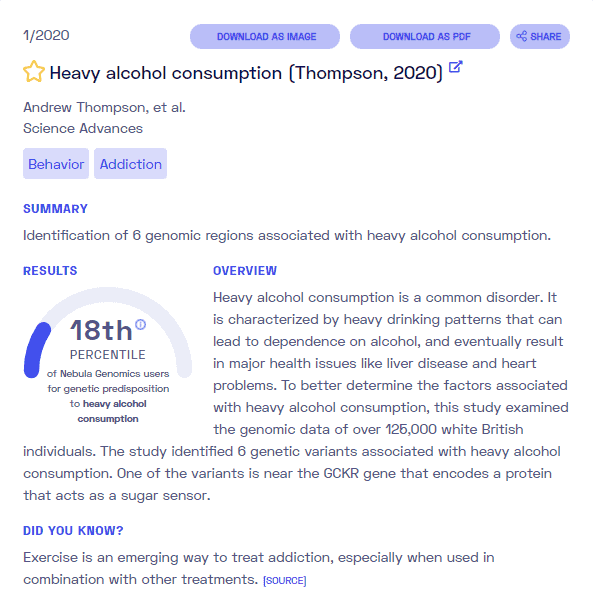
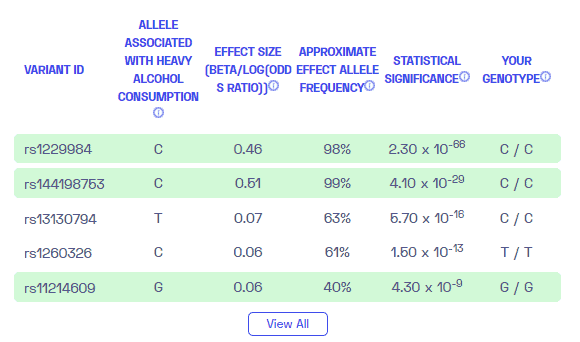
To learn more about how Nebula Genomics reports genetic variants in the table above, check out the Nebula Research Library Tutorial.
| This information has been updated to reflect recent scientific research as of May 2021. |
What is Alcoholism?
Patients experience typical symptoms that include:
- Progressive loss of control over drinking behavior up to compulsive alcohol consumption
- Neglect of former interests in favor of drinking, denial of addictive behavior
- Reduced withdrawal symptoms when consuming alcohol
- Tolerance to the substance
- Personality changes.
The number of people suffering from alcoholism and the resulting social and economic consequential damage is often higher in absolute figures in Europe and the USA than for other drugs.

Alcoholism can feel like a prison to those who suffer from it. Wikipedia CC–Attribution-Share Alike 4.0 International
In 1849, the Swedish physician Magnus Huss was the first to define excessive drinking as a disease. He distinguished between “acute alcoholic disease or intoxication” and “alcoholismus chronicus.” However, this recognition did not prevail for a long time. Elvin Morton Jellinek, who worked for the World Health Organization (WHO), gained worldwide acceptance in 1951 with his view, inspired by his work with Alcoholics Anonymous, that the condition was a disease.
Is Alcoholism Genetic?
A 2008 study conducted by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (a section of the National Institutes of Health) reviewed much of the research on this condition and genetics. The study concluded that genetic factors account for 40-60 percent of the variance among people who have a problem with alcoholism. Since then, scientists have identified some specific genes that contribute to a genetic predisposition to alcohol abuse.
Potential alcoholism genes
Some genes playing a role in the condition correlate with the development of reward. That is, a predisposition to metabolize the substance in such a way that the pleasurable effects are more prominent than adverse effects such as nausea and headaches increases a person’s risk of developing an alcohol use disorder.
For instance, gamma-aminobutyric acid (GABA) is a neurotransmitter that decreases certain brain signals and drops your nervous system activity. Experts associate the gene responsible for the movement of this amino acid with a higher risk of alcoholism.
Another genetic factor for alcoholism may be an association of a variant of the DRD2 gene, which affects the neurotransmitter dopamine. The brain releases dopamine in greater quantities when drinking and lifts the mood, activating the brain’s reward system.
So, “can alcoholism be inherited?” is probably not the right question due to its complexity.
Genetic differences in tolerance or liver degradation capacity can also genetically influence the condition. These include, for example, the enzyme alcohol dehydrogenase.
In some people, a variant with reduced activity is present, resulting in more severe symptoms of intoxication. This makes dependence less likely. On the other hand, people who can tolerate comparatively large amounts of alcohol are at risk of becoming dependent in the long term, suggesting a genetic predisposition.
Experts believe that they have associated an alteration of the MAOA gene with this condition, as well as substance abuse and antisocial behavior.
Learn more about hereditary alcoholism, including the latest research on genetic variants, from the Delphi Behavioral Health Group.
Current Research on Genetic Alcoholism
This condition has been present in human history since men learned to ferment fruit – which is about 10 million years ago. More recently, studies have shown that the condition may be related to genetics. For example, this study from 2013 makes a strong case for genetic predisposition.
Studies about the relationship between alcoholism and genetics go back over 80 years. Today, we have made tremendous progress learning that there is no “alcoholism gene” but genetic markers that accentuate dependence.
The Genetics of Alcoholism studies have seen progress in their search for the genetic variants that affect dependence and addiction risk. Researcher have conducted several methods, including an analysis of whole genome-transcriptomic organization in brain to identify genes associated with alcoholism.
This paper identified risk loci (positions in the chromosome), in 2019, with shared effects on alcoholism, heroin, and methamphetamine dependence.
A interesting study from 2020 involved the fruit fly, where it was used as a tractable model for AUD.
Finally, a well-documented article seems to have found that alcoholism is a risk factor for COVID 19. The work analyzes the relationship between SARS-CoV-2 and alcoholism.
Research on addiction science, prevention, and treatment are a large focus of the National Institute on Drug Abuse, which provides funding to support research. This includes the genetic connection with alcoholism.
Epidemiology
According to the World Health Organization, worldwide drinking patterns vary across countries. In 2017, binge drinking had the highest reported prevalence in Europe overall, with Eastern European countries, France, and England reporting some of the highest rates of binge drinking.
In the United States, the prevalence of any drinking in 12 months in 2012 rose from approximately 65% to just over 72%. Scientists most highly observe this increase in women, rural citizens, those with lower socioeconomic status, and minorities. From 2001 – 2012, the condition increased by 50%, and this increase was more pronounced in women, rising 80% over the time frame. In 2020, one estimate suggested that as many as 18 million adults in the country struggle with alcohol addiction.
Worldwide, the ratio of men to women who drink alcohol is 3.8, with 54% of men and 32% of women reporting being drinkers. However, women are starting to experience an increase.
As reported in the World Mental Health Surveys in 2020, 15% of all lifetime alcohol use disorder (AUD) cases occurred by the time the individual turned 18. People with higher financial status, older at the time of the interview, married, and with a higher educational level presented a lower risk for lifetime alcoholism.
Symptoms
The course of alcohol disease is not uniform and symptoms range from mild to severe.
According to WebMD, the condition is a chronic, relapsing brain disease that includes:
- Compulsive drinking
- Loss of control when it relates to drinking
- A noticeable bad mood when not drinking
The disease can begin with regular consumption of small amounts, and people may be oblivious to frequent intoxication. It is not always noticeable from the outside.
If the affected person can function, doctors often refer to them as a functioning alcoholic. The disease often progresses relatively inconspicuously and slowly, usually over several years. Sufferers can be unaware of the severity of their illness and may deny it altogether.
Additionally, the disease isn’t just about how much you drink. It’s also about:
- How often you drink
- What the effects are
- What happens when you try to cut back

At first, the earliest stages may include:
- Drinking more than planned
- Continuing to drink despite concerns from others
- Frequent attempts to cut down on or quit drinking
As the disease progresses, an individual will usually need to consume larger quantities to get the desired effect. If it is not available, the individual may go through withdrawal syndrome.
In the next stage, blackouts and loss of control may occur. Personality changes and additional physical effects begin to show.
This progression, continuing until the individual hits the bottom with excessive drinking and then moves back up to rehabilitation, is called the Jellinek curve.
E. Morton Jellinek, a pioneer in the study of alcohol abuse and dependence, suggested the “progressive phases of alcoholism.” It came to be known as the Jellinek curve in 1950 and is still widely used today with modifications.
Alcohol withdrawal syndrome
When patients reduce or abruptly stop heavy drinking they may experience a withdrawal syndrome. Severe to life-threatening withdrawal symptoms may occur. Withdrawal symptoms include nausea, nervousness, sleep disturbances, the strong urge to drink (“binge drinking”), irritability, and depression. If the patient already has advanced physical dependence they may also experience heavy sweating, trembling (especially of the hands), flu-like symptoms, and – in extremely bad cases – seizures with tongue biting and hallucinations.
Personality changes
The change in character varies among dependent individuals. In addition to significant memory loss, concentration, drive and attention, a frequent occurrence of jealousy mania is noticeable. Affected are mainly the reaction patterns to everyday stresses and conflicts, as a result of which the overall personality appears unharmonious-differentiated. Depression can also occur.
As a consequence of long-term alcoholism, psychotic substance use disorders also occur, which were not present before. In addition, people may strongly narrow their interests to addiction while neglecting previous activities, as well as personal hygiene and care. Very problematic is the often increased aggressiveness and propensity to violence. The change in character also includes a tendency to deny or trivialize the disease.
Physical effects
Someone who drinks excessively tends to have an average 20-year shorter life expectancy. Long-term abuse often causes (sometimes chronic) secondary health problems:
- Malignant tumors
- Liver disease
- Pancreas
- Damaged muscles
- Alcoholic myopathy
- Metabolic disorders
- Cardiovascular disorders
- Gastrointestinal issues
- Nervous system and neurological disorders
Causes
Research currently suggests that the genetic component tends to explain only about half of the risk. They believe the other half is influenced by environmental factors and interpersonal factors (e.g., cultural attitudes, availability, expectations about the effects of alcohol on mood and behavior, personal experiences with the substance, and stress).
In a twin study, researchers found that twins adopted by families with drinking problems were slightly more likely to abuse the substance themselves. However, the chance of alcoholism was much higher if the twins’ biological father suffered from it, whether alcohol was present in the adoptive families or not. Generally, children of alcoholics are more likely to abuse it themselves.
Other Factors
Children of addicted parents are more likely to become addicted than other children. Physical, psychological, and sexual violence combined with addiction in the family of origin are significant risk factors. Physically, doctors have seen adolescents with a family history of alcoholism to have a smaller amygdala (emotional center in the brain) that may affect substance-based cravings.
Starting to drink at an early age and mental illnesses such as anxiety, depression, bipolar disorder, ADHD, and schizophrenia, also put an individual at a higher risk of developing the condition.
Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides eleven criteria, of which at least two must be present over twelve months for an alcoholism diagnosis. Most clinicians use the term “alcohol use disorder” to help emphasize the disease value of the disorder and reduce inhibitions to seek medical help.
DSM-5
- Alcohol is consumed in greater quantities or for longer than intended
- Persistent desire or unsuccessful attempts to reduce or control consumption
- High time expenditure to obtain or consume the substance or to recover from its effects
- Craving or a strong desire to drink
- Repeated use that results in failure to fulfill essential responsibilities at work, school, or home
- Continued use despite ongoing or repeated interpersonal problems caused or worsened by the effects
- Important social, occupational, or recreational activities are abandoned or curtailed because of use.
- Repeated consumption in situations where consumption results in physical danger
- Continued use despite knowledge of a persistent or recurring physical or psychological problem that is likely caused or exacerbated by drinking
- Development of alcohol tolerance, defined by any of the following:
- Desire for marked increases in dose to bring about a state of intoxication or the desired effect
- Markedly diminished effect with continued consumption of the same amount
- Withdrawal symptoms manifested by any of the following:
- Characteristic withdrawal syndrome related to alcohol
- Drinking (or a very similar substance, such as benzodiazepines) is used to relieve or avoid withdrawal symptoms
The condition can be divided into three severity levels (mild, moderate, severe):
- Mild: meeting 2-3 symptom criteria
- Medium: meeting 4-5 symptom criteria
- Severe: meeting 6 or more symptom criteria
Most individuals or family members eventually notice the common signs of alcoholism without physician intervention. Self-tests from support and counseling centers may be helpful at this point.
Treatment
Speaking with a medical physician is a first step towards alcohol treatment. A physician can tell you if you need assistance, work with you to put together a plan of treatment for alcohol abuse, possibly including medication, and/or refer you to a support group, counseling, or treatment center.
If the condition is serious, attempts to stop drinking very suddenly may lead to severe complications, including withdrawal syndrome and seizures. Some individuals may need to reduce drinking in a hospital or rehabilitation setting to manage acute withdrawal medically. After detox, an individual may choose to attend either residential treatment facilities or outpatient treatment programs.
Both types of treatment programs tend to prioritize the following approaches:
- Behavioral therapy, including cognitive-behavioral therapy (CBT) and motivational enhancement
- Family therapy
- Treatment for dual diagnosis (i.e., depression)
- 12-step or other mutual support group meetings
Sometimes, medication may be recommended to reduce cravings and reduce the chances of relapsing into dangerous drinking for long-term treatment.
- Campral (acamprosate) acts on the GABA and glutamate neurotransmitter systems. It helps to control the insomnia, anxiety, and restlessness that often accompany withdrawal.
- Disulfiram (Antabuse) deters drinking in patients highly motivated to quit. If a person takes disulfiram and then drinks, the result is flushing, nausea, and heart palpitations.
- Naltrexone acts on the opioid receptors in the brain to block the reward of drinking and potentially reduce cravings.
- Topiramate is sometimes used off-label to help decrease continued drinking behavior in those recovering from alcohol misuse.
If you or someone you know is in need of help, you should consider calling the SAMHSA’s national helpline: 1-800-662-HELP (4357).
If you liked this article, you should check out our other posts in the Nebula Research Library!
You may also be interested in reviews for prescription antidepressants, such as Lexapro and Zoloft.
June 22, 2022
