Table of contents
- Nebula Genomics DNA Report for Hyperthyroidism
- What is hyperthyroidism? (Part 1 of Is hyperthyroidism genetic?)
- Is Hyperthyroidism Genetic?
- Current Research on Hyperthyroidism [Updated June 2021]
- Epidemiology (Part 4 of Is hyperthyroidism genetic?)
- Hyperthyroidism Symptoms (Part 5 of Is hyperthyroidism genetic?)
- Hyperthyroidism Causes (Part 6 of Is hyperthyroidism genetic?)
- Diagnosis (Part 7 of Is hyperthyroidism genetic?)
- Treatment (Part 8 of Is hyperthyroidism genetic?)
Nebula Genomics DNA Report for Hyperthyroidism
Is hyperthyroidism genetic? We created a DNA report based on a study that attempted to answer this question. Below you can see a SAMPLE DNA report. To get your personalized DNA report, purchase our Whole Genome Sequencing!

| This information has been updated to reflect recent scientific research as of June 2021 |
What is hyperthyroidism? (Part 1 of Is hyperthyroidism genetic?)
The thyroid gland is a hormonal gland in vertebrates. In mammals, it is located on the neck below the larynx in front of the trachea. In humans, it has the shape of a butterfly and consists of two lobes connected by a narrow bridge called the isthmus.
The primary function of the thyroid gland is the storage of iodine and the formation of the iodine-containing thyroid hormones triiodothyronine and thyroxine, as well as the peptide hormone calcitonin. The iodine-containing thyroid hormones play an important role in energy metabolism, growth and development, body temperature, heart rate, menstrual cycles, and weight.
The thyroid gland is the starting point for numerous diseases, which, among other things, can lead to disturbances in hormone metabolism and cause either hypothyroidism or hyperthyroidism. Hyperthyroidism occurs when the thyroid gland outputs too much of the hormone thyroxine, leading to accelerated metabolism and irregular heartbeat. Hypothyroidism is when the gland does not make enough hormones to support wellbeing.
Is Hyperthyroidism Genetic?
Graves’ disease, the most common form of hyperthyroidism, is known to have a hereditary component, suggesting that genes play a role in the condition. As an autoimmune disease, it results from the body’s immune system attacking its own cells. But are thyroid problems genetic?
Possible genetic risk factors contributing to Graves’ disease include genes in a family called the human leukocyte antigen (HLA) complex. This complex helps the immune system distinguish its own proteins from those of outside sources (like viruses). Due to its nature, any genes involved with the immune system (such as the PTPN22 gene involved in the functioning of T cells) or with thyroid function (such as the TG gene that contributes to the release of thyroid hormones and the TSHR gene that codes a receptor that binds to TSH) may also play a role. Although several genes have been associated with the condition, it is thought that each individual gene plays only a small part in disease development.
Current Research on Hyperthyroidism [Updated June 2021]
Research on hyperthyroidism in recent years has sought to find better treatments to improve patients’ life quality. To do this, we need to understand better how thyroid hormones work in the body. This 2017 study taps into hyperthyroidism and developmental dysfunction, for instance.
In November 2019, Pediatrics released this interesting study about the correlation between mental health conditions and hyperthyroidism. They discovered, among other things, a higher rate of suicidality in mental health patients with hyperthyroidism than those who were not diagnosed with hyperthyroidism.
Hyperthyroidism is known to cause changes in cognitive function. In this study from 2018, researchers try to find the effect of hyperthyroidism on reaction time using the oddball paradigm.
As we saw earlier, Graves disease is the most common cause of hyperthyroidism. If you would like to learn more about the road toward ultimate care for Graves’ hyperthyroidism, this PDF has insightful information about the proper direction to take.
Epidemiology (Part 4 of Is hyperthyroidism genetic?)
According to the American Thyroid Association, more than 12% of the U.S. population will develop some form of thyroid condition in their lifetime. Up to 60% of those with a thyroid condition are undiagnosed. Regarding hyperthyroidism and hypothyroidism, 1.2% of the worldwide population experiences hypothyroidism while 5% experience hyperthyroidism.
Women are five to eight times more likely to develop one of these conditions in their lifetime, with 1 in 8 women experiencing it.
Hyperthyroidism Symptoms (Part 5 of Is hyperthyroidism genetic?)
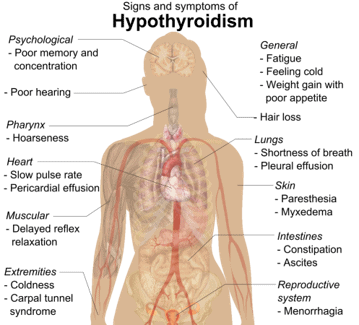
Both hypothyroidism and hyperthyroidism symptoms vary by the severity of the hormone imbalance. Problems tend to start gradually before getting worse. In the case of hypothyroidism, your metabolism slows down, most noticeably causing fatigue and weight gain. Other common symptoms of this type of thyroid disease include:
- Fatigue
- Increased sensitivity to cold
- Constipation
- Dry skin
- Weight gain
- Puffy face
- Hoarseness
- Muscle weakness
- Elevated blood cholesterol level
- Muscle aches, tenderness, and stiffness
- Pain, stiffness, or swelling in your joints
- Heavier than usual or irregular menstrual periods
- Thinning hair
- Slowed heart rate
- Depression
- Impaired memory
- Enlarged thyroid gland (goiter)
In the opposite case, hyperthyroidism will accelerate the metabolism, causing unintended weight loss and rapid or irregular heart rate. In addition, because the varying amount of hormone is carried to every part of the body, other symptoms are related to many of the body’s systems speeding up.
The condition can mimic other problems, which makes it hard to diagnose. Some of the more common symptoms include:
- Increased appetite
- Nervousness, anxiety, and irritability
- Tremor — usually a light trembling in your hands and fingers
- Sweating
- Changes in the menstrual cycle
- Increased sensitivity to heat
- More frequent bowel movements
- Goiter (enlarged thyroid gland)
- Fatigue
- Muscle weakness
- Difficulty sleeping
- Skin thinning
- Fine, brittle hair
Patients may find that they initially have a lot of energy due to the increased metabolism. However, as the body breaks down, they will eventually feel tired more often.
Hyperthyroidism Causes (Part 6 of Is hyperthyroidism genetic?)
Graves’ disease
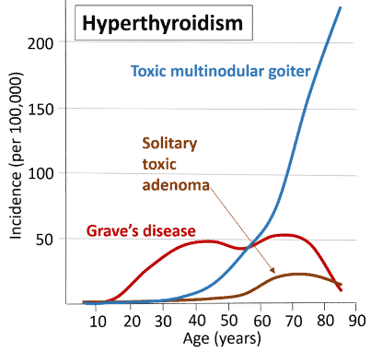
There are several hyperthyroidism causes. The most common condition (contributing to 70% of all cases) that results in hyperthyroidism is Graves’ disease, an autoimmune disorder in which the body produces an antibody that stimulates the overproduction of thyroid hormones by the thyroid gland.
Given all these facts, how common is hyperthyroidism? It is more common in women than in men, and onset often occurs in early adulthood, although symptoms can appear at any time. Symptoms are particularly noticeable in older adults.
Although the cause and Grave’s disease genetic influence is unknown, it is known to run in families, suggesting a hereditary and genetic component.
Graves’ disease has a number of hallmark symptoms, such as eye abnormalities, known as Graves ophthalmopathy. This eye disease causes swelling and inflammation, redness, dryness, puffy eyelids, and a gritty sensation in the eyes. It may also lead to bulging eyes due to inflammation of the tissue and pulling back of the eyelids.
Graves’ ophthalmopathy is thought to be the result of a buildup of carbohydrates in the muscles and tissues behind the eyes as a result of the same antibodies that lead to increased hormone production also being attracted to these tissues. About 25 to 50 percent of patients experience this symptom as well as swelling at the front of the neck due to an enlarged thyroid.
People with Graves disease have an increased risk of developing other autoimmune disorders such as rheumatoid arthritis, pernicious anemia, systemic lupus erythematosus, Addison’s disease, celiac disease, type 1 diabetes, and vitiligo.
Other causes
Other than Graves disease, what can cause hyperthyroidism? Let’s try to answer this question below.
Toxic nodular or multinodular goiters are characterized by one or more nodules or lumps in the thyroid that may gradually grow and increase their activity so that the amount of thyroid hormone into the blood is greater than normal.
Another cause of hyperthyroidism is thyroiditis. This condition is caused by a problem with the immune system or a viral infection that causes the gland to leak stored thyroid hormone. You may also experience similar symptoms by taking too many thyroid hormone supplements. In these cases, the thyroid is not overactive, but there is too much thyroid hormone in the body, mimicking the symptoms of hyperthyroidism.
Overall, it is believed that hyperthyroidism resulting from Graves’ disease is caused by both environmental and genetic factors. What triggers hyperthyroidism? Some environmental factors are thought to trigger the condition in individuals already at risk. Some of these influences include sex hormones (particularly in women), viral or bacterial infections, certain medications, and having too much or too little iodine (a substance critical for thyroid hormone production).
Diagnosis (Part 7 of Is hyperthyroidism genetic?)
Your doctor will want to know your history of symptoms and conduct a physical exam to diagnose the condition. Since some of the signs are noticeable, like unintended weight loss and irregular menstrual cycles in women, it is recommended that you discuss thyroid concerns with your doctor, who can then order the necessary tests. The doctor may also feel your thyroid gland to check for enlargement and swelling.
Did you know you can check thyroid hormone levels at home? Learn more about at-home thyroid tests!
If a thyroid condition is suspected, your doctor will usually order initial blood tests.
Blood tests
Blood tests determine if you have abnormal levels of thyroid hormones in your blood, indicating that your thyroid may be producing too many or too few. The most common tests look for either thyroxine or TSH. High levels of thyroxine or low levels of TSH indicate an overactive thyroid.
You may get a false positive test if you are taking biotin – a B vitamin supplement present alone or in multivitamins. Therefore, it is usually advised that you stop taking biotin at least 12 hours before the test.
If the blood tests indicate hyperthyroidism, your doctor may order some additional tests to confirm the diagnosis.
Radioiodine uptake test
This test involves taking a small, oral dose of radioactive iodine and measuring its uptake in the thyroid at certain time points, usually four, six, and 24 hours. If iodine uptake is high, it is a good indication that your thyroid is producing too much thyroxine, a sign of either Graves’ disease or hyperfunctioning thyroid nodules. Conversely, if iodine uptake is low, this points to thyroxine leaking out of the thyroid gland, a more common sign of thyroiditis.
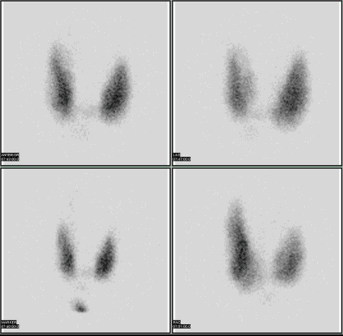
Thyroid scan
During this test, a radioactive isotope is administered intravenously. Next, your thyroid gland is scanned, and an image showing how the isotope is absorbed by the gland is observed on a computer screen.
Thyroid ultrasound
This test takes an image of the thyroid gland using ultrasound. It usually is better at diagnosing thyroid nodules than other tests and may be used if nodules are expected.
Treatment (Part 8 of Is hyperthyroidism genetic?)
According to the American Thyroid Association, the type of treatment for hyperthyroidism depends on your age, severity of the condition, and other health conditions. The first course of treatment is usually antithyroid drugs.
Medications
Antithyroid medicines work by blocking the thyroid’s ability to produce more hormones. The most commonly prescribed medication is methimazole (Tapazole®), as it tends to have the least amount of side effects. About 20–30% of patients with Graves’ disease saw remission after 12–18 months on these medications. The drugs do not work as effectively for patients with toxic nodular or multinodular goiter but may be used in preparation for a different treatment.
Side effects are rare, but reactions such as red skin rashes, hives, and occasionally fever and joint pains may occur in up to 5% of patients. In even fewer cases (0.2%), a rare side effect of lowered white blood cells may occur. This immune reaction can lead to reduced resistance to infection. A fever or sore throat is a sign that you will want to get your white blood cell count checked immediately. Stopping the medication will allow your white blood cell count to return to normal.
Radioactive iodine
Another approach to treat hyperthyroidism is to destroy some of the thyroid cells. In this case, the patient will orally swallow a safe amount of radioactive iodine that the thyroid cells then take up to make hormones as they do not distinguish between different forms of iodine. The radioactive version will kill the cells that take it up, shrinking the thyroid or thyroid nodules and reducing the produced hormone.
Sometimes, the hyperthyroid symptoms only decrease, at which a second dose of radioactive iodine may be used. In more cases, the patient acquires hypothyroidism (an underactive thyroid) which can then be treated with thyroid supplements.
This has been a standard treatment for over 60 years, and no link has been found between the radioactive iodine treatment and increases in cancer.
Surgery
Partial or complete thyroid gland removal via thyroid surgery will completely cure hyperthyroidism, although the surgery can be risky. Therefore, it is best to first get your thyroid under control with medication before going through surgery. Your surgeon may also ask you to take nonradioactive iodine before the surgery to limit blood supply to the thyroid.
Risks specific to this surgery include damage to the parathyroid glands that are next to the thyroid and control your body’s calcium levels, and damage to the nerves that control your vocal cords. However, these complications are rare, especially if the surgery is performed by an experienced surgeon.
As with radioactive iodine therapy, patients will experience long-term hypothyroidism after surgery and will need to take thyroid hormone supplements for the rest of their life.
All forms of medical care for this condition usually come with a prescription of beta-blockers that block the action of thyroid hormones. Although the hormone levels remain the same, these medications effectively counter the symptoms such high levels have on the body, such as increased heart rate, palpitations, shakes, and nervousness.
For more information on hyperthyroidism resources, you should check out the National Institute of Diabetes and Digestive and Kidney Diseases.
If you liked this article, you should check out our other posts in the Nebula Research Library!
July 5, 2021
